Study of Coracoid Bone Graft Osteolysis Following Latarjet Procedure for Recurrent Traumatic Anterior Shoulder Dislocation
Article Information
Ahmed Wahid Kandil1*, Mohammad Mesbah Elwany1, Karim Mohamed Elsharkawi2, Mohie Eldin Mahmoud Fadel1
1Department of Orthopaedic Surgery and Traumatology, Faculty of Medicine, Alexandria University, Egypt
2Department of Radiodiagnosis and Intervention, Faculty of Medicine, Alexandria University, Egypt
*Corresponding Author: Ahmed Wahid Kandil, Department of Orthopaedic Surgery and Traumatology, Faculty of Medicine, Alexandria University, Egypt.
Received: 15 May 2025; Accepted: 22 May 2025; Published: 29 May 2025
Citation:
Ahmed Wahid Kandil, Mohammad Mesbah Elwany, Karim Mohamed Elsharkawi, Mohie Eldin Mahmoud Fadel. Study of Coracoid Bone Graft Osteolysis Following Latarjet Procedure for Recurrent Traumatic Anterior Shoulder Dislocation. Journal of Orthopedics and Sports Medicine. 7 (2025): 256-261.
View / Download Pdf Share at FacebookAbstract
Background: The Latarjet procedure is a reliable and successful method for treating shoulder instability. Despite its success, the Latarjet procedure is associated with a reported complication rate of approximately 15%.
Patient and method: The study included 30 patients with recurrent traumatic anterior shoulder dislocation treated with the Latarjet procedure. The age of the patients ranged from 19 to 37 years old, and the mean age was 27.43 ± 5.73. 26 patients were males (86.7%), and 4 patients were females (13.3%). The right side was affected in 16 patients (60%), and the left side was affected in 14 (40%) patients. The dominant side was affected in 19 patients (63.3%), while the non-dominant side was affected in 11 patients (36.7%).
Results: Age, smoking, and significant preoperative glenoid bone loss were found as risk factors for increased levels of osteolysis, while gender and dominant side were not. There was no correlation of statistical significance between postoperative (Rowe score) and overall osteolysis of the coracoid bone graft.
Conclusion: coracoid bone graft osteolysis is a common finding after the Latarjet procedure within the first six months, predominantly affecting the superficial proximal graft region. Importantly, this osteolysis did not correlate with negative clinical outcomes in our cohort. Age, smoking, and glenoid bone loss emerged as potential risk factors that correlate with levels of bone resorption.
Keywords
Bone Graft; Coracoid; Osteolysis; Latarjet; Shoulder Dislocation
Bone Graft articles; Coracoid articles; Osteolysis articles; Latarjet articles; Shoulder Dislocation articles
Article Details
1. Introduction
The stability of the glenohumeral joint is determined by the interaction of both static and dynamic stabilizers. While static stabilizers, encompassing the glenoid labrum, ligaments, and joint capsule, provide passive support, dynamic stabilization is primarily mediated by the periarticular musculature, notably the rotator cuff [1]. The presence of Hill-Sachs and Bankart lesions can significantly increase the likelihood of repeated shoulder dislocations [2]. Bankart repair (open or arthroscopic) and the Latarjet procedure are common surgical treatments for recurrent anterior shoulder dislocation [3].
The Latarjet procedure is a reliable and successful method for treating shoulder instability. The "sling" effect created by this procedure helps to prevent the shoulder from dislocating anteriorly, especially when the arm is abducted and externally rotated [4].
Coracoid bone osteolysis can occur due to a combination of biological and biomechanical factors. These factors include the shape and size of the graft, the preoperative glenoid bone loss, the availability of blood supply from multiple sources, the stability and appropriate mechanical loading at the graft-glenoid interface, which are essential for bone remodeling and infection that can also contribute to graft failure [5,6].
Despite its success, the Latarjet procedure is associated with a reported complication rate of approximately 15%, with osteolysis, or the resorption of the transferred coracoid bone graft, being among these complications [7].
The aim of this study was to study the coracoid bone graft osteolysis following the Latarjet procedure for recurrent traumatic anterior shoulder dislocation.
2. Materials and Methods
This is a prospective study that included 30 patients with recurrent traumatic anterior shoulder dislocation treated with the Latarjet procedure. Surgeries were performed in the arthroscopy unit of our University Hospital. Data were collected from November 2023 till December 2024. All patients completed a period of at least 6 months of follow-up. Informed written consent was obtained from the patients. The study was done after approval from the Ethics Committee of the Faculty of Medicine.
