Successful Treatment of Chemotherapy Induced Hemorrhagic Cystitis with Intravesical Application of A Specific Product in n Ambulatory Setting
Article Information
Elisaveta Gerova1*, Jorg Humburg2
1Department of Gynecology, Bethesda Hospital Basel, Switzerland
2Department of Urogynecology Bethesda Hospital Basel, Switzerland
*Corresponding author: Elisaveta Gerova, Department of Gynecology, Bethesda Hospital Basel, Switzerland
Received: 20 May 2020; Accepted: 10 June 2020; Published: 19 June 2020
Citation:
Elisaveta Gerova, Jorg Humburg. Successful Treatment of Chemotherapy Induced Hemorrhagic Cystitis with Intravesical Application of A Specific Product in n Ambulatory Setting. Journal of Women’s Health and Development 3 (2020): 148-153.
View / Download Pdf Share at FacebookAbstract
Background and Aim: Hemorrhagic cystitis (HC) is an inflammation of the urinary bladder defined by signs of urinary bladder irritation and hematuria. It is thought that damage to the Glycosaminoglycan- (GAG) layer, which coats the uroepithelium and provides the initial barrier for physiological protection, may be the first step in its development. The disease can be triggered by chemotherapeutic drugs exposure and radiation therapy. The incidence rate of HC is predicted to rise substantially in the future as more aggressive treatments of cancer are implemented.
Case Presentation: A 53-year old female patient presented with persistent dysuria, frequent voiding and nocturia. At the time the patient received adjuvant chemotherapy for her breast cancer.
The patient presented with late-onset hemorrhagic cystitis after completing four cycles of chemotherapy. We treated her with intravesical instillations of hyaluronic acid and chondroitin sulphate in order to substitute the GAG layer.
The report’s primary aim is to present the significant effect of an intravesical application of a GAG layersubstitution product.
In our case report, we outline the indications as well as procedural steps of our approach and compare the results with those of other therapies and troubleshooting recommendations.
The treatment was held in an ambulatory setting, making it both cost-effective and lifestyle-friendly for our patient. To the best of our knowledge, the treatment as described has not yet been used in chemotherapy-induced HC.
Conclusions: This is the first report showing complete regression of haemorrhagic cystitis after inravesical application of a specific product. Prospective studies should evaluate if the treatment effect is reproducible and if this approach could be a useful profilactic measure as well as a
Keywords
Hemorrhagic cystitis; Hyaluronic acid; Chondroitin sulphate; Intravesical instillations; Dysuria; Frequent voiding; Nocturia
Hemorrhagic cystitis articles Hemorrhagic cystitis Research articles Hemorrhagic cystitis review articles Hemorrhagic cystitis PubMed articles Hemorrhagic cystitis PubMed Central articles Hemorrhagic cystitis 2023 articles Hemorrhagic cystitis 2024 articles Hemorrhagic cystitis Scopus articles Hemorrhagic cystitis impact factor journals Hemorrhagic cystitis Scopus journals Hemorrhagic cystitis PubMed journals Hemorrhagic cystitis medical journals Hemorrhagic cystitis free journals Hemorrhagic cystitis best journals Hemorrhagic cystitis top journals Hemorrhagic cystitis free medical journals Hemorrhagic cystitis famous journals Hemorrhagic cystitis Google Scholar indexed journals Hyaluronic acid articles Hyaluronic acid Research articles Hyaluronic acid review articles Hyaluronic acid PubMed articles Hyaluronic acid PubMed Central articles Hyaluronic acid 2023 articles Hyaluronic acid 2024 articles Hyaluronic acid Scopus articles Hyaluronic acid impact factor journals Hyaluronic acid Scopus journals Hyaluronic acid PubMed journals Hyaluronic acid medical journals Hyaluronic acid free journals Hyaluronic acid best journals Hyaluronic acid top journals Hyaluronic acid free medical journals Hyaluronic acid famous journals Hyaluronic acid Google Scholar indexed journals Chondroitin sulphate articles Chondroitin sulphate Research articles Chondroitin sulphate review articles Chondroitin sulphate PubMed articles Chondroitin sulphate PubMed Central articles Chondroitin sulphate 2023 articles Chondroitin sulphate 2024 articles Chondroitin sulphate Scopus articles Chondroitin sulphate impact factor journals Chondroitin sulphate Scopus journals Chondroitin sulphate PubMed journals Chondroitin sulphate medical journals Chondroitin sulphate free journals Chondroitin sulphate best journals Chondroitin sulphate top journals Chondroitin sulphate free medical journals Chondroitin sulphate famous journals