Stratification of THROMBOTIC RISK in Patients that are Undergoing to PICC Implantation: The CoRa-MaPiCC STUDY Corelli-Raimondi-Marchitto-Piovanello Project
Article Information
Marchitto N1*, Piovanello P2, Giacopelli P2 , Teseo L1, Panfilio S3, Raimondi G4
1Internal Medicine Department, Alfredo Fiorini Hospital, Terracina, Latina, Italy
2Surgery Department, Alfredo Fiorini Hospital, Terracina. Sapienza University of Rome, Italy
3First Haid Department, Alfredo Fiorini Hospital, Terracina, Latina, Italy
4Internal Medicine, Department of Medico-surgical Sciences and Biotechnologies. "Sapienza" University of Rome, Italy
*Corresponding Author: Dr. Nicola Marchitto, Specialist in Geriatry and Gerontology, Medical Assistant, Department of Internal Medicine, Alfredo Fiorini Hospital, Terracina, Latina, Italy
Received: 15 May 2018; Accepted: 31 May 2018; Published: 05 June 2018
Citation: Marchitto N, Piovanello P, Giacopelli P, Teseo L, Panfilio S, Raimondi G. Stratification of THROMBOTIC RISK in Patients that are Undergoing to PICC Implantation: The “CoRa-MaPiCC STUDY” Corelli-Raimondi-Marchitto-Piovanello Project. Journal of Surgery and Research 1 (2018): 22-33.
View / Download Pdf Share at FacebookAbstract
Background: The PICC is a central venous system inserted in the peripherally vein. The central peripheral catheter catheter system (PICC=peripherally inserted central catheters) is a widely used procedure in clinical practice by medical and nurse team. PICC has potential complications that are rare but not entirely irrelevant. It is used for continuous and discontinuous treatment and, after a correct insertion procedure, it can be used for a period of time between 1 week to 3 months. The last-generation dispositive has an high-biocompatibility due to the high quality of the materials (silicone or polyurethane), a total length of 40-60 cm and a diameter between 16 to 25 Gauge or 2 to 5 French.
Aims: The aim of our study is to evaluate the trombotic risk related to the positioning of the device in relation to the individual risk factors. Therefore we have elaborated the CoRaMaPicc protocol that allows, based on the preliminary data evaluation, to reduce the trombotic risk in patients with high cardiovascular risk profile.
Methods: The study has started in July 2016. We have enrolled 30 patients (18 males and 12 females with range age of 30-99 yrs and mean age of 82+13,5 yrs). Enrolled patients have Body mass Index or (BMI) with range from 16,3-26,5 Kg/mq and mean BMI value of 23,5+2,5 Kg/mq. Enrolled patients were subjected to laboratory assessment of cardiovascular risk factors like laboratory assessment of Methyl-Tetra-Hydro-Folate-Reductase or (MTHFR) and Homocysteine, Fibrinogen, D-Dimer, International Normalized Ratio (INR), Prothrombin Time (PT), activated Partial Thromboplastin Time (aPTT), Platelets (PLT), trombotic risk evaluation (CHA2DS2-VASc Score), and bledding risk evaluation (HAS-BLED Score). Before the insertion procedure of the PICC, single or duble lumen (Groshong or Power PICC type), the patient were subjected to a preliminary ultrasound and ech
Keywords
PICC, Peripherally inserted central catheters, Trombotic risk, CoRaMaPIcc protocol
Peripherally inserted central catheters articles Peripherally inserted central catheters Research articles Peripherally inserted central catheters review articles Peripherally inserted central catheters PubMed articles Peripherally inserted central catheters PubMed Central articles Peripherally inserted central catheters 2023 articles Peripherally inserted central catheters 2024 articles Peripherally inserted central catheters Scopus articles Peripherally inserted central catheters impact factor journals Peripherally inserted central catheters Scopus journals Peripherally inserted central catheters PubMed journals Peripherally inserted central catheters medical journals Peripherally inserted central catheters free journals Peripherally inserted central catheters best journals Peripherally inserted central catheters top journals Peripherally inserted central catheters free medical journals Peripherally inserted central catheters famous journals Peripherally inserted central catheters Google Scholar indexed journals Trombotic risk articles Trombotic risk Research articles Trombotic risk review articles Trombotic risk