The inclusion criteria included patients aged between 19 and 40 years old with recurrent anterior shoulder dislocation. Patients with rotator cuff tear and multidirectional instability were excluded from the study.
2.1 Operative technique:
Surgical Approach:
The surgery was conducted under general anesthesia, and the patients were positioned in the beach chair position. A 5- to 7-cm incision is made along the deltopectoral interval, and the interval between the deltoid and pectoralis major muscles was identified by the presence of the cephalic vein which was retracted laterally with the deltoid muscle.
The pectoralis minor muscle is identified, and its attachment to the medial side of the coracoid was released, then the coracoacromial ligament (CAL) was cut from the lateral side of the coracoid. Then, osteotomy of the coracoid at its base using a sharp osteotome. The inferior surface of the coracoid is cleaned from any remaining soft tissue and decorticated until a broad, flat, bleeding surface.
Upper and lower borders of the subscapularis are identified, and it is bluntly split in line with its fibers along the junction of its proximal two-thirds and distal one-third or between its upper and lower half. After a capsulotomy, the glenoid neck is subperiosteally dissected, and the anterior-inferior glenoid labrum is removed. Then, decortication of the anterior glenoid neck is done till reaching a bleeding surface of bone.
The longitudinal axis of the coracoid graft is positioned superoinferiorly along the glenoid neck flush with the articular surface. Then, two 3.5-mm titanium screws were used to fix the coracoid graft in position. The subcutaneous dermal layer is subsequently closed with interrupted sutures followed by subcuticular skin closure.
After surgery, a sling was usually worn for the first three to six weeks. The patient may, however, engage in mild passive shoulder range of motion in the scapular plane during this initial phase. After six weeks, during clinical follow-up assessments, active range of motion is started and increased gradually, strengthening exercises are initiated and increased gradually to rebuild shoulder muscle strength, and light activities may be resumed. Usually, recovery from surgery requires up to three months before one may resume contact sports or strenuous jobs.
2.2 Clinical and Radiological assessment
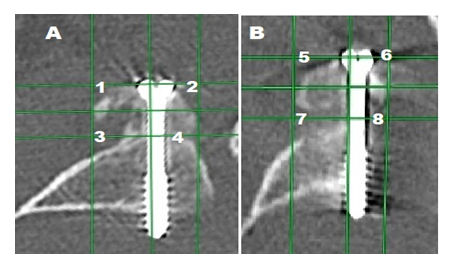
Patients were evaluated pre- and postoperatively using the Rowe Score for Instability. An initial CT scan of the shoulder was done after surgery; and another follow-up CT scan was done after 6 months. The coracoid bone graft was partitioned into eight sections. Two primary areas were identified as superficial and deep, and each of these was further subdivided into proximal, distal, medial, and lateral portions. In the axial oblique cut of the CT scan, the reference point is the superior screw, creating the proximal portion, and the inferior screw is the other reference point in the distal portion. The surface area of the eight parts of the coracoid bone graft was measured and compared between CT taken after the Latarjet surgery and 6 months afterwards (Figure 1).
2.3 Statistical Analysis
Data were fed to the computer and analyzed using the IBM SPSS software package version 20.0. (NY: IBM Corp.) (72) Qualitative data were described using numbers and percentages. The Shapiro-Wilk test was used to verify the normality of distribution. Quantitative data were described using range (minimum and maximum), mean, standard deviation, median, and interquartile range (IQR). The significance of the obtained results was judged at the 5% level. The used test was Wilcoxon signed ranks test for abnormally distributed quantitative variables, to compare between two periods.
3. Results
Analysis of initial and follow-up CT scans revealed osteolysis of the coracoid bone graft in all cases. Osteolysis of the coracoid bone graft demonstrated significant inter-patient variability, with a mean resorption of 48.5% ± 8.2% of the original graft volume, minimal osteolysis was 30% and maximal osteolysis was 58.97%.
