Successful Surgery for Coral Reef Aorta Owing to Takayasu’s Arteritis Complicated by Infected Aortic Aneurysms
Article Information
Tsutomu Doita MD1, Yoshiki Watanabe MD, PhD1, Takashi Shirakawa MD1, Osamu Iida, MD2, Yosuke Hata, MD2, Shinya Fukui MD, PhD1*
1Department of Cardiovascular Surgery, Kansai Rosai Hospital, Hyogo, Japan
2Department of Cardiology, Kansai Rosai Hospital, Hyogo, Japan
*Corresponding Author: Dr. Shinya Fukui, Department of Cardiovascular Surgery, Kansai Rosai Hospital, Inabaso 3-1-69, Amagasaki, Hyogo, 660-8511, Japan
Received: 21 November 2020; Accepted: 03 December 2020; Published: 04 January 2021
Citation: Tsutomu Doita, Yoshiki Watanabe, Takashi Shirakawa, Osamu Iida, Yosuke Hata, Shinya Fukui. Successful Surgery for Coral Reef Aorta Owing to Takayasu’s Arteritis Complicated by Infected Aortic Aneurysms. Archives of Clinical and Medical Case Reports 5 (2021): 001-007.
View / Download Pdf Share at FacebookAbstract
A 61-year-old woman presented with coral reef aorta (CRA) owing to Takayasu’s arteritis (TA) complicating infective aortic aneurysms. Though antibiotic therapy was continued, infective aortic aneurysms were growing, so urgent surgical treatment was required. First, we performed thoracic endovascular aortic repair (TEVAR) using trans-subclavian access, followed by open repair. TEVAR access and landing zone are limited in CRA cases. Moreover, the risk of persistent infection may be important in the situation where sepsis is ongoing. Few reports describe CRA complicated by infected aortic aneurysms. We describe a method of surgical treatment for this condition.
Keywords
Coral reef aorta; Infected aortic aneurysm; Takayasu’s arteritis; Thoracic endovascular aortic repair
Coral reef aorta articles; Infected aortic aneurysm articles; Takayasu?s arteritis articles; Thoracic endovascular aortic repair articles
Coral reef aorta articles Coral reef aorta Research articles Coral reef aorta review articles Coral reef aorta PubMed articles Coral reef aorta PubMed Central articles Coral reef aorta 2023 articles Coral reef aorta 2024 articles Coral reef aorta Scopus articles Coral reef aorta impact factor journals Coral reef aorta Scopus journals Coral reef aorta PubMed journals Coral reef aorta medical journals Coral reef aorta free journals Coral reef aorta best journals Coral reef aorta top journals Coral reef aorta free medical journals Coral reef aorta famous journals Coral reef aorta Google Scholar indexed journals Infected aortic aneurysm articles Infected aortic aneurysm Research articles Infected aortic aneurysm review articles Infected aortic aneurysm PubMed articles Infected aortic aneurysm PubMed Central articles Infected aortic aneurysm 2023 articles Infected aortic aneurysm 2024 articles Infected aortic aneurysm Scopus articles Infected aortic aneurysm impact factor journals Infected aortic aneurysm Scopus journals Infected aortic aneurysm PubMed journals Infected aortic aneurysm medical journals Infected aortic aneurysm free journals Infected aortic aneurysm best journals Infected aortic aneurysm top journals Infected aortic aneurysm free medical journals Infected aortic aneurysm famous journals Infected aortic aneurysm Google Scholar indexed journals Takayasu’s arteritis articles Takayasu’s arteritis Research articles Takayasu’s arteritis review articles Takayasu’s arteritis PubMed articles Takayasu’s arteritis PubMed Central articles Takayasu’s arteritis 2023 articles Takayasu’s arteritis 2024 articles Takayasu’s arteritis Scopus articles Takayasu’s arteritis impact factor journals Takayasu’s arteritis Scopus journals Takayasu’s arteritis PubMed journals Takayasu’s arteritis medical journals Takayasu’s arteritis free journals Takayasu’s arteritis best journals Takayasu’s arteritis top journals Takayasu’s arteritis free medical journals Takayasu’s arteritis famous journals Takayasu’s arteritis Google Scholar indexed journals Thoracic endovascular aortic repair articles Thoracic endovascular aortic repair Research articles Thoracic endovascular aortic repair review articles Thoracic endovascular aortic repair PubMed articles Thoracic endovascular aortic repair PubMed Central articles Thoracic endovascular aortic repair 2023 articles Thoracic endovascular