Subacute Lethal Bilateral Leg Time-Lag Infection by Streptococcus dysgalactiae
Article Information
Department of Acute Critical Care Medicine, Shizuoka Hospital, Juntendo University, Japan
*Corresponding Author: Dr. Youichi Yanagawa, 1129 Nagaoka, Izunokuni City, Shizuoka, Japan
Received: 31 May 2019; Accepted: 06 June 2019; Published: 12 August 2019
Citation: Hiroki Nagasawa, Youichi Yanagawa, Sei Kutsumi, Ken-ichi Muramatsu, Yoshihiro Kushida, Ikuto Takeuchi, Hiromichi Ohsaka, Kei Jitsuiki, Kazuhiko Omori, Yasumasa Oode. Subacute Lethal Bilateral Leg Time-Lag Infection by Streptococcus dysgalactiae. Archives of Clinical and Medical Case Reports 3 (2019): 153-157.
View / Download Pdf Share at FacebookAbstract
A 66-year-old man felt left leg pain 7 days prior to admission to our hospital. His history included diabetes mellitus, hypertension, alcoholic live disease and chronic renal failure without hemodialysis. He drank 90 g of ethanol per day. As the pain gradually became exacerbated, he visited a local clinic on foot. The chemical laboratory analysis showed thrombocytopenia, so he was admitted to our department. On arrival, his consciousness was clear, and he had stable vital signs. He had bilateral lichen legs, and the left leg showed swelling, tenderness and redness. Computed tomography revealed a high-density area of soft tissue in the left leg. The patient was treated with meropenem and linezolid. On the second hospital day, he felt improvement of pain in his left leg, but began to feel pain in his right leg. He had oligouria. The same day, his blood pressure and respiratory function deteriorated, and both legs became red with purpura. He died on the third hospital day. Streptococcus dysgalactiae was detected in the blood and skin of his left leg cultures. We herein report a unique case of invasive Streptococcus dysgalactiae infection. Elderly patients with underlying diseases, who might have a soft tissue infection, may require early aggressive debridement of the infected tissue, in addition to performing prophylactic decontaminated measurements of the uninfected area.
Keywords
Streptococcus dysgalactiae, Bilateral leg infection, Fatal
Streptococcus dysgalactiae articles Streptococcus dysgalactiae Research articles Streptococcus dysgalactiae review articles Streptococcus dysgalactiae PubMed articles Streptococcus dysgalactiae PubMed Central articles Streptococcus dysgalactiae 2023 articles Streptococcus dysgalactiae 2024 articles Streptococcus dysgalactiae Scopus articles Streptococcus dysgalactiae impact factor journals Streptococcus dysgalactiae Scopus journals Streptococcus dysgalactiae PubMed journals Streptococcus dysgalactiae medical journals Streptococcus dysgalactiae free journals Streptococcus dysgalactiae best journals Streptococcus dysgalactiae top journals Streptococcus dysgalactiae free medical journals Streptococcus dysgalactiae famous journals Streptococcus dysgalactiae Google Scholar indexed journals Bilateral leg infection articles Bilateral leg infection Research articles Bilateral leg infection review articles Bilateral leg infection PubMed articles Bilateral leg infection PubMed Central articles Bilateral leg infection 2023 articles Bilateral leg infection 2024 articles Bilateral leg infection Scopus articles Bilateral leg infection impact factor journals Bilateral leg infection Scopus journals Bilateral leg infection PubMed journals Bilateral leg infection medical journals Bilateral leg infection free journals Bilateral leg infection best journals Bilateral leg infection top journals Bilateral leg infection free medical journals Bilateral leg infection famous journals Bilateral leg infection Google Scholar indexed journals Fatal articles Fatal Research articles Fatal review articles Fatal PubMed articles Fatal PubMed Central articles Fatal 2023 articles Fatal 2024 articles Fatal Scopus articles Fatal impact factor journals Fatal Scopus journals Fatal PubMed journals Fatal medical journals Fatal free journals Fatal best journals Fatal top journals Fatal free medical journals Fatal famous journals Fatal Google Scholar indexed journals health articles health Research articles health review articles health PubMed articles health PubMed Central articles health 2023 articles health 2024 articles health Scopus articles health impact factor journals health Scopus journals health PubMed journals health medical journals health free journals health best journals health top journals health free medical journals health famous journals health Google Scholar indexed journals tissue infection articles tissue infection Research articles tissue infection review articles tissue infection PubMed articles tissue infection PubMed Central articles tissue infection 2023 articles tissue infection 2024 articles tissue infection Scopus articles tissue infection impact factor journals tissue infection Scopus journals tissue infection PubMed journals tissue infection medical journals tissue infection free journals tissue infection best journals tissue infection top journals tissue infection free medical journals tissue infection famous journals tissue infection Google Scholar indexed journals diabetes mellitus articles diabetes mellitus Research articles diabetes mellitus review articles diabetes mellitus PubMed articles diabetes mellitus PubMed