Status of Vitamin D in Women with Uterine Fibroid and Impact of Vitamin D Supplementation
Article Information
Prof. Shiuly Chowdhury1*, Dr. Shahjada Selim2, Dr. Menhazul Islam3, Dr. Shuva Shrestha4
1Professor, Department of Obstetrics and Gynecology, Bangabandhu Sheikh Mujib Medical University (BSMMU), Dhaka, Bangladesh
2Associate Professor, Department of Endocrinology, Bangabandhu Sheikh Mujib Medical University (BSMMU), Dhaka, Bangladesh
3Assistant Professor, Department of Radiology and Imaging, Bangabandhu Sheikh Mujib Medical University (BSMMU), Dhaka, Bangladesh
4Assistant Professor, Department of Obstetrics and Gynecology, Bangabandhu Sheikh Mujib Medical University (BSMMU), Dhaka, Bangladesh
*Corresponding Author: Prof. Shiuly Chowdhury, Professor, Department of Obstetrics and Gynecology, Bangabandhu Sheikh Mujib Medical University (BSMMU), Dhaka, Bangladesh.
Received: 20 July 2022; Accepted: 27 July 2022; Published: xx October 2022
Citation:
Prof. Shiuly Chowdhury, Dr. Shahjada Selim, Dr. Menhazul Islam, Dr. Shuva Shrestha. Status of Vitamin D in Women with Uterine Fibroid and Impact of Vitamin D Supplementation Journal of Obstetrics and Gynecology Research 5 (2022): 311-318.
View / Download Pdf Share at FacebookAbstract
Background
Uterine fibroids, also known as leiomyomas, are benign smooth muscle tumors of the uterus. The exact cause of uterine fibroids is indistinct. However, fibroids appear to be partly determined by hormone levels. There is a high prevalence of Vitamin D deficiency for uterine fibroids. Vitamin D from food or from skin synthesis by sunshine becomes biologically inactive. It is activated by two protein enzyme hydroxylation steps. The first in the liver and the second in the kidney. As Vitamin D can be synthesized, it is considered a prohormone. Vitamin D is taken to the liver where it is transformed into 25[OH] D.
Objective
The objective of this study was to determine the impact of Vitamin D supplementation in women with fibroids uterus. Methods: This interventional study was conducted in the department of obstetrics & gynecology, BSMMU, Dhaka, Bangladesh. A purposive sampling method was done. A total of 95 patients diagnosed as uterine fibroids with Vitamin D deficiency were included in the study. BMI was measured and the size of the fibroid was determined by ultrasonography and serum Vitamin D level was estimated. Vitamin D was supplemented to the participants. Then repeat ultrasonography and serum Vitamin D level were done after 3 months, to the assessment of vitamin impact. Regression of the size of the fibroid was done. Results: The mean age was 37.31±7.10 years. The majority of the participants were housewives 67.4%. Mean Vitamin D was 21.71±7.32, BMI 27.96±4.72. At the initial stage, among total study population in 11.6% (n=11), 47.4% (n=45) and 41.0% (n=39) patients we found <2.5cm(Small), 2.5-4.9cm (Medium) and (≥5cm (Large) sized fibroids respectively. The mean size of fibroids in a total of 95 patients was 4.99 ± 2.59 and after Vitamin D sup
Keywords
Uterine fibroid, vitamin D, 25[OH] D
Uterine fibroid articles Uterine fibroid Research articles Uterine fibroid review articles Uterine fibroid PubMed articles Uterine fibroid PubMed Central articles Uterine fibroid 2023 articles Uterine fibroid 2024 articles Uterine fibroid Scopus articles Uterine fibroid impact factor journals Uterine fibroid Scopus journals Uterine fibroid PubMed journals Uterine fibroid medical journals Uterine fibroid free journals Uterine fibroid best journals Uterine fibroid top journals Uterine fibroid free medical journals Uterine fibroid famous journals Uterine fibroid Google Scholar indexed journals vitamin D articles vitamin D Research articles vitamin D review articles vitamin D PubMed articles vitamin D PubMed Central articles vitamin D 2023 articles vitamin D 2024 articles vitamin D Scopus articles vitamin D impact factor journals vitamin D Scopus journals vitamin D PubMed journals vitamin D medical journals vitamin D free journals vitamin D best journals vitamin D top journals vitamin D free medical journals vitamin D famous journals vitamin D Google Scholar indexed journals 25[OH] D articles 25[OH] D Research articles 25[OH] D review articles 25[OH] D PubMed articles 25[OH] D PubMed Central articles 25[OH] D 2023 articles 25[OH] D 2024 articles 25[OH] D Scopus articles 25[OH] D impact factor journals 25[OH] D Scopus journals 25[OH] D PubMed journals 25[OH] D medical journals 25[OH] D free journals 25[OH] D best journals 25[OH] D top journals 25[OH] D free medical journals 25[OH] D famous journals 25[OH] D Google Scholar indexed journals UVB rays articles UVB rays Research articles UVB rays review articles UVB rays PubMed articles UVB rays PubMed Central articles UVB rays 2023 articles UVB rays 2024 articles UVB rays Scopus articles UVB rays impact factor journals UVB rays Scopus journals UVB rays PubMed journals UVB rays medical journals UVB rays free journals UVB rays best journals UVB rays top journals UVB rays free medical journals UVB rays famous journals UVB rays Google Scholar indexed journals parathyroid hormone