aortic repair 2024 articles Thoracic endovascular aortic repair Scopus articles Thoracic endovascular aortic repair impact factor journals Thoracic endovascular aortic repair Scopus journals Thoracic endovascular aortic repair PubMed journals Thoracic endovascular aortic repair medical journals Thoracic endovascular aortic repair free journals Thoracic endovascular aortic repair best journals Thoracic endovascular aortic repair top journals Thoracic endovascular aortic repair free medical journals Thoracic endovascular aortic repair famous journals Thoracic endovascular aortic repair Google Scholar indexed journals CRA articles CRA Research articles CRA review articles CRA PubMed articles CRA PubMed Central articles CRA 2023 articles CRA 2024 articles CRA Scopus articles CRA impact factor journals CRA Scopus journals CRA PubMed journals CRA medical journals CRA free journals CRA best journals CRA top journals CRA free medical journals CRA famous journals CRA Google Scholar indexed journals treatment articles treatment Research articles treatment review articles treatment PubMed articles treatment PubMed Central articles treatment 2023 articles treatment 2024 articles treatment Scopus articles treatment impact factor journals treatment Scopus journals treatment PubMed journals treatment medical journals treatment free journals treatment best journals treatment top journals treatment free medical journals treatment famous journals treatment Google Scholar indexed journals CT articles CT Research articles CT review articles CT PubMed articles CT PubMed Central articles CT 2023 articles CT 2024 articles CT Scopus articles CT impact factor journals CT Scopus journals CT PubMed journals CT medical journals CT free journals CT best journals CT top journals CT free medical journals CT famous journals CT Google Scholar indexed journals surgery articles surgery Research articles surgery review articles surgery PubMed articles surgery PubMed Central articles surgery 2023 articles surgery 2024 articles surgery Scopus articles surgery impact factor journals surgery Scopus journals surgery PubMed journals surgery medical journals surgery free journals surgery best journals surgery top journals surgery free medical journals surgery famous journals surgery Google Scholar indexed journals SARS-COV-2 articles SARS-COV-2 Research articles SARS-COV-2 review articles SARS-COV-2 PubMed articles SARS-COV-2 PubMed Central articles SARS-COV-2 2023 articles SARS-COV-2 2024 articles SARS-COV-2 Scopus articles SARS-COV-2 impact factor journals SARS-COV-2 Scopus journals SARS-COV-2 PubMed journals SARS-COV-2 medical journals SARS-COV-2 free journals SARS-COV-2 best journals SARS-COV-2 top journals SARS-COV-2 free medical journals SARS-COV-2 famous journals SARS-COV-2 Google Scholar indexed journals tomography articles tomography Research articles tomography review articles tomography PubMed articles tomography PubMed Central articles tomography 2023 articles tomography 2024 articles tomography Scopus articles tomography impact factor journals tomography Scopus journals tomography PubMed journals tomography medical journals tomography free journals tomography best journals tomography top journals tomography free medical journals tomography famous journals tomography Google Scholar indexed journals
Article Details
Abbreviations:
CRA- Coral reef aorta; TA-Takayasu’s arteritis; TEVAR-Thoracic endovascular aortic repair
1. Introduction
Coral reef aorta (CRA) is a rare condition characterized by atherosclerosis and overt aortic calcification leading to severe luminal stenosis. Few reports describe CRA complicated by infected aortic aneurysms [1]. We describe a method of surgical treatment for this condition, and our case highlights the difficulty of treatment planning.
2. Case Report
A 61-year-old woman with minimal risk factors for lifestyle diseases was referred to us because of chest pain on effort and easy fatigability while walking. Computed tomography (CT) showed overt aortic calcification of thoracoabdominal aorta: coral reef aorta (CRA) (Figure 1). She met the American College of Rheumatology classification criteria of claudication of the extremities, bruit over the aorta, and arteriographic abnormalities [2].