Central articles diabetes mellitus 2023 articles diabetes mellitus 2024 articles diabetes mellitus Scopus articles diabetes mellitus impact factor journals diabetes mellitus Scopus journals diabetes mellitus PubMed journals diabetes mellitus medical journals diabetes mellitus free journals diabetes mellitus best journals diabetes mellitus top journals diabetes mellitus free medical journals diabetes mellitus famous journals diabetes mellitus Google Scholar indexed journals thrombocytopenia articles thrombocytopenia Research articles thrombocytopenia review articles thrombocytopenia PubMed articles thrombocytopenia PubMed Central articles thrombocytopenia 2023 articles thrombocytopenia 2024 articles thrombocytopenia Scopus articles thrombocytopenia impact factor journals thrombocytopenia Scopus journals thrombocytopenia PubMed journals thrombocytopenia medical journals thrombocytopenia free journals thrombocytopenia best journals thrombocytopenia top journals thrombocytopenia free medical journals thrombocytopenia famous journals thrombocytopenia Google Scholar indexed journals patient articles patient Research articles patient review articles patient PubMed articles patient PubMed Central articles patient 2023 articles patient 2024 articles patient Scopus articles patient impact factor journals patient Scopus journals patient PubMed journals patient medical journals patient free journals patient best journals patient top journals patient free medical journals patient famous journals patient Google Scholar indexed journals medicine articles medicine Research articles medicine review articles medicine PubMed articles medicine PubMed Central articles medicine 2023 articles medicine 2024 articles medicine Scopus articles medicine impact factor journals medicine Scopus journals medicine PubMed journals medicine medical journals medicine free journals medicine best journals medicine top journals medicine free medical journals medicine famous journals medicine Google Scholar indexed journals treatment articles treatment Research articles treatment review articles treatment PubMed articles treatment PubMed Central articles treatment 2023 articles treatment 2024 articles treatment Scopus articles treatment impact factor journals treatment Scopus journals treatment PubMed journals treatment medical journals treatment free journals treatment best journals treatment top journals treatment free medical journals treatment famous journals treatment Google Scholar indexed journals
Article Details
1. Introduction
Streptococcus dysgalactiae infection can range in severity from relatively mild skin and soft-tissue conditions, such as wound infection, erysipelas, and most commonly cellulitis, to life-threatening necrotizing fasciitis and streptococcal toxic shock syndrome [1]. Invasive forms of this infection are most commonly found in elderly patients with underlying comorbidities and skin breakdown [1]. We herein report a patient with alcoholic liver disease, chronic renal failure, diabetes mellitus and hypertension who suffered from the subacute onset of lethal soft tissue infection of the bilateral legs induced by S. dysgalactiae.
2. Case Presentation
A 66-year-old man felt left leg pain 7 days prior to admission to our hospital. His history included diabetes mellitus, hypertension, alcoholic liver disease and chronic renal failure without hemodialysis. He drank 90 g of ethanol per day. He had received prescriptions for irbesartan amlodipine besilate, atenolol, teneligliptin, pioglitazone and ursodeoxycholic acid. As the pain gradually became exacerbated, he visited a local clinic on foot.
The chemical laboratory analysis showed thrombocytopenia, so he was admitted to our department. On arrival, his consciousness was clear. A physical examination revealed the following findings: blood pressure, 108/57 mmHg; heart rate, 76 beats per minute (BPM); respiratory rate, 22 BPM; SpO2, 94% under room air; and body temperature, 37°C. His bilateral legs had lichen, suggesting a history of inflammation. In addition, the left leg had swelling, tenderness and redness. A venous gas analysis revealed the following findings: pH, 7.351; PCO2, 29.9 mmHg; PO2, 40.0 mmHg; HCO3-, 16.1 mmol/L; base excess -7.9 mmol/L; and lactate, 5.0 mmol/L. Electrocardiography revealed sinus tachycardia. Chest roentgenography revealed cardiomegaly. Whole-body computed tomography revealed a high-density area of soft tissue in the left leg (Figure 1). The main results of a blood analysis were as follows: white blood cell count, 4,600/mm3; hemoglobin, 13.0 g/dL; platelet count, 2.9 × 104/mm3; total protein, 6.7 g/dL; albumin, 2.9 g/dL; total bilirubin, 2.1 mg/dL; aspartate aminotransferase, 53 IU/L; alanine aminotransferase, 25 U/L; creatine phosphokinase, 123 IU/L; amylase, 60 IU/L; lactate dehydrogenase, 397 IU/L, blood urea nitrogen, 58.9 mg/dL; creatinine, 3.25 mg/dL; glucose, 127 mg/dL; HbA1C, 6.2%; sodium, 135 mEq/L; potassium, 4.8 mEq/L; chloride, 108 mEq/L; C-reactive protein, 22.9 mg/dL; activated partial thromboplastin time, 34.0 (24.9) seconds; prothrombin time, 14.1 (11.9) seconds; and fibrinogen degradation products, 104 μg/mL.
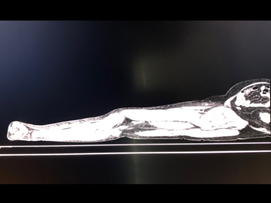
Figure 1: Computed tomography (CT) of the left leg on arrival. CT revealed a high-density area of soft tissue in the left leg.