PubMed articles Trombotic risk PubMed Central articles Trombotic risk 2023 articles Trombotic risk 2024 articles Trombotic risk Scopus articles Trombotic risk impact factor journals Trombotic risk Scopus journals Trombotic risk PubMed journals Trombotic risk medical journals Trombotic risk free journals Trombotic risk best journals Trombotic risk top journals Trombotic risk free medical journals Trombotic risk famous journals Trombotic risk Google Scholar indexed journals CoRaMaPIcc protocol articles CoRaMaPIcc protocol Research articles CoRaMaPIcc protocol review articles CoRaMaPIcc protocol PubMed articles CoRaMaPIcc protocol PubMed Central articles CoRaMaPIcc protocol 2023 articles CoRaMaPIcc protocol 2024 articles CoRaMaPIcc protocol Scopus articles CoRaMaPIcc protocol impact factor journals CoRaMaPIcc protocol Scopus journals CoRaMaPIcc protocol PubMed journals CoRaMaPIcc protocol medical journals CoRaMaPIcc protocol free journals CoRaMaPIcc protocol best journals CoRaMaPIcc protocol top journals CoRaMaPIcc protocol free medical journals CoRaMaPIcc protocol famous journals CoRaMaPIcc protocol Google Scholar indexed journals Cardiovascular risk articles Cardiovascular risk Research articles Cardiovascular risk review articles Cardiovascular risk PubMed articles Cardiovascular risk PubMed Central articles Cardiovascular risk 2023 articles Cardiovascular risk 2024 articles Cardiovascular risk Scopus articles Cardiovascular risk impact factor journals Cardiovascular risk Scopus journals Cardiovascular risk PubMed journals Cardiovascular risk medical journals Cardiovascular risk free journals Cardiovascular risk best journals Cardiovascular risk top journals Cardiovascular risk free medical journals Cardiovascular risk famous journals Cardiovascular risk Google Scholar indexed journals High-risk bacteria patients articles High-risk bacteria patients Research articles High-risk bacteria patients review articles High-risk bacteria patients PubMed articles High-risk bacteria patients PubMed Central articles High-risk bacteria patients 2023 articles High-risk bacteria patients 2024 articles High-risk bacteria patients Scopus articles High-risk bacteria patients impact factor journals High-risk bacteria patients Scopus journals High-risk bacteria patients PubMed journals High-risk bacteria patients medical journals High-risk bacteria patients free journals High-risk bacteria patients best journals High-risk bacteria patients top journals High-risk bacteria patients free medical journals High-risk bacteria patients famous journals High-risk bacteria patients Google Scholar indexed journals Thromboplastin Time articles Thromboplastin Time Research articles Thromboplastin Time review articles Thromboplastin Time PubMed articles Thromboplastin Time PubMed Central articles Thromboplastin Time 2023 articles Thromboplastin Time 2024 articles Thromboplastin Time Scopus articles Thromboplastin Time impact factor journals Thromboplastin Time Scopus journals Thromboplastin Time PubMed journals Thromboplastin Time medical journals Thromboplastin Time free journals Thromboplastin Time best journals Thromboplastin Time top journals Thromboplastin Time free medical journals Thromboplastin Time famous journals Thromboplastin Time Google Scholar indexed journals venipuncture articles venipuncture Research articles venipuncture review articles venipuncture PubMed articles venipuncture PubMed Central articles venipuncture 2023 articles venipuncture 2024 articles venipuncture Scopus articles venipuncture impact factor journals venipuncture Scopus journals venipuncture PubMed journals venipuncture medical journals venipuncture free journals venipuncture best journals venipuncture top journals venipuncture free medical journals venipuncture famous journals venipuncture Google Scholar indexed journals endothelial damage articles endothelial damage Research articles endothelial damage review articles endothelial damage PubMed articles endothelial damage PubMed Central articles endothelial damage 2023 articles endothelial damage 2024 articles endothelial damage Scopus articles endothelial damage impact factor journals endothelial damage Scopus journals endothelial damage PubMed journals endothelial damage medical journals endothelial damage free journals endothelial damage best journals