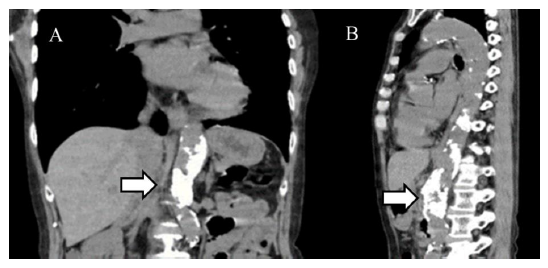
Figure 1: Coral reef aorta. Computed tomography image showing overt aortic calcification (arrow) from the lower thoracic aorta to the suprarenal abdominal aorta: coral reef aorta (A, B).
Her C-reactive protein level was low, so she was diagnosed as chronic and inactive Takayasu’s arteritis (TA). Moreover, coronary CT demonstrated no significant stenosis, so we monitored her symptoms. Five months later, she was admitted to our hospital with a fever and pain in her right wrist. CT showed no special findings except for CRA. Blood culture indicated Streptococcus pneumoniae; therefore, we diagnosed phlegmon and initiated antibiotic therapy. On admission day 12, she suddenly developed lumbar pain. Enhanced CT showed two thoracoabdominal aortic saccular aneurysms; the cranial aneurysm indicated impending rupture from the 7th to 8th thoracic vertebrae, and the caudal aneurysm extended from the 10th to 12th thoracic vertebrae (Figure 2).
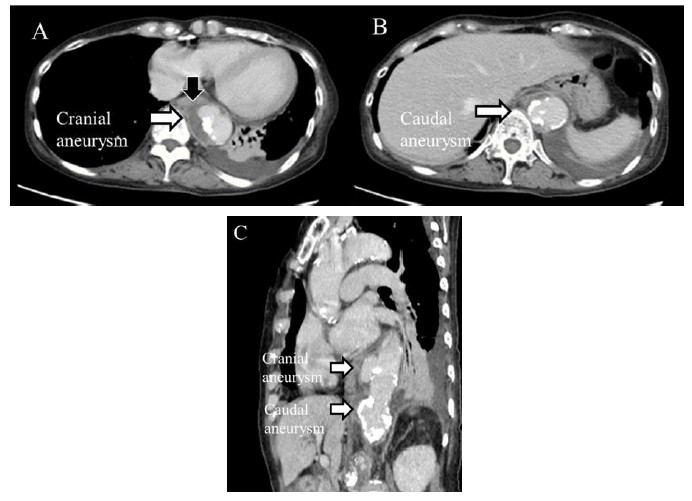
Figure 2: Two thoracoabdominal aortic saccular aneurysms. Enhanced computed tomography image showing two thoracoabdominal aortic saccular aneurysms; the cranial one with liquid accumulation around the aneurysm, which indicated impending rupture (black arrow). A, cranial aneurysm; B, caudal aneurysm; C, sagittal view.
Moreover, it revealed occlusion of celiac artery (CA) and superior mesenteric artery (SMA) due to severe calcification. We diagnosed infected aortic aneurysms according to the positive blood culture results (Streptococcus pneumoniae), liquid accumulation around the cranial aneurysm, and aneurysmal morphology. It was most important for us to prevent their rupture. Therefore, we performed emergent thoracic endovascular aortic repair (TEVAR) only for the cranial aneurysm with impending rupture, because it was difficult to place a stent distal to the caudal aneurysm because of the severe aortic calcification (Figure 2C). We used transsubclavian access because the CRA made it difficult to use transfemoral access (Figure 1, 3). An 18-Fr introducer sheath was inserted for delivery of the main device. Two 32-mm × 45-mm ExcluderR devices (W. L. Gore & Associates, Flagstaff, Ariz) were deployed uneventfully (Figure 3).
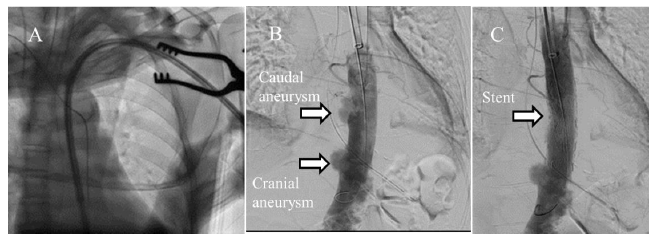
Figure 3: Angiography in thoracic endovascular aortic repair. A. We used transsubclavian access in the thoracic endovascular aortic repair; B. Angiographic image showing two thoracoabdominal aortic saccular aneurysms; C. We performed stenting to treat the cranial aneurysm.