articles parathyroid hormone Research articles parathyroid hormone review articles parathyroid hormone PubMed articles parathyroid hormone PubMed Central articles parathyroid hormone 2023 articles parathyroid hormone 2024 articles parathyroid hormone Scopus articles parathyroid hormone impact factor journals parathyroid hormone Scopus journals parathyroid hormone PubMed journals parathyroid hormone medical journals parathyroid hormone free journals parathyroid hormone best journals parathyroid hormone top journals parathyroid hormone free medical journals parathyroid hormone famous journals parathyroid hormone Google Scholar indexed journals Endocrine articles Endocrine Research articles Endocrine review articles Endocrine PubMed articles Endocrine PubMed Central articles Endocrine 2023 articles Endocrine 2024 articles Endocrine Scopus articles Endocrine impact factor journals Endocrine Scopus journals Endocrine PubMed journals Endocrine medical journals Endocrine free journals Endocrine best journals Endocrine top journals Endocrine free medical journals Endocrine famous journals Endocrine Google Scholar indexed journals pelvic articles pelvic Research articles pelvic review articles pelvic PubMed articles pelvic PubMed Central articles pelvic 2023 articles pelvic 2024 articles pelvic Scopus articles pelvic impact factor journals pelvic Scopus journals pelvic PubMed journals pelvic medical journals pelvic free journals pelvic best journals pelvic top journals pelvic free medical journals pelvic famous journals pelvic Google Scholar indexed journals fibroids articles fibroids Research articles fibroids review articles fibroids PubMed articles fibroids PubMed Central articles fibroids 2023 articles fibroids 2024 articles fibroids Scopus articles fibroids impact factor journals fibroids Scopus journals fibroids PubMed journals fibroids medical journals fibroids free journals fibroids best journals fibroids top journals fibroids free medical journals fibroids famous journals fibroids Google Scholar indexed journals ultrasonography articles ultrasonography Research articles ultrasonography review articles ultrasonography PubMed articles ultrasonography PubMed Central articles ultrasonography 2023 articles ultrasonography 2024 articles ultrasonography Scopus articles ultrasonography impact factor journals ultrasonography Scopus journals ultrasonography PubMed journals ultrasonography medical journals ultrasonography free journals ultrasonography best journals ultrasonography top journals ultrasonography free medical journals ultrasonography famous journals ultrasonography Google Scholar indexed journals transvaginal articles transvaginal Research articles transvaginal review articles transvaginal PubMed articles transvaginal PubMed Central articles transvaginal 2023 articles transvaginal 2024 articles transvaginal Scopus articles transvaginal impact factor journals transvaginal Scopus journals transvaginal PubMed journals transvaginal medical journals transvaginal free journals transvaginal best journals transvaginal top journals transvaginal free medical journals transvaginal famous journals transvaginal Google Scholar indexed journals
Article Details
Introduction
Vitamin D, In the early 1900s, it was thought to be a vitamin, but scientists today consider it to be a prohormone [1]. Humans obtain 80% of their vitamin D from UVB rays via their skin and 20% from meals. [2] 7-dehydrocholesterol is converted to pre-vitamin D3 by sunlight, which is then isomerized to vitamin D3 in the skin. The liver is actually responsible for the conversion of vitamin D into the primary circulating metabolite known as 25-hydroxyvitamin D (25[OH]D or calcidiol). 25[OH] D is transported from the liver to the kidneys, where it is converted into 1, 25-dihydroxyvitamin D (1, 25[OH]2D or calcitriol), the active form of vitamin D. This kidney conversion is controlled by plasma levels of parathyroid hormone as well as serum calcium and phosphorus level. The serum level of the inactive metabolite 25[OH]D is presently recommended to acquire because it provides a more accurate indicator of the state of vitamin D than does the serum level of 1, 25[OH] D. [3,4] The Endocrine Society defines vitamin D insufficiency as a 25(OH)D level below 20 ng/mL as the most prevalent sign. A vitamin D level of 21 to 29 ng/mL is regarded inadequate, but a level of 30 ng/mL or more is considered adequate. Vitamin D toxicity may develop if the 25[OH]D level is more than 150 ng/mL. [4] Uterine fibroids are a growth of smooth muscle cells encased in a pseudocapsule of compressed muscle fibers. They're frequently found by accident during routine physical examinations, such as a pelvic exam, ultrasound, or other imaging procedure. In the 1970s, ultrasonography was used to diagnose fibroids, and when transvaginal scans were developed in the 1980s, this became the gold standard. Ultrasonography is now the imaging method of choice for the identification and assessment of uterine fibroids. Ultrasonography often reveals fibroids as well-defined, hypoechoic masses that create varying acoustic shadowing.