Chondroitin sulphate Google Scholar indexed journals Intravesical instillations articles Intravesical instillations Research articles Intravesical instillations review articles Intravesical instillations PubMed articles Intravesical instillations PubMed Central articles Intravesical instillations 2023 articles Intravesical instillations 2024 articles Intravesical instillations Scopus articles Intravesical instillations impact factor journals Intravesical instillations Scopus journals Intravesical instillations PubMed journals Intravesical instillations medical journals Intravesical instillations free journals Intravesical instillations best journals Intravesical instillations top journals Intravesical instillations free medical journals Intravesical instillations famous journals Intravesical instillations Google Scholar indexed journals Dysuria articles Dysuria Research articles Dysuria review articles Dysuria PubMed articles Dysuria PubMed Central articles Dysuria 2023 articles Dysuria 2024 articles Dysuria Scopus articles Dysuria impact factor journals Dysuria Scopus journals Dysuria PubMed journals Dysuria medical journals Dysuria free journals Dysuria best journals Dysuria top journals Dysuria free medical journals Dysuria famous journals Dysuria Google Scholar indexed journals Frequent voiding articles Frequent voiding Research articles Frequent voiding review articles Frequent voiding PubMed articles Frequent voiding PubMed Central articles Frequent voiding 2023 articles Frequent voiding 2024 articles Frequent voiding Scopus articles Frequent voiding impact factor journals Frequent voiding Scopus journals Frequent voiding PubMed journals Frequent voiding medical journals Frequent voiding free journals Frequent voiding best journals Frequent voiding top journals Frequent voiding free medical journals Frequent voiding famous journals Frequent voiding Google Scholar indexed journals Nocturia articles Nocturia Research articles Nocturia review articles Nocturia PubMed articles Nocturia PubMed Central articles Nocturia 2023 articles Nocturia 2024 articles Nocturia Scopus articles Nocturia impact factor journals Nocturia Scopus journals Nocturia PubMed journals Nocturia medical journals Nocturia free journals Nocturia best journals Nocturia top journals Nocturia free medical journals Nocturia famous journals Nocturia Google Scholar indexed journals urinary articles urinary Research articles urinary review articles urinary PubMed articles urinary PubMed Central articles urinary 2023 articles urinary 2024 articles urinary Scopus articles urinary impact factor journals urinary Scopus journals urinary PubMed journals urinary medical journals urinary free journals urinary best journals urinary top journals urinary free medical journals urinary famous journals urinary Google Scholar indexed journals chemotherapeutic articles chemotherapeutic Research articles chemotherapeutic review articles chemotherapeutic PubMed articles chemotherapeutic PubMed Central articles chemotherapeutic 2023 articles chemotherapeutic 2024 articles chemotherapeutic Scopus articles chemotherapeutic impact factor journals chemotherapeutic Scopus journals chemotherapeutic PubMed journals chemotherapeutic medical journals chemotherapeutic free journals chemotherapeutic best journals chemotherapeutic top journals chemotherapeutic free medical journals chemotherapeutic famous journals chemotherapeutic Google Scholar indexed journals uroepithelium articles uroepithelium Research articles uroepithelium review articles uroepithelium PubMed articles uroepithelium PubMed Central articles uroepithelium 2023 articles uroepithelium 2024 articles uroepithelium Scopus articles uroepithelium impact factor journals uroepithelium Scopus journals uroepithelium PubMed journals uroepithelium medical journals uroepithelium free journals uroepithelium best journals uroepithelium top journals uroepithelium free medical journals uroepithelium famous journals uroepithelium Google Scholar indexed journals
Article Details
Introduction
Hemorrhagic cystitis (HC) is an inflammation of the urinary bladder defined by signs of urinary bladder irritation and hematuria. The disease can be triggered by chemotherapeutic drugs exposure and radiation therapy for instance. It is well documented after exposure to cyclophosphamide [1,2,3] and oxoamide [4,5]. As a preventive measure after exposure to these drugs patients would receive Mesna to protect the bladder. It is thought that damage to the Glycosaminoglycan- (GAG) layer, which coats the uroepithelium and provides the initial barrier for physiological protection, may be the first step in its development [6].