3.1 CT assessment:
CT scan analysis revealed significant regional variations in coracoid bone graft osteolysis. The proximal coracoid, particularly its superficial aspects exhibited the highest mean osteolysis percentages (medial: 67.69% ± 10.97%, lateral: 62.10% ± 16.17%). Conversely, the deep regions of the distal coracoid demonstrated the lowest levels of bone resorption (lateral: 33.92% ± 14.22%, medial: 29.89% ± 12.28%) (Table 1).
|
Osteolysis |
Min. – Max. |
Mean ± SD. |
Median (IQR) |
|
Proximal Superficial Medial |
30.05 – 84.73 |
67.69 ±10.97 |
70.31 (68.77 – 71.67) |
|
Proximal Superficial Lateral |
5.47 – 81.98 |
62.10 ±16.17 |
66.75 (61.78 – 70.67) |
|
Proximal Deep Medial |
12.83 – 81.33 |
59.18 ±16.55 |
63.88 (52.26 – 69.21) |
|
Proximal Deep Lateral |
16.79 – 89.67 |
50.81 ±20.39 |
48.44 (33.78 – 67.46) |
|
Distal Superficial Medial |
12.78 – 80.32 |
46.86 ±20.24 |
42.93 (29.05 – 65.14) |
|
Distal Superficial Lateral |
7.81 – 55.30 |
38.76 ±11.73 |
40.65 (31.70 – 48.30) |
|
Distal Deep Lateral |
10.23 – 62.35 |
33.92 ±14.22 |
32.92 (23.71 – 42.51) |
|
Distal Deep Medial |
9.32 – 59.96 |
29.89 ±12.28 |
29.94 (22.82 – 32.96) |
Table 1: Descriptive analysis of the studied cases according to the percentage of osteolysis of the graft segments (n = 30).
3.2 Analysis of potential risk factors and overall osteolysis:
Gender and dominant side showed no statistically significant difference regarding overall osteolysis in the studied group. On the other hand, a statistically significant direct correlation was observed between patient age and the extent of overall osteolysis, showing that younger individuals presented with a lower degree of osteolysis compared to older individuals. Furthermore, glenoid bone loss (GBL) ranged between 0% and 19.5%. A statistically significant inverse correlation was found between the extent of preoperative GBL and postoperative osteolysis, indicating that patients with minimal or no preoperative GBL exhibited a greater degree of osteolysis following the procedure, while those with more substantial initial GBL experienced less postoperative bone resorption. (Table 2). In this study, a statistically significant difference in the degree of osteolysis was found between the smokers and non-smokers, with the smoker group exhibiting a higher level of bone graft resorption (Table 3).
|
Overall osteolysis |
||
|
r |
p |
|
|
Age (years) |
0.536* |
0.002* |
|
Glenoid bone loss |
–0.802* |
<0.001* |
Table 2: Correlation between overall osteolysis and both age and glenoid bone loss (n = 30).
|
N |
Overall osteolysis |
t |
P |
||
|
Mean ± SD. |
Median (Min. – Max.) |
||||
|
Smoking |
|||||
|
Non-smoker |
12 |
43.57 ± 6.98 |
43.77 (31.05 – 57.71) |
3.411* |
0.002* |
|
Smoker |
18 |
52.04 ± 6.45 |
53.26 (30.0 – 58.97) |
||
Table 3: Relation between overall osteolysis and smoking (n = 30).
Preoperatively, Rowe scores ranged from 25 to 70 points, with a mean of 54.83 ± 13.29 points. This distribution showed that 12 patients (40%) exhibited poor Rowe scores, while 18 patients (60%) demonstrated fair Rowe scores. Postoperatively, Rowe scores ranged from 15 to 95 points, with a mean of 85.67 ± 16.12 points. These outcomes were categorized as follows: 20 patients (66.7%) achieved excellent results, 7 patients (23.3%) demonstrated good results, 2 patients (6.7%) exhibited fair results, and 1 patient (3.3%) experienced a poor outcome. There was a statistically significant improvement of postoperative Rowe score.
3.3 Other complications:
There was a single patient that had iatrogenic musculocutaneous nerve injury, and this resulted in poor results regarding his clinical outcome, and unfortunately, long-term follow-up data for this patient could not be obtained as he could not be reached. Another patient had suffered from a superficial infection, which was treated with antibiotics and was completely resolved, and this resulted in some delay in his rehabilitation program and affected his clinical course, and his total Rowe score was fair.
4. Discussion
Our current study prospectively analyzed data from 30 patients with anterior shoulder instability who underwent open Latarjet procedure. The follow-up period for these patients extended to six months.