endothelial damage top journals endothelial damage free medical journals endothelial damage famous journals endothelial damage Google Scholar indexed journals coagulation articles coagulation Research articles coagulation review articles coagulation PubMed articles coagulation PubMed Central articles coagulation 2023 articles coagulation 2024 articles coagulation Scopus articles coagulation impact factor journals coagulation Scopus journals coagulation PubMed journals coagulation medical journals coagulation free journals coagulation best journals coagulation top journals coagulation free medical journals coagulation famous journals coagulation Google Scholar indexed journals septic vascular disease articles septic vascular disease Research articles septic vascular disease review articles septic vascular disease PubMed articles septic vascular disease PubMed Central articles septic vascular disease 2023 articles septic vascular disease 2024 articles septic vascular disease Scopus articles septic vascular disease impact factor journals septic vascular disease Scopus journals septic vascular disease PubMed journals septic vascular disease medical journals septic vascular disease free journals septic vascular disease best journals septic vascular disease top journals septic vascular disease free medical journals septic vascular disease famous journals septic vascular disease Google Scholar indexed journals
Article Details
1. Introduction
In hospital the absence of venous access led us to use a Peripherally Inserted Central Catheter (PICC) for continuous or discontinuous use for a period of time between 1 week to 3 months. The inserction of this device is significantly increased, because PICC is considered a safety method for long-term administration of Antibiotics, total parenteral nutrition or chemotherapy in frailty patients. In the 1070s , the poor quality of the materials (polyethylene or first-generation polyurethanes) caused an excessive level of complications. In the early 1990s, the new material (silicone) represented a new alternative for the progressive affirmation of peripheral central venous access. GAVeCeLT identified, in 2005, four possible causes of reduced use of PICC: (poor knowledge, by doctors and nurses, of the correct indications of such presidencies; the lack of training courses focused on the implant and the management of PICC; the poor diffusion of ecoguided technique, in other words;. Nurses opinion about the PICC implant (did not regard their professional profile). For these reasons, in recent years, PICCs are widely used particularly in North America and, most recently, in continental Europe [1].
1.1 PICC Classification
For the PICC timing on site the guidelines have distinguisced
- Short term CVC:<4 weeks (peripheral; material: teflon)
- Medium term CVC:<1-6 months (PICC, midline, cvc; material: silicone )
- Long-term CVC:>1-6 months CVCs (Groshong or Hickman) and fully implantable CVCs (port-a-cath)
- For the presence of antimicrobial or antiseptic drugs the guidelines have distinguisced dispositive with chlorhexidine/silver or sulfadiazine; minocycline/rifampicin; (to prevent infections) and platinum/silver [2].
1.2 Indication to PICC insertion
Directions for PICC The insertion of a PICC is consistent with: Need for infusion of acid solutions (pH<5) or basal (pH>9) or hypertonic (osmolarity>800 mOsm/l), or with irritating effect on the endothelium Need for measuring the Central Venus Pressure high risk of mechanical complications when a CVC is inserted in the internal or succulent jugular vein (obese patients, patients with anatomical and/or pathological disorders of the neck, patients with severe coagulopathy); presence of high risk of infectious complications if it is placed a traditional CVC (tracheotomy patients, immunodepressed or high-risk bacteria patients); Situations where it is logistically difficult or expensive to proceed to the placement of a traditional CVC (domicile, lack of a dedicated team, etc); need for central venous access for particularly prolonged time ('mid-term':<3 months); Need for medium central venous access (<3 months) in the patient to be treated either exclusively or in the field outside the hospital; Need for medium central venous access (<3 months) to be used either exclusively or discontinuously.