We successfully performed TEVAR and continued enough antibiotics, but the caudal aneurysm gradually increased in size (Figure 4C, D, and E) and C-reactive protein level did not decrease to the normal ranges.
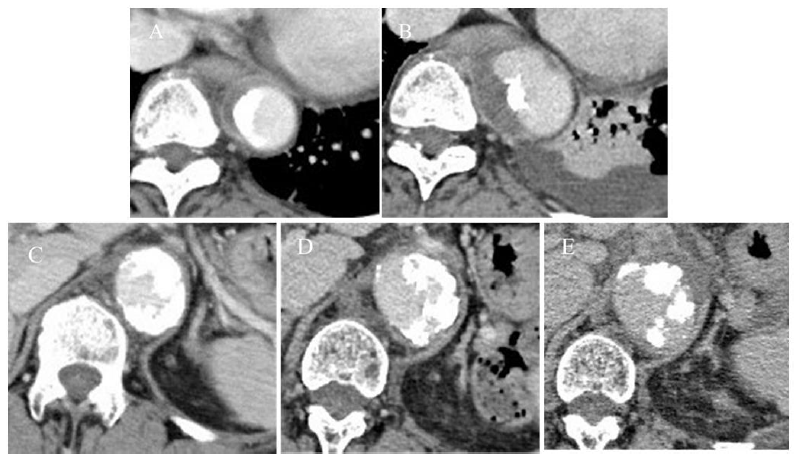
Figure 4: The change in the size of two infected aortic aneurysms. A and B are the cranial one respectively on admission day 1 and 12. Its maximum diameter changed from 30 to 51 mm; C, D, and E are the caudal one respectively on admission day 1, 12, and 33. Its maximum diameter was gradually enlarged from 32 to 40, and finally to 45 mm.
We performed open thoracoabdominal aortic repair on admission day 35. To prevent spinal cord ischemia, preoperative cerebral spinal fluid drainage was instituted. The right common femoral artery and vein were cannulated for partial cardiopulmonary bypass. We made a circumferential diaphragm incision, dissected the thoracic aorta and thoracoabdominal aorta and clamped the aorta proximally at the 6th, and distally at the 9th, intercostal space under partial cardiopulmonary bypass. We opened and transected the aorta, removed the stent graft, and thoroughly debrided the aortic wall. A rifampin-soaked graft (J graftR with four branches; Japan Lifeline Co., Ltd., Tokyo, Japan) was sutured to the proximal aorta. We released the proximal aortic clamp and repositioned the clamp between bilateral renal arteries (RAs) and the inferior mesenteric artery. The thoracoabdominal aorta was opened longitudinally, and the RAs were cannulated with 8-Fr cannulas and perfused. We removed overt calcification, back-flow from CA and SMA was confirmed and we completely resected the infected thoracoabdominal aortic aneurysm and tissue. The intercostal artery at the 12th intercostal space, which we believed was connected to the Adamkiewicz artery, was reconstructed with an 8-mm tube graft and anastomosed to the prosthetic graft. The other patent intercostal and lumbar arteries were then ligated. We reconstructed bilateral RAs, CA and SMA with the prosthetic branches and completed the anastomosis to the distal aorta. (Figure 5).
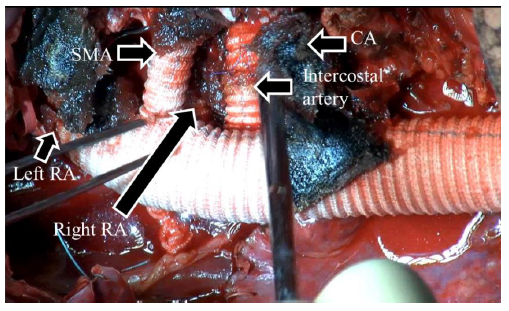
Figure 5: Intraoperative photograph. We performed thoracoabdominal bypass grafting and reconstructed the celiac, superior mesenteric, bilateral renal, and intercostal artery connection to the Adamkiewicz artery.
