Stent Placement in the Hepatic Artery with Anatomical Variant for Treatment of A Massive Ulcer Bleeding
Article Information
Van Dijk B MD1*, de Vos tot Nederveen Cappel WH MD PhD1, van Hasselt BAAM MD2, van Westreenen HL MD PhD3, Nieuwenhuijs VB MD PhD3
1Gastroenterology and Hepatology at Isala Hospital, Zwolle, The Netherlands
2Interventional radiology at Isala Hospital, Zwolle, The Netherlands
3Abdominal surgery at Isala Hospital, Zwolle, The Netherlands
*Corresponding Author: Van Dijk B, Gastroenterology and Hepatology at Isala Hospital, Zwolle, The Netherlands
Received: 25 August 2021; Accepted: 20 September 2021; Published: 21 October 2021
Citation: Van Dijk B, de Vos tot Nederveen Cappel WH, van Hasselt BAAM, van Westreenen HL, Nieuwenhuijs VB. Stent Placement in the Hepatic Artery with Anatomical Variant for Treatment of A Massive Ulcer Bleeding. Archives of Clinical and Medical Case Reports 5 (2021): 721-723.
View / Download Pdf Share at FacebookAbstract
A 54-year-old man, presented with melaena after a recent bowel perforation resulting in sigmoid resection. The gastroduodenoscopy showed a large clot and active bleeding in the postpyloric duodenum without the opportunity of obtaining endoscopic hemostasis. A diagnostic angiography was attempted, but no blush was seen. The next day radiologic coiling took place. Unfortunately long term hemostasis was not achieved. A second gastroscopy was performed and a postpyloric ulcer with a large pulsating blood vessel was seen. Hemostasis was attempted by both endoscopic clipping and radiological coiling of the target vessels. An angiography with coiling was attempted. It was technically impossible to coil all the vessels due to an anatomic variation. In order to prevent to sacrify the hepatic artery by coiling the entire hepatic artery, we successfully tried a unique approach to place a radiologic covered stent in the common hepatic artery to cover the origin of the gastroduodenal artery.
Keywords
Hemorrhage; Vascular malformations; Artery; Gastrointestinal; Arterial intervention; Radioembolization; Stenting; Stent graft
Hemorrhage articles; Vascular malformations articles; Artery articles; Gastrointestinal articles; Arterial intervention articles; Radioembolization articles; Stenting articles; Stent graft articles
Hemorrhage articles Hemorrhage Research articles Hemorrhage review articles Hemorrhage PubMed articles Hemorrhage PubMed Central articles Hemorrhage 2023 articles Hemorrhage 2024 articles Hemorrhage Scopus articles Hemorrhage impact factor journals Hemorrhage Scopus journals Hemorrhage PubMed journals Hemorrhage medical journals Hemorrhage free journals Hemorrhage best journals Hemorrhage top journals Hemorrhage free medical journals Hemorrhage famous journals Hemorrhage Google Scholar indexed journals Vascular malformations articles Vascular malformations Research articles Vascular malformations review articles Vascular malformations PubMed articles Vascular malformations PubMed Central articles Vascular malformations 2023 articles Vascular malformations 2024 articles Vascular malformations Scopus articles Vascular malformations impact factor journals Vascular malformations Scopus journals Vascular malformations PubMed journals Vascular malformations medical journals Vascular malformations free journals Vascular malformations best journals Vascular malformations top journals Vascular malformations free medical journals Vascular malformations famous journals Vascular malformations Google Scholar indexed journals Artery articles Artery Research articles Artery review articles Artery PubMed articles Artery PubMed Central articles Artery 2023 articles Artery 2024 articles Artery Scopus articles Artery impact factor journals Artery Scopus journals Artery PubMed journals Artery medical journals Artery free journals Artery best journals Artery top journals Artery free medical journals Artery famous journals Artery Google Scholar indexed journals Gastrointestinal articles Gastrointestinal Research articles Gastrointestinal review articles Gastrointestinal PubMed articles Gastrointestinal PubMed Central articles Gastrointestinal 2023 articles Gastrointestinal 2024 articles Gastrointestinal Scopus articles Gastrointestinal impact factor journals Gastrointestinal Scopus journals Gastrointestinal PubMed journals Gastrointestinal medical journals Gastrointestinal free journals Gastrointestinal best journals Gastrointestinal top journals Gastrointestinal free medical journals Gastrointestinal famous journals Gastrointestinal Google Scholar indexed journals Arterial intervention articles Arterial intervention Research articles Arterial intervention review articles Arterial intervention PubMed articles Arterial intervention PubMed Central articles Arterial intervention 2023 articles Arterial intervention 2024 articles Arterial intervention Scopus articles Arterial intervention impact factor journals Arterial intervention Scopus journals