As cellulitis was initially suspected, the patient was treated with meropenem and linezolid in the general ward after blood samples were obtained for culturing. On the second hospital day, he reported improvement of the pain in the left leg; however, began to feel pain in his right leg. His urinary output per night was almost 0 ml. That same afternoon, his blood pressure and respiratory function deteriorated, so he was moved to the intensive-care unit, and tracheal intubation was performed in addition to the infusion of noradrenalin and massive infusion of Ringer’s lactate solution. In addition, both legs became red with purpura (Figure 2). We recommended both of his legs be amputated, but his family refused to consent to the operation. His respiration and circulation became unstable, and he ultimately died on the third day of hospitalization. S. dysgalactiae was detected in the blood and skin of his left leg cultures. We were unable to obtain permission to perform an autopsy.

Figure 2: Bilateral legs on the second hospital day. Both legs developed redness with purpura.
3. Discussion
The present case has three unique points. The first point is the time course of the disease. While invasive Streptococcus infection is typically rapid, the time course of the present case was more than one week [1-3]. The second point is the time-lag infection of the bilateral legs in a single subject. The present patient initially reported improvement of his subjective symptoms in the left leg, but the opposite leg also was found to be infected on the eighth day, leaving both legs ultimately infected. This suggested the ping-pong transmission of Streptococcus infection between the two legs in the same subject [4]. The third point is the timing of amputation. The present patient had stable vital signs initially, and the color of his skin resembled that associated with cellulitis. Accordingly, we selected conservative treatment with antibiotics. While the initial response to the treatments was good for the left leg, the opposite leg subsequently became infected. We believed that the condition of the opposite leg would similarly be improved by antibiotic treatment, but this approach failed.
Bilateral and simultaneous lower extremity amputations unrelated to diabetes, peripheral vascular disease and trauma are uncommon [5, 6]. Bilateral amputation in the late phase of purpura fulminans has been reported, but the efficacy of such a procedure in the acute setting is poor [7, 8]. We were unable to find any reports of cases that obtained a survival outcome after bilateral amputation following invasive S. dysgalactiae infection [9].
Invasive forms of this infection are most commonly found in elderly patients with underlying comorbidities and skin breakdown [1]. Accordingly, elderly patients with underlying diseases, who might have soft tissue infection, may require early aggressive debridement of the infected tissue, in addition to performing prophylactic decontaminated measurements of the uninfected area.in order to obtain a survival and favorable functional outcome.
4. Conclusion
We encountered a unique case of invasive S. dysgalactiae infection. Elderly patients with underlying diseases, who might have soft tissue infection, may require early aggressive debridement of the infected tissue, in addition to performing prophylactic decontaminated measurements of the uninfected area.
Conflict of Interest
The authors declare no conflicts of interest in association with the present study.
Acknowledgements
This manuscript received financial support from the Ministry of Education, Culture, Sports, Science and Technology (MEXT)-supported Program for the Strategic Research Foundation at Private Universities, 2015-2019, concerning [The constitution of a total research system for comprehensive disaster and medical management, corresponding to a wide-scale disaster].
References
- Rantala S. Streptococcus dysgalactiae subsp. equisimilis bacteremia: an emerging infection. Eur J Clin Microbiol Infect Dis 33 (2014): 1303-1310.
- Watanabe S, Takemoto N, Ogura K, et al. Severe invasive streptococcal infection by Streptococcus pyogenes and Streptococcus dysgalactiae subsp. equisimilis. Microbiol Immunol 60 (2016): 1-9.
- Mori M, Kitagawa T, Sasaki Y, et al. Streptococcal toxic shock-like syndrome caused by Streptococcus dysgalactiae subsp. equisimilis in a patient with acute myeloid leukemia at diagnosis. Rinsho Ketsueki 54 (2013): 219-223.
- Falck G, Holm SE, Kjellander J, et al. The role of household contacts in the transmission of group A streptococci. Scand J Infect Dis 29 (1997): 239-244.
- Taylor M, McKay D, Eid M, et al. What are the ethical issues in treating a patient with bilateral leg gangrene incapable of consenting to amputation secondary to psychiatric illness? Clin Orthop Relat Res 473 (2015): 3998-4003.
- Penn-Barwell JG, Bennett PM, Kay A, et al. Severe Lower Extremity Combat Trauma (SeLECT) Study Group. Acute bilateral leg amputation following combat injury in UK servicemen. Injury 45 (2014): 1105-1110.
- Hacking HG, Lo-a-Njoe BA, Visser-Meily JM. Multiple amputations due to sepsis: however, functional rehabilitation is possible. Ned Tijdschr Geneeskd 143 (1999): 1073-1077.
- Tomita Y, Miyano S, Ohashi M, et al. A case of bilateral hip disarticulation caused with toxic shock like syndrome. SOGO rehabilitation 2001; 29: 949-953.
- Yoshizawa T, Ishikawa K, Nagasawa H, et al. A Fatal Case of Super-super Obesity (BMI >80) in a Patient with a Necrotic Soft Tissue Infection. Intern Med 57 (2018): 1479-1481.