Depending on the degree of calcification or/and the quantity of fibrous tissue, however, leiomyomas may exhibit varying echogenicity, often hyperechogenic or isoechogenic. [5,6] Symptoms are almost never linked with uterine fibroids that are small in size. Recent studies have shown that women who have hypertension have an increased chance of developing fibroid tumors, cytokine release or smooth muscle damage may be the cause. [7] Sometimes, fibroids in the uterus can be made worse by a number of symptoms, such as menstrual problems, pressure symptoms, feeling full, frequent urination, bowel problems, or pelvic pain. So definite treatment methods are essential according to the symptoms and condition of the patients. The specific cause of uterine fibroids is uncertain, estrogen and progesterone are largely considered in fibroid formation. [8] When it comes to gynecological problems, fibroids account for a large portion of the hospitalizations due to hysterectomy (both abdominal and vaginal). [9,10] Additionally, it is by far the most common choice offered to a woman who have just finished giving birth. If uterine fibroids-related symptoms can be treated less invasively, many women may want to keep the uterus for future reproduction. Women who want to protect their fertility in the future often choose to myomectomy as one of the more conservative treatment options. [11] Recent research from 3 North African independent groups, the eastern United States, and central Europe shows a link between low serum vitamin D levels and a higher risk of uterine fibroids. This is not a minor finding, but one that may impact clinical practice and enhance the global treatment of this prevalent illness. Preclinical evidence reveals that vitamin D inhibits the proliferation of human fibroid cells in vitro in a dose-dependent manner, as shown by a recent research.[12] Women from the eastern United States and Italian women were found to have similar findings.[13,14] Estrogen and progesterone, through their nuclear receptors, play important roles in fibroid development and function. [12] To confirm vitamin D3's regulatory role in uterine fibroid steroid receptor expression, Western blot analysis was performed. Results showed that vitamin D3 reduced the growth of fibroid tumors in Eker rats by decreasing ESR1 protein expression and boosting VDR protein expression, as well as decreasing the expression of progesterone receptors PGR-A and PGR-B. [15] In total, 53 women with small burden uterine fibroids (50 mm in diameter and less than 4 tumors) got vitamin D treatment, which restored proper vitamin D serum concentrations. Vitamin D slowed illness progression in these women. In women with uterine fibroids, baseline 25-hydroxy-cholecalciferol (25-OH-D3) concentration was negatively correlated with both the biggest fibroid volume (r=0.18, P=0.01) and overall fibroid volume (r=0.19, P=0.01). There was no association between 25- OH-D3 levels at baseline and the number of fibroids per patient (r = 0.10, P = 0.16). After 3 months of supplementation, women had a substantial rise in 25- OH-D3 serum level and a decreased incidence of "progression to severe illness." This was the first human study indicating vitamin D's benefits in fibroid control. [15] As surgical management of fibroid uterus is associated with morbidity and mortality, it is important to look for new ways to treat fibroids without surgery and figure out ways to stop them from happening.
Materials and Methods
This interventional study has been conducted at the Department of Obstetrics & Gynecology, (BSMMU), Dhaka, Bangladesh. Consecutively all the women attending the OPD of BSMMU having a radiological diagnosis of fibroid uterus (size<2.5cm in diameter and <4m in number), have been approached to participate.