Our findings revealed the occurrence of osteolysis in the coracoid bone graft in all participants. The average degree of osteolysis observed at six months post-surgery was 48.5% ± 8.2%. Notably, the superficial medial region of the proximal half of the graft exhibited the most significant resorption, averaging 67.69%, closely followed by the superficial lateral region of the same half, with an average of 62.1%. Conversely, the deep medial region of the distal part of the graft showed the least amount of osteolysis, averaging 29.89%, with the deep lateral region exhibiting a mean osteolysis of 33.92%.
These observations are consistent with previous research documenting varying levels of coracoid bone graft resorption following the Latarjet procedure. Di Giacomo et al. were among the first to meticulously document the specific location and extent of coracoid graft osteolysis using computed tomography (CT) scan analysis. Their study, with an average 12-month follow-up, reported an average of 59.5% osteolysis in the grafted bone, with the most affected area being superficial and proximally located [8].
Similarly, Zhu et al. [9], through CT scans conducted approximately one year after the Latarjet procedure, found that 90.5% of their patient cohort experienced coracoid bone resorption. Their analysis also indicated more pronounced resorption around the superior screw compared to the inferior screw. Furthermore, they proposed a four-grade classification system for coracoid bone osteolysis based on axial CT images [9].
Haeni et al. [10] utilized three-dimensional CT scans to quantify the volume of osteolysis in the coracoid graft following arthroscopic Latarjet procedures. Their findings at six months post-operatively demonstrated significant osteolysis in the upper portion of the graft [10].
A study by Young Moon Kee et al. [11], spanning 37 months, also reported osteolysis in all cases, observed on oblique sagittal CT scans, with the superior aspect of the grafted bone being predominantly affected [11].
Interestingly, Zhu et al. [12] also demonstrated that the arthroscopic Latarjet technique resulted in significantly less graft resorption compared to the open approach in their prospective comparative study. They attributed this difference to the preservation of soft tissues during the arthroscopic procedure, which likely aids in maintaining the blood supply to the coracoid bone graft [12].
The phenomenon of osteolysis is likely influenced by both biological and mechanical factors. Maintaining adequate blood supply to the coracoid graft appears to mitigate the extent of resorption. Additionally, Wolff's law suggests that the lower portion of the anterior glenoid rim experiences greater stress during abduction and external rotation, potentially contributing to increased bone loss in the upper part of the graft. Variations in surgical techniques, including graft harvesting and fixation methods, may also play a role in the degree of osteolysis. Therefore, careful consideration of these factors during surgical planning is essential for optimizing outcomes [9].
Our investigation into potential risk factors for coracoid bone graft osteolysis revealed that while gender and the dominant side did not show a statistically significant association, age, smoking, and the extent of glenoid bone loss were significant predictors of osteolysis.
These findings partially align with prior research. Di Giacomo et al. observed less osteolysis in patients with significant glenoid bone loss (>15%) compared to those without [5]. However, Cohen et al. [13] identified the absence of significant preoperative glenoid bone loss as the sole risk factor for severe graft osteolysis, although this did not significantly impact clinical results [13].
Despite observing a statistically significant improvement in the Rowe score from the pre-operative to the post-operative period, we found no statistically significant correlation between clinical outcomes and the degree of coracoid bone graft osteolysis. This is consistent with previous studies. Di Giacomo et al. demonstrated that substantial graft resorption can occur without necessarily affecting clinical outcomes [8]. Similarly, Ryan S. Ting et al. [14] reported favorable clinical results in patients exhibiting significant bone graft resorption.
Consequently, Di Giacomo et al. [8] proposed that the bone block's contribution in the Latarjet procedure might not be the primary mechanism for treating anteroinferior shoulder instability. They reasoned that despite significant osteolysis, patients in their study did not experience pain, stiffness, subtle instability, or recurrent shoulder dislocation following the procedure [8].
In contrast, Yamamoto et al. [15] emphasized the critical role of bone grafting, particularly in cases involving significant bone loss in the shoulder glenoid.
While coracoid bone graft osteolysis in isolation may not have a clinical impact [7]. The accurate positioning of the graft relative to the glenoid margin remains the most critical determinant of the Latarjet procedure's technical success. Suboptimal graft placement can lead to complications such as nonunion, the development or progression of pre-existing osteoarthritis if positioned too laterally, and recurrent instability if positioned too medially [16].