Arterial intervention PubMed journals Arterial intervention medical journals Arterial intervention free journals Arterial intervention best journals Arterial intervention top journals Arterial intervention free medical journals Arterial intervention famous journals Arterial intervention Google Scholar indexed journals treatment articles treatment Research articles treatment review articles treatment PubMed articles treatment PubMed Central articles treatment 2023 articles treatment 2024 articles treatment Scopus articles treatment impact factor journals treatment Scopus journals treatment PubMed journals treatment medical journals treatment free journals treatment best journals treatment top journals treatment free medical journals treatment famous journals treatment Google Scholar indexed journals CT articles CT Research articles CT review articles CT PubMed articles CT PubMed Central articles CT 2023 articles CT 2024 articles CT Scopus articles CT impact factor journals CT Scopus journals CT PubMed journals CT medical journals CT free journals CT best journals CT top journals CT free medical journals CT famous journals CT Google Scholar indexed journals Dermoid Cyst articles Dermoid Cyst Research articles Dermoid Cyst review articles Dermoid Cyst PubMed articles Dermoid Cyst PubMed Central articles Dermoid Cyst 2023 articles Dermoid Cyst 2024 articles Dermoid Cyst Scopus articles Dermoid Cyst impact factor journals Dermoid Cyst Scopus journals Dermoid Cyst PubMed journals Dermoid Cyst medical journals Dermoid Cyst free journals Dermoid Cyst best journals Dermoid Cyst top journals Dermoid Cyst free medical journals Dermoid Cyst famous journals Dermoid Cyst Google Scholar indexed journals Radioembolization articles Radioembolization Research articles Radioembolization review articles Radioembolization PubMed articles Radioembolization PubMed Central articles Radioembolization 2023 articles Radioembolization 2024 articles Radioembolization Scopus articles Radioembolization impact factor journals Radioembolization Scopus journals Radioembolization PubMed journals Radioembolization medical journals Radioembolization free journals Radioembolization best journals Radioembolization top journals Radioembolization free medical journals Radioembolization famous journals Radioembolization Google Scholar indexed journals Stent graft articles Stent graft Research articles Stent graft review articles Stent graft PubMed articles Stent graft PubMed Central articles Stent graft 2023 articles Stent graft 2024 articles Stent graft Scopus articles Stent graft impact factor journals Stent graft Scopus journals Stent graft PubMed journals Stent graft medical journals Stent graft free journals Stent graft best journals Stent graft top journals Stent graft free medical journals Stent graft famous journals Stent graft Google Scholar indexed journals
Article Details
1. Case Report
A 54-year-old man, presented with melaena after a recent scrotal hernia correction complicated by bowel perforation resulting in sigmoid resection. The gastroduodenoscopy showed a large clot and active bleeding in the postpyloric duodenum without the opportunity of obtaining endoscopic hemostasis.
A CT-angiography was performed and demonstrated a blush into the duodenum. A diagnostic angiography was attempted, but no blush was seen. The next day, the patient was hypotensive and radiologic coiling took place. Unfortunately long term hemostasis was not achieved; fluid resuscitation and blood transfusions were needed to stabilize the patient. A second gastroscopy was performed and a postpyloric ulcer with a large pulsating blood vessel was seen. Endoscopic treatment with adrenaline and the goldprobe was performed, which provoked recurrent bleeding. Hemostasis was attempted by both endoscopic clipping and radiological coiling of the target vessels.
An angiography with coiling was attempted. It was technically impossible to coil all the vessels due to an anatomic variation (shown in figure 1). The short origin of the gastroduodenal artery arose from the common hepatic artery which was displaced to the superior mesenteric artery. In order to prevent to sacrify the hepatic artery by coiling the entire hepatic artery, we successfully tried a unique approach to place a radiologic covered stent (Gore Viabahn 8 × 50 mm, shown in Figure 2) in the common hepatic artery to cover the origin of the gastroduodenal artery. Eight weeks later an outpatient gastroscopy showed a healed ulcer.
Stenting is not the initial therapy, but should be considered if endoscopic treatment or coiling cannot arrest the bleeding and surgery is detrimental.
References
None.

Figure 1: 3D reconstruction of the anatomical variation of the vascular supply.
1 Truncus coelicus; 2 Superior mesenteric artery; 3 Common hepatic artery; 4 Right renal artery
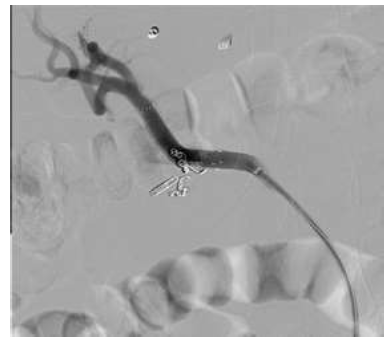
Figure 2: Hemostasis achieved with the Covered stent (Gore Viabahn, 8 × 50 mm).