PICC is contraindicated in the following situations: Note or suspect bacterium or septicaemia; Prevents irradiation of the intended insertion site; Pregnant venous thrombosis episodes or vascular surgery interventions at the planned positioning site; Local factors that can prevent proper device stabilization or access (erythema, edema or eczema); Insufficient body size of the patient compared to the implant size. However, in patients undergoing infusional therapy over five days, an opportunity to use a long-term intravascular catheter, such as PICC, should be considered, based on evaluation criteria related to the characteristics of infusions over to the availability of the peripheral vascular vein, necessary to guarantee the therapeutic continuity and the efficiency of the infusive system [2].
1.3 Risk factors due to PICC implantation
Data presented in the literature underline that the incidence of complications associated with Picc insertion is between 3% and 38% of cases and the complications can be due to different factors, including the trauma of the vascular wall caused by the insertion of the catheter, the endothelial abrasion caused by the movement of the catheter or the Kinking due to the torsion of the catheter; and the pinch-off syndrome due to CVC compression between the clavicle and the first rib when PICC is inserted into the succlavia vein. Another aspect to consider is the thrombotic adjunctive risk due to the number of manipulations and the quality of the management procedure of the catheter.
2. Aim
The aim of the study is to evaluate the thrombotic risk associated with the positioning of the device. We have developed the CoRaMaPicc protocol which allows to reduce the thrombotic risk due to PICC insertion [3] in patients with high cardiovascular and trombotic risk.
3. Materials and Methods
We have enrolled 30 patients (18 males and 12 females with range age 30-99 yrs and mean age of 82+13.5 yrs). Enrolled patients have Body mass Index or BMI with range from 16.3-26.5 Kg/mq and mean BMI value of 23.5+2.5 Kg/mq. Enrolled patients were subjected to laboratory assessment of cardiovascular risk factors like laboratory assessment of Methyl-Tetra-Hydro-Folate-Reductase or (MTHFR) (Figure 1a) and Homocysteine (Figure 1b), Fibrinogen (Figure 2a), D-Dimer, International Normalized Ratio (INR) (Figure 2b), Prothrombin Time (PT), activated Partial Thromboplastin Time (aPTT), Platelets (PLT), trombotic risk evaluation (CHA2DS2-VASc Score) (Figure 3a and Table 1) and bledding risk evaluation (HAS-BLED Score) (Figure 3b and Table 2). All patients enrolled have high cardiovascular risk profile in 90% of cases and low or moderate risk profile in 10% of cases and have high value of blood pressure. All patients had undergone pre-insertion phase, at an ultrasound evaluation.
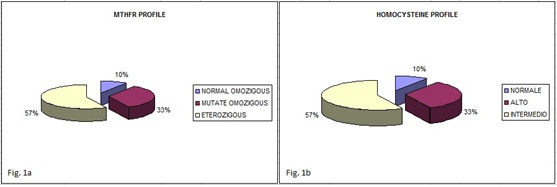
Figure 1a-1b: Methyl-Tetra-Hydro-Folate-Reductase (MTHFR) and Homocysteine profile of enrolled patients.
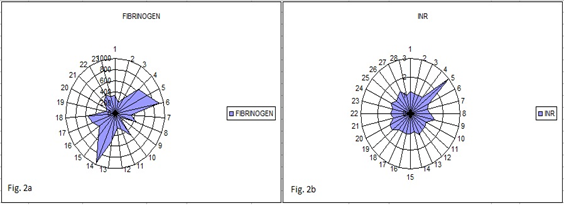
Figure 2a-2b: Fibrinogen and International Normalized Ratio (INR) profile of enrolled patients.
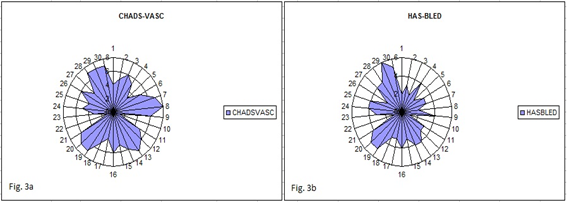
Figure 3a-3b: CHADS-VASC and HAS-BLED evaluation of enrolled patients.