Finally, in total 95 women had been recruited who fulfilled the inclusion criteria and signed the informed consent form. Patients with heavy menstrual bleeding (>80.0 mL), pelvic discomfort, severe anemia, infertility, or other indications for surgery, complicated with myoma degeneration and adenomyosis, malabsorption syndrome, planning of pregnancy in near future, acute crisis, history of the previous myomectomy, history of total thyroidectomy, chronic systemic disease, any malignancy, menopausal women, pregnant and lactating women, history of or current vitamin D supplementation, abortion or miscarriage during the previous six months, and usage of oral contraceptives or hormonal drugs within the last three months were excluded from the study. Socio- demographic, personal habits, and family information were collected through face-to-face interviews and disease-specific data were recorded from the register. Bodyweight, height, and waist circumference were also recorded. Then vitamin D was supplemented in the prescribed dose in Vitamin D insufficient women. After three months, a follow-up ultrasonography was performed to see if Vitamin D had any effect on the fibroid's shrinkage. The study's goals and methods were explained to the participants. Ethical committee clearance was obtained from the institution. HPLC was used to determine the amount of vitamin D3.
Results
|
Characteristics |
Frequency (N=95) |
Percentage (%) |
Mean ±SD |
|
Age in years |
|||
|
20 - 30 yrs. |
17 |
17.9 |
37.31±7.10 |
|
31 - 45 yrs. |
69 |
72.6 |
|
|
>45 yrs. |
9 |
9.5 |
|
|
Education |
|||
|
Illiterate |
13 |
13.7 |
|
|
Primary |
25 |
26.3 |
|
|
SSC |
22 |
23.2 |
|
|
HSC |
20 |
21.1 |
|
|
Graduate or Above |
15 |
15.7 |
|
|
Occupation |
|||
|
House wife |
64 |
67.4 |
|
|
Service |
14 |
14.7 |
|
|
Student |
8 |
8.4 |
|
|
Others |
9 |
9.5 |
|
|
Residence |
|||
|
Urban |
53 |
55.8 |
|
|
Rural |
42 |
44.2 |
|
|
DMFI |
|||
|
10,000-20,000 |
32 |
33.7 |
29074±12522 |
|
21,000-30,000 |
36 |
37.9 |
|
|
>30,000 |
27 |
28.4 |
|
|
Marital Status |
|||
|
Unmarried |
6 |
6.3 |
|
|
Married |
86 |
90.5 |
|
|
Widow/Divorce |
3 |
3.2 |
|
|
Number of Parity |
|||
|
0 |
23 |
24.2 |
|
|
1 |
19 |
20 |
|
|
≥2 |
53 |
55.8 |
|
Table 1: Sociodemographic characteristics of the participants (N=95).
Table 1 showed, according to the age group highest number of participants, 69(72.6%) were from the 31-45 years age group. Participant’s mean age was 37.31±7.10. In educational status, highest 25(26.3%) were primary level educated followed by 22(23.2%) who completed SSC. The majority of the participants
were housewives 64(67.4%), followed by 14(14.7%) were service holders. Regarding the patient’s marital status, 86(90.5%) were married 6(6.3%) were unmarried and 3(3.2%) were widows/divorced.
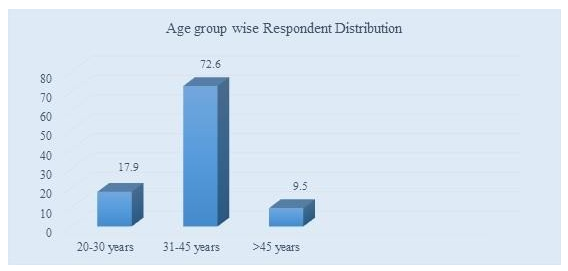
Figure 1: Age group wise Respondents Distribution
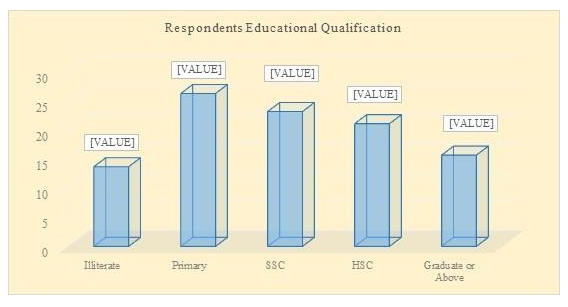
Figure 2: Respondents Educational Qualification Status.