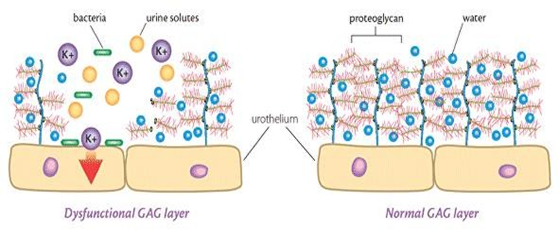
Figure 1: GAG layer (illustration adapted from The UK Bladder Infection Centre website)
The severity of HC can range from asymptomatic microhematuria to potentially life-threatening conditions such as the development of gross hematuria accompanied by clot formation, severe pain and occasionally uncontrollable bleeding, urinary tract obstruction and renal failure. In this latter setting, patients are extremely debilitated, require prolonged hospitalization and may eventually die [7]. The incidence rate of HC is predicted to rise substantially in the future as more aggressive treatments of cancer are implemented [9]. This acute complication is associated with significant rates of morbidity and mortality; treatment entails prolonged hospitalization and may require aggressive measures such as selective vesicle artery embolization or even cystectomy [8].
While dysuria, frequent voiding and urgency can be controlled with a symptomatic therapy, the challenging therapeutic targets in chemotherapy-induced HC are micturition symptoms and massive hematuria.
To date the following symptomatic treatment methods have been thoroughly evaluated [9]:
- hyperhydration and continuous bladder irrigation
- intravesical therapies, e.g. chondroitine sulphate, sodium hyaluronate, prostaglandin, formalin, and alum irrigation
- systematic treatments, e.g. HBO, estrogen, sodium pentosanpolysulphate, recombinant factor VII or VIII, and aminocaproic acid
In our case report we outline the indications as well as procedural steps of our approach and compare the results with those of other therapies and troubleshooting recommendations. The report’s primary aim is to present the significant effect of an intravesical therapy with a specific product, Instillamed®, a combination of chondroitine sulphate and sodium hyaluronate. To the best of our knowledge, the treatment as described has not yet been used in chemotherapy- induced HC.
Patient information
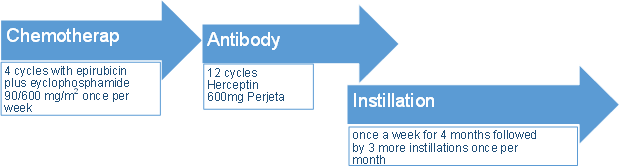
A 53-year old female patient presented with persistent dysuria, frequent voiding and nocturia. At the time the patient received adjuvant chemotherapy for her breast cancer (ypT2 (m) ypTis pyN1a (1/2) (sn) cMO G3 Stage IIB R1 VO PnO RO ER 90% PR 70% Her2neu +). Treatment included four cycles with epirubicin plus cyclophosphamide 90/600 mg/m2 on a weekly basis, followed by 12 cycles of weekly Taxol® and, every three weeks, Herceptin® 600mg and Perjeta®.
The patient presented with late-onset hemorrhagic cystitis after completing four cycles of chemotherapy, 10 weeks after finishing the last cycle. Therapy with D-Mannose had been tried without showing significant positive effects.
The patient had a daily fluid intake of 4–5 l, which relieved symptoms but caused a troublesome urgency-frequency syndrome.
Findings
Pelvic exam: External genitalia without erythema, exudate or discharge. The vestibulum is sensitive to pressure and pain. A hysterectomy was performed several years in the past. The vaginal vault is atrophic and no relevant prolapse is noted. The pelvic examination is unremarkable.
Dipstick test of the urine from intermittent catheter is positive for Erythrocytes, Leucocytes and Protein but negative for Nitrite. Bacteriological cultures were negative for bacterial growth.
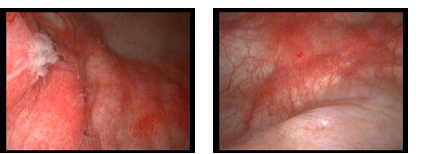
During cystoscopy the bladder capacity was limited to 150 ml. Bladder mucosa was hyperemic with inflamed flushing areas. Ureteral orifice was normal in size, shape and position, ureteral jets were seen, Bladder neck was normal. Based on the patient’s history and the symptoms, our diagnosis was: Chemotherapy induced hemorrhagic cystitis Grade 1.
The picture below depicts the author’s procedure findings.
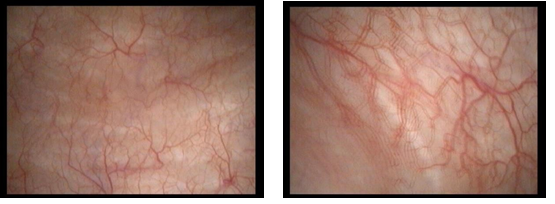
The pictures below show the author’s findings during procedure.