|
Condition |
Points |
|
|
C |
Congestive heart failure (or Left ventricular |
1 |
|
H |
Hypertension: blood pressure consistently above |
1 |
|
A2 |
Age ≥75 years |
2 |
|
D |
Diabetes Mellitus |
1 |
|
S2 |
Prior Stroke/TIA/Thromboembolism |
2 |
|
V |
Vascular disease (e.g. peripheral artery |
1 |
|
A |
Age 65?74 years |
1 |
|
Sc |
Sex category (i.e. female sex) |
1 |
Table 1: HAS-BLED Score (acronym of the major
factors associated with ischaemic stroke risk in patients with atrial fibrillation).
| Condition | Points | |
| H | Hypertension -(systolic blood pressure >160 mmHg) | (Points: 1) |
| A | Abnormal renal function (defined as the presence of chronic dialysis or renal transplantation or serum creatinine 200µmol/L (>~2.3 mg/dL)) |
(Points: 1) |
| A | Abnormal liver function ( defined as chronic hepatic disease (eg. cirrhosis) or biochemical evidence of significant hepatic derangement (eg. bilirubin >2x upper limit of normal, in association with AST/ALT/ALP >3x upper limit normal) |
(Points: 1) |
| S | Stroke (Previous history of stroke) | (Points: 1) |
| B | Bleeding (Major bleeding history (anemia or predisposition to bleeding)) |
(Points: 1) |
| L | Labile INRs (refers to unstable/high INRs or poor time in therapeutic range(eg<60%)) |
(Points: 1) |
| E | Elderly (age >/= 65) | (Points: 1) |
| D | Drug Therapy (concomitant therapy such as antiplatelet agents, NSAID's) |
(Points: 1) |
| A | Alcohol intake (consuming 8 or more alcoholic drinks per week) | (Points: 1) |
Table 2: HAS-BLED Score (acronym of the major factors associated with bleeding risk in patients receiving oral anticoagulation).
3.1 Preliminary vein evaluation PICC positioning require, for a correct positioning, of the availability of a large gauge vein like Succlavia, internal or external jugular, femoral, Cephalic, external jugular vein, internal jugular vein or saphenous vein because alarge diameter of the vein reduce the endothelial damage and therefore reduce the risk of vascular disease and thrombotic events due to all causes. The recommended plant technique is that for percutaneous venipuncture [4, 5].
3.2 CoRaMaPiCC executive protocol
NAVAN recommends that the most appropriate position for the PICC tip is the lower third of the Upper Cave Vein near the junction between the latter and the right atrium. This tip position allows the catheter to float free within the lumen of the vein and reduce the percentage of complications such as thrombosis and infections [6]. A specific setting has been created to provide a better PICC positioning procedure with good patient comfort and to warranty an aseptic procedure. The skin preparation should be made with 2% chlorhexidine in an alcoholic solution by carefully scrubbing the area. The 2% chlorhexidine solution in 70% isopropyl alcohol isvused with a monodose applicator. The procedure for the implant was carried out in echo-guidated mode by preparing the ultrasound device with sterile washers.
3.3 Study of the patient's veins
The doctor with adeguate trainer period, after relative acquisition of certification and authorization, can study the veins of the arm and neck, with an ultrasound echo-doppler. The purpose of this examination is diagnostic and semiological, and gives us the possibility to underline the presence of a linear pathway of the vein of the arm (basilica, cephalic or brachial) in order to receive a venous catheter and esclude the presence of a thrombotic disease. Frequently, the veins of the dominant arm (predominates), have a greater caliber and the more frequent use during the movements reduce the risk of thrombosis. A second choice can be the brachial vein because it shows, generally, a smaller diameter than the basilica vein and has a greater number of valves. The third choice is the cephalic vein because it has a smaller linear pathway and a significant increase of number of the valves. In obese patients, however, the basilic vein becomes the third choice, because it is anatomically located more deeply than the cephalic vein, therefore the cephalic vein becomes the first choice (superficial vein).