The postoperative course was uneventful, and the patient was intravenously treated by antibiotics for 1 month and discharged without morbidity. She is visiting outpatient clinic without recurrence of inflammatory symptom, taking oral antibiotics 9 months after surgery.
Histopathological examination of the resected aorta showed thickening of the intima with small nodular calcifications caused by atherosclerosis, plate-like calcification, and purulent inflammation (Figure 6). It indicates chronic TA complicated by infected aortic aneurysm.
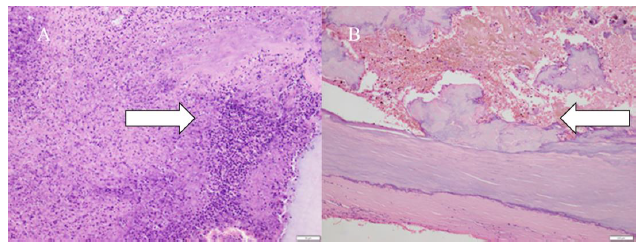
Figure 6: Histopathological examination of the resected aorta. Purulent inflammation (A, white arrow), and plate-like calcification (B, white arrow) in the intima.
3. Discussion
The pathophysiological basis of CRA is unknown. Some authors suspected infections [3], TA [4], or local amyloidosis3 as the disease underlying CRA. Other authors suggested that exogenous trauma with an extensive repair process in the dissected aortic wall may cause excessive calcification [3, 4]. Our patient was never treated for TA, and we assumed that chronic TA caused CRA. CRA complicated by infected aortic aneurysms is rare and needs precise surgical planning [1]. In recent years, endovascular repair has developed and we think that strategy for CRA with infection has changed. So, we prevented infected aneurysm rupture with CRA, using TEVAR as bridging procedure, and successfully treated it by graft replacing.
In TEVAR, we used trans-subclavian access, though a femoral artery approach is the most common for TEVAR. In cases of CRA, access and the TEVAR landing zone were limited because of the overt calcification. So, precise treatment planning for CRA before operation is necessary. TEVAR is easier to perform than open repair in an emergency and is useful to prevent rupture, because TEVAR does not need cerebral spinal fluid drainage in many cases and is performed by small incisions, on supine position and two-lungs ventilation. TEVAR could save us more time than open repair. The risk of persistent infection may be important in the situation where sepsis is ongoing. TEVAR is reported to be effective and a durable option for patients with infected aortic pseudoaneurysms [5]. So, we performed TEVAR at first as a bridging procedure to save the patient from aneurysms rupture, and finally thoracoabdominal bypass grafting. If TEVAR is impossible according to access, landing zone, atherosclerosis, and vascular diameter, open repair should be required at first even if it is in an emergency. Open repair for infected aneurysm has been a reliable procedure for a long time, however, less invasive TEVAR should be considered as a bridging or a destination procedure in recent era.
4. Conclusion
Rapid surgical treatment is required to prevent rupture of infected aneurysms. TEVAR is easier to perform than open repair. TEVAR is effective as bridging procedure before open repair in an emergency.
5. Conflict of Interest Statement
All authors declare no conflicts of interest and no funding.
References
- Qvarfordt PG, Reilly LM, Sedwitz MM, et al. “Coral reef” atherosclerosis of the suprarenal aorta: a unique clinical study. J Vasc Surg 1 (1984): 903-909.
- Arend WP, Michel BA, Bloch DA, et al. The American College of Rheumatology 1990 criteria for the classification of Takayasu arteritis. Arthritis Rheum 33 (1990): 1129-1134.
- Charnsangavej C. Intraluminal calcification and occlusion of the abdominal aorta above the renal arteries. Cardiovasc Intervent Radiol 4 (1981): 242-244.
- Combe J, Huart JY, Kantelip B, et al. Amyloidosis of a coral reef infrarenal aorta. J Mal Vasc 22 (1997): 43-47.
- Ting AC, Cheng SW, Ho P, et al. Endovascular stent graft repair for infected thoracic aortic pseudoaneurysms—a durable option? J Vasc Surg 44 (2006): 701-705.