Method and Outcomes
We treated her with intravesical instillations of hyaluronic acid and chondroitin sulphate in order to substitute the GAG layer. The procedure was performed in an ambulant setting. Over a period of four months there were four instillations done once a week, followed by three more once a month.
At the end of this period objective changes could be seen:
- An increase of bladder capacity from 150 ml to 250 ml
- During a control cystoscopy bladder mucosa was normal, without any signs of irritation
- Bladder washing cytology was normal
Discussion
Severe HC is a major complication in patients undergoing chemo- and/or radiotherapy. Despite the improvement of prophylactic measures, the incident rate for HC continues to be significant and remains associated with raised morbidity and mortality rates for cancer patients. With a tendency towards more aggressive treatment of cancer under review, the incidence of HC is likely to further increase in the foreseeable future [9]. Therefore the complications affiliated with HC should be considered an increasingly important clinical issue, because they are for the most part challenging conditions to treat.
Treatment is based on hyperhydration, platelet and blood-cell transfusions, bladder irrigation and pain management. Where these measures have failed to control HC, numerous therapeutic approaches can be applied but with poor success. Surgery is seen as the ultimate therapeutic approach for this complication, but the inherent morbidity of a major surgical procedure in an extremely debilitated patient makes this approach very problematic [10].
Today out-patient procederus and short-stay hospitalization are prioritized by patients, medical professionals as well as health insurers for reasons of costs and quality of life.
We report the successful treatment of a patient with severe HC: the ambulatory procedure consisted of a seven-week course of intravesical application of a GAG layer-substitution product. We noted that the instillation therapy significantly relieved bleeding, pain as well as dysuria, and was well tolerated by the patient.
Since it is a successful, safe and cost-effective procedure with no apparent side effects, we strongly suggest that intravesical instillation to restore the GAG layer should be considered a first-line treatment option in cases of severe HC. The question arises whether this could also prove to be an effective prophylactic option.
To the best of our knowledge, this treatment has not yet been used in chemotherapy induced HC.
References
- Russell SJ, Vowels MR, Vale T. Haemorrhagic cystitis in paediatric bone marrow transplant patients: an association with infective agents, GVHD and prior cyclophosphamide. Bone Marrow Transplant 13 (1994): 533–539.
- Sandoval C, Swift M. Treatment of lymphoid malignancies in patients with ataxia- telangiectasia. Med Pediatr Oncol 31 (1998): 491–497.
- Le Guenno G, Mahr A, Pagnoux C, Dhote R, Guillevin L, French Vasculitis Study Incidence and predictors of urotoxic adverse events in cyclophosphamide-treated patients with systemic necrotizing vasculitides. Arthritis Rheum 63 (2011): 1435–1445.
- Klatersky J. Side effects of ifosfamide. Oncology 65 (2003): 7–10.
- Lima MV, Ferreira FV, Macedo FY, de Castro Brito GA, Ribeiro RA. Histological changes in bladders of patients submitted to ifosfamide chemotherapy even with mesna prophylaxis. Cancer Chemother Pharmacol 59 (2007): 643–650.
- Bassi PF, Costantini E, Foley S, Palea S. Glycosaminoglycan therapy for bladder diseases: emerging new treatments. Eur Urol Suppl 10 (2011): 451–459.
- Giné E, Rovira M, Real I, Burrel M, Montaña J, Carreras E, Montserrat E. Successful treatment of severe hemorrhagic cystitis after hemopoietic cell transplantation by selective embolization of the vesical arteries. Bone Marrow Transplant 31 (2003): 923–925.
- Decker DB, Karam JA, Wilcox DT. Pediatric hemorrhagic cystitis. J Pediatr Urol 5 (2009): 254–264.
- Payne H, Adamson A, Bahl A, Borwell J, Dodds D, Heath C, Huddart R, McMenemin R, Patel P, Peters JL, Thompson A. Chemical- and radiation-induced haemorrhagic cystitis: current treatments and challenges. BJU Int 112 (2013): 885–897.
- Baronciani D, Angelucci E, Erer B, Fabrizi G, Galimberti M, Giardini C, Milella D, Montesi M, Polchi P, Severini A, et al. Suprapubic cystotomy as treatment for severe hemorrhagic cystitis after bone marrow transplantation. Bone Marrow Transplant 16 (1995): 267–270.