The venipuncture site should be calculated by evaluating: the size of the vein, the number of the valves and the position of the vein compared to the artery. The insertion site of the catheter must be a sufficiently isolated area and it is adeguate to warranty a lower risk of infection. The diameter of the catheter should be about one-third of the diameter of the vein and, in cases where this rule cannot be observed, the catheter gauge should not exceed 50% of the diameter of the vein. The diameter of the venous vessel is expressed in mm and the catheter in Fr (French). The calculation is made considering that 1 mm equals to 3 Fr.
3.4 Ecoguided venipuncture
The venipuncture of a deep vein (basil or brachial) is the standard venous technique for positioning a PICC, associating with enormous benefits in terms of safety, cost-effectiveness and efficiency. ESPEN Guidelines- European Society of Parenteral and Enteral Nutrition, recommended the constant use of ECU and the use of Micro-insertion procedure (Seldinger modified technique). The appropriateness of the training received is the most important factor to determinate a successful procedure. Similar evaluations can be referred to the quality of the ultrasound examination that require a clear visualization of the median nerve and the quality of the micro-insertion kit. A too rigid metal guide or a mediocre micro-introducer are associated with failures even in expert hands.
When the catheter is positioned, it is easy to visualize into the vein with ECU and a simple compression with the hand or the ultrasound probe to facilitate the passage of the catheter from the succlavia vein to avoid the giugular vein involvment. Alternatively, if the patient is collaborative, it is possible to turn the head versus the operator side to have a good giugular vein compression and avoid malposition. After the maneuver, it is recommended to check with the ultrasonic probe the absence of the catheter in both jugular veins. This easy and simple procedure allows to immediately identify potential catheter malpositions. At the end of the implant operation, the patient was studied ultrasonically with a linear probe in a longitudinal section from the apex to the bases of the lung for pneumothorax search and with longitudinal and transverse section, integrating with the power-doppler method, to evaluate the possible malposition of the catheter into the vein. A Convex probe was used for the evaluation of the cardiac cavities using an epigastric window section (under the xifoid process) and a subcostal section. Finally, the radiography of the chest has been performed as well as guidelines to confirm the exact positioning of the device. At the end of these operations, the patient was subjected to follow-up for thrombosis due to high cardiovascular risk profile or endothelial damage related to the insertion procedure.
All patients received daily wash-out, with 5 cc (ml) of saline solution using a 10 cc (ml) syring type, into the PICC or an added wash-out after any pharmacological treatment. We have used standard instruments to register ECU. The statistical analysis was performed using Sigmastat Analysis Program (version 3.5) and Survival Analysis Test (Figure 4) to analize the number of the thrombotic events in all enrolled patients during the follow-up period.
3.5 Study design
All the patients provided a written informed consent. The Study is caratherized by a run-in period during which all patients have undergone laboratory exams pre-insertion procedure to underline a thrombotic disease and then have undergone a follow-up evaluation (Figure 4). The study started in July 2016. We have enrolled 30 patients (18 males and 12 females with range age 30-99 yrs and mean 82+13.5 yrs). An alteration of the coagulation values due to anticoagulant treatment are not a contraindication to the PICC implant but should be known to eventually make a more enduring and accurate compression of the venipuncture zone. The presence of thrombotic processes may be an absolute contraindication to the inserction of central venous system like the PICC. Presence of Pace Maker/ Defibrillator; It is necessary to ascertain whether the patient is carrying a Pace Maker or other device on one side of the trunk as it indicates the need to implant the venous access from the opposite side; Possible allergy to the administration of anesthetic. The presence of burns in the arms at the insertion level is an absolute contraindication to the PICC implant.
3.6 Study limitations
The limit of the study can be actually related to the number of patients (30 patients) enrolled in the CoRaMaPicc study and currently in follow up. This limitation imposes an obligation to describe the study data in terms of preliminary data requiring further investigation.
3.6.1 Study patients: Elegibility requirements at screening included age of at least 18 years. Exclusion criteria included presence of trombosis or septic vascular disease.
3.6.2 Study procedures: Patients who had no trombosis or septic vascular disease were assigned to the study group. Patients were evaluated during the first day (and during the follow-up phase if required) and then after 1-3 month.