This study has several limitations that warrant consideration. Firstly, the relatively small sample size may limit the generalizability of our findings. Secondly, the short follow-up duration of six months necessitates longer-term studies to fully understand the long-term effects of osteolysis on graft stability and clinical outcomes. Thirdly, our study did not delve into a detailed investigation of potential risk factors for osteolysis, such as bone quality and specific surgical techniques employed.
5. Conclusion
Our study confirms that coracoid bone graft osteolysis is a common finding after the Latarjet procedure within the first six months, predominantly affecting the superficial proximal graft region. Importantly, this osteolysis did not correlate with negative clinical outcomes in our cohort. Age, smoking, and glenoid bone loss emerged as potential risk factors that correlate with levels of bone resorption. Further long-term studies with larger groups are needed to better understand the implications of osteolysis and other contributing factors.
Conflicts of Interest: Nil
References
- Lugo R, Kung P, Ma CB. Shoulder biomechanics. Eur J Radiol 68 (2008): 16-24.
- Hovelius L, Olofsson A, Sandström B, et al. Nonoperative Treatment of Primary Anterior Shoulder Dislocation in Patients Forty Years of Age and Younger: A Prospective Twenty-five-Year Follow-up. J Bone Joint Surg Am 90 (2008): 945-52.
- Bishop JY, Hidden KA, Jones GL, et al. Factors Influencing Surgeon's Choice of Procedure for Anterior Shoulder Instability: A Multicenter Prospective Cohort Study. Arthroscopy 35 (2019): 2014-25.
- van der Linde JA, van Wijngaarden R, Somford MP, et al. The Bristow–Latarjet procedure, a historical note on a technique in comeback. Knee Surg Sports Traumatol Arthrosc 24 (2016): 470-8.
- Di Giacomo G, De Gasperis N, Costantini A, et al. Does the presence of glenoid bone loss influence coracoid bone graft osteolysis after the Latarjet procedure? A computed tomography scan study in 2 groups of patients with and without glenoid bone loss. J Shoulder Elbow Surg 23 (2014): 514-8.
- Young DC, Rockwood CA. Complications of a failed Bristow procedure and their management. J Bone Joint Surg 73 (1991): 969-81.
- Domos P, Lunini E, Walch G. Contraindications and complications of the Latarjet procedure. Shoulder Elbow 10 (2018): 15-24.
- Di Giacomo G, Costantini A, De Gasperis N, et al. Coracoid graft osteolysis after the Latarjet procedure for anteroinferior shoulder instability: a computed tomography scan study of twenty-six patients. J Shoulder Elbow Surg 20 (2011): 989-95.
- Zhu YM, Jiang CY, Lu Y, et al. Coracoid bone graft resorption after Latarjet procedure is underestimated: a new classification system and a clinical review with computed tomography evaluation. J Shoulder Elbow Surg 24 (2015): 1782-8.
- Haeni DL, Opsomer G, Sood A, et al. Three-dimensional volume measurement of coracoid graft osteolysis after arthroscopic Latarjet procedure. J Shoulder Elbow Surg 26 (2017): 484-9.
- Kee YM, Kim JY, Kim HJ, et al. Fate of coracoid grafts after the Latarjet procedure: will be analogous to the original glenoid by remodelling. Knee Surg Sports Traumatol Arthrosc 26 (2018): 926-32.
- Zhu Y, Jiang C, Song G. Arthroscopic versus open Latarjet in the treatment of recurrent anterior shoulder dislocation with marked glenoid bone loss: a prospective comparative study. Am J Sports Med 45 (2017): 1645-53.
- Cohen M, Zaluski AD, Siqueira GSL, et al. Risk Factors for Coracoid Graft Osteolysis after the Open Latarjet Procedure. Rev Bras Ortop (Sao Paulo) 55 (2020): 585-90.
- Ting RS, Jang B, Murray N, et al. An assessment of the clinical relevance of coracoid graft osteolysis following the Latarjet procedure: a clinical and radiological review. JSES Int 8 (2024): 719-23.
- Yamamoto N, Itoi E, Abe H, et al. Contact between the glenoid and the humeral head in abduction, external rotation, and horizontal extension: a new concept of glenoid track. J Shoulder Elbow Surg 16 (2007): 649-56.
- Marion B, Klouche S, Deranlot J, et al. A prospective comparative study of arthroscopic versus mini-open Latarjet procedure with a minimum 2-year follow-up. Arthroscopy 33 (2017): 269-77.