3.7 Data management
The data collection was performed at the same time as also the informed consent request for positioning of peripheral venous access. Scale utilization has been aligned with the international referencing system for laboratory examinations and instrumental examinations.
3.7.1 Study outcome: The primary outcome was the trombotic risk evaluation after the dispositive inserction (Figure 4) with a clinical summary score (in a scale from 0 to 1, with lower scores indicating absence of trombosis due to the implantation procedure) in patients with different genetic profile (Figure 1a-b) and CHAD-VASC OR HASBLED score (Figure 3a-b).
3.7.2 Statistical analysis: The data collection has been done by integrating the paper material with a database specifically created for inserting the laboratory data and the instrumental examinations associated with the procedure. The need to create a database is linked to the ability to perform preliminary data analysis using simple "filter" functions and to control the integrity of the data entered and to export the data in a mode compatible with the statistical analysis software performed with Sigmastat VERSION 3.5 for WindowsXp.
3.8 Data elaboration
Preliminary data has shown that genetic factors, while having an internationally recognized prothrombotic role, are not alone sufficient to discriminate against post-implant thrombotic risk, but must be framed in the primum movens that may be sought in mechanical and/or chemical endothelial traumas And in inadequate device management (especially for PICCs, which, being not tunneled, are subjected to a higher risk of thrombotic complications) [7]. We used Survival Analysis test (Figure 4) to analize data related to the follow-up period.
4. Results
4.1 Study patients
From June 2016, through December 2016, a total of 30 patients entered in the run-in period. All patients fulfilled the criteria for the study. No patients underwent randomization erroneously or were enrolled at sites that were closed owing to serious Good Clinical Practice Violations. Most patients were receiving a recommended pharmacologic therapy for hypertension disease. At the end of the treatment we obtained a statistically significant correlation about improvement of use of CoraMaPiCC protocol and low presence of procedural complication confronted with data reported in the literature.
4.2 Study drug administration and follow-up
Except for discontinuations owing to death, the study drugs was continued in all patients. The median duration of follow-up was 3 month (2 month+1 month). This value was related to the clinical conditions and the presence of patient and /or caregiver compliance to the follow-up phase.
4.3 Study outcome
All patients enrolled in the CoRaMaPiCC protocol show a reduction of the trombotic risk if compared with data presented in the literature (Gonsalves, Eschei et al. 2003 and Ong, Gibbs et al. 2006), in both group with normal or mutate MTHFR and Homocysteine profile (Figure 1a-b) and different thrombotic or bledding score evaluated with CHADSVASC and HASBLED score (Figure 3a-b).
4.4 Safety
Treatment was effective and well-tolerated when used in routine clinical practice.
5. Results
The CoRaMaPicc protocol allows, based on the estimation of the preliminary data, to clearly minimize the trombotic risk. Our study was designed to provide evidence to support the efficacy of the CoRaMaPiCC protocol in the management of frailty patients with comorbidity and absence of vein access [8]. Data shows that the treatment improves the patient’s quality of life, reduce the hospedalization period and, therefore, improves the patient’s adherence to therapy. This experience led us to use CoRaMaPiCC protocol in patients that have the need to undergo a PICC insertion. The protocol was efficacy and well-tollerated when used in routine clinical practice.
The positioning of the device by ultrasound study consent an adeguate evaluation pre and post procedure. A radiographic control has allowed that the control procedures can have some limitations. It is beneficial to integrate the CoRaMaPiCC Protocol with the Intracavitary ECG (not available during the study) in the presence of contraindications for ultrasound evaluation (meteorism) or radiographic evaluation (ascites in forced decupitus). In the first case the ultrasound examination was replaced by the radiographic evaluation. In the second case is not possible to execute a radiographic control, therefore, the evaluation of the functionality of the device was deduced using the only ultrasound approach, with the limits of the ultrasound method. In effect in a patient, an adequate Thorax radiographic assessment was not possible because of the poor collaboration due to the presence of ascites (even after drainage with 5000cc evacuation paracentesis) and the X-ray procedure can be performed in the only lateral decoupled to evoid dyspnoea (decupid on the right side).
6. Discussion
Intravenous therapy can be administered using different intravascular devices with specific indications that must be identified. The use of the Peripherally Inserted Central Catheter (PICC) has been significantly increased, being considered a safe method for long-term administration of antibiotics, chemotherapy [9], parenteral nutrition, both in the hospital and in the treatment house. The PICC is a central venous system inserted peripherally for continuous and discontinuous use for a period of time ranging from 1 week to 3 months. It is made up of last-generation high-biocompatibility, silicone or polyurethane materials, of 40-60 cm in length, ranging between 16 and 25 G or 2 and 5 Fr. The PICC allows all the typical uses of central venous catheters ( CVC), inserted in succlavia and giugulare, but with respect to these, has the following advantages of avoiding the risk of mechanical insertion complications, typical of direct central venous puncture (eg hemo-pneumothorax), low risk of bacterial complications, low risk of central venous thrombosis, it can be positioned by medical or nursing personnel with adequate trainer period without an anesthesiologic or surgical specialistic formation, it can also be used discontinuously, without increasing the risk of obstructive or infectious complications. From the data in the literature, the presence of non-eliminable risk factors (i.e. anatomical configuration of the vein) play a secondary role in the evaluation of the procedural risk factors.
The gold standard to certify the correct positioning of the tip of the device results is a RX chest post-implant. During the study period (1 year), the PICCs were removed for death (7 patients; 4 patients for irreversible heart disease, 1 patient for cardiogenic shock, 1 patient for septic shock [10], 1 patient for Creutzfeld-Jacob disease, 1 patient for spontaneously remotion due to the low compliance of the patient. In the other cases, the PICC were removed for end of therapy (22 patients) (Figure 4). Only a scrupolous PICC insertion protocol and a meticulous management of the dispositive (like a wash-out with 5 cc (ml) of saline solution using a 10 cc (ml) syringe after any pharmacological treatment) can minimize the thrombotic risk respect to the data reported in the international literature.
7. Conclusion
The CoRaMaPicc protocol, which we have elaborated, allows, based on the estimation of preliminary data, to minimize the trombotic risk. Further studies are needed to expand the number of enrolled patients and to prolong their follow-up period. Our data gives comfortable results but further evaluation are needed to have conclusive results.
Acknowledgments
The Authors are particularly grateful to Dicembre Stella for English translation and Marchitto Lino, Maisano Carla Maria and Marchitto Federica for organizational aspects.
References
- Dougherty L. The Management of intravenous therapy in palliative Care. Int J of Palliative Nursing (1999).
- Yamamoto AJ, Solomon JA, Soulen MC, et al. Sutureless securement device reduces complications of peripherally inserted central venous catheters. J Vasc Interv Radiol (2001).
- Grove JR. Venous thrombosis related to peripherally inserted central catheters. J Vasc Interv Radiol 11 (2000): 837-840.
- Ong B, Gibbs H, Catchpole I, et al. Peripherally inserted central catheters and upper extremity deep vein thrombosis. Australasian Radiology 50 (2006): 451-454.
- McGee DC, Gould MK. Preventing complications of central venous catheterization. N Engl J Med 348 (2003):1123-1133.
- Langston CS. The aberrant central venous catheter and its complications. Radiology 100 (1971): 55.
- Van Rooden CJ, Shippers EF, Barge RM, et al. Infectious complications of central venous catheters increase the risk of catheter-related thrombosis in hematology patients: a prospective study. J Clin Oncol 23 (2005): 2655-2660.
- Lee AY, Levine MN, Butler G, et al. Incidence, risk factors, and outcomes of catheter-related thrombosis in adult patients with cancer. Journal of Clinical Oncology 24 (2006): 1404-1408.
- van Rooden CJ, Schippers EF, Barge RM, et al. Infectious complications of central venous catheters increase the risk of catheter-related thrombosis in hematology patients: a prospective study. J Clin Oncol 23 (2005): 2655-2660.
- Levine M, Kakkar AK. Catheter-Associated Thrombosis: thromboprophylaxis or not? Journal of Clinical Oncology 23 (2005): 4006-4008.