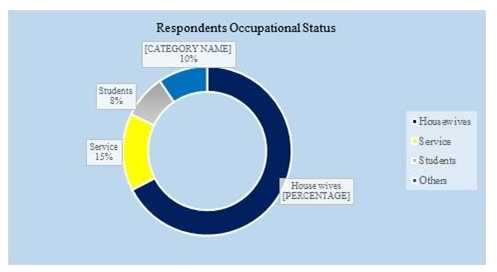
Figure 3: Respondent’s Occupation Wise Distribution.
Table 2 showed that the mean (±SD) fibroid was 4.97 ±
2.56 and after having Vitamin D fibroid mean was 3.09
± 0.68. BMI 27.96±4.71and most of them where medium anemia patients were 40(42.1%).
|
Characteristics |
Frequency (n) |
Percentage (%) |
Mean ±SD |
|
Fibroid Size |
|||
|
Small (<2.5 cm) |
11 |
11.6 |
4.99 ± 2.59 |
|
Medium (2.5- 4.9 cm) |
45 |
47.4 |
|
|
Large (≥5 cm) |
39 |
41 |
|
|
Follow up Fibroid Size |
|||
|
Small (<2.5cm) |
20 |
21.1 |
4.77±3.04 |
|
Medium (2.5- 4.9 cm) |
42 |
44.2 |
|
|
Large (≥5cm) |
33 |
34.7 |
|
|
BMI |
|||
|
Underweight |
1 |
1 |
27.96±4.72 |
|
Normal |
24 |
25.3 |
|
|
Overweight |
41 |
43.2 |
|
|
Obese |
29 |
30.4 |
|
|
Anemia* |
|||
|
Mild |
35 |
36.8 |
|
|
Moderate |
40 |
42.1 |
|
|
Severe |
20 |
21.1 |
|
*Bangladesh national anemia profile (February 2017 revision) (10.0-11.9=Low, 7.0-9.9=Medium, <7.0=High)
Table 2: Clinical characteristics of the participants (N=95).
Table 2 showed, that the mean fibroid was 4.99±2.59 and after having Vitamin D fibroid mean was 3.09±0.68. BMI was 27.96±4.72 and most of them were medium anemia patients were 40(42.1%).
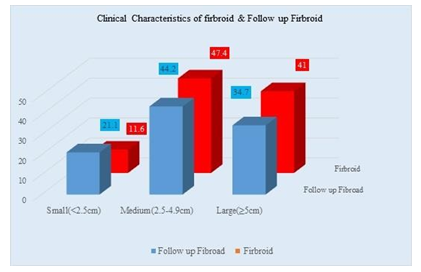
Figure 4: Clinical Characteristics of Fibroid & Follow up Fibroid.
|
Characteristics |
Frequency (n) |
Percentage (%) |
Mean ±SD |
|
Vitamin D Status |
|||
|
Deficiency (<20) |
30 |
31.6 |
21.71±7.32 |
|
Insufficiency (20-24.9) |
29 |
30.5 |
|
|
Sufficiency (≥25) |
36 |
37.9 |
|
Table 3: Vitamin D level is biochemical Characteristics (N=95).
Table 3 showed, that a higher number of patients was Vitamin D Sufficiency was 36(37.9%), and the mean value was 21.71±7.32.
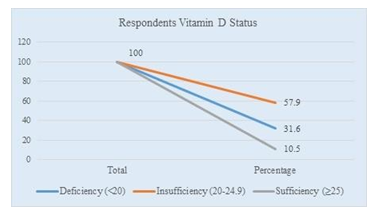
Figure 5: Vitamin D Status of Respondents.
|
Age Group |
Vitamin D |
p- Value |
|||||
|
Deficiency (<20) |
Insufficiency (20- 24.9) |
Sufficiency (≥25) |
|||||
|
n |
% |
n |
% |
n |
% |
0.724ns |
|
|
20 - 30 yrs. |
6 |
20 |
6 |
20.7 |
5 |
13.9 |
|
|
31 -45 yrs. |
19 |
63.3 |
21 |
72.4 |
29 |
80.5 |
|
|
>45 yrs. |
5 |
16.7 |
2 |
6.9 |
2 |
5.6 |
|
Table 4: Age-related vitamin D status (N=95)
Table 4 showed, according to the age group of patients 31-45 years age group had the highest number of patients which was 69(72.0%) in number with vitamin D insufficiency (p<0.724).
|
Age Group |
Vitamin D Level |
p-Value |
|||
|
Frequency |
Mean ±SD |
95% CI |
|||
|
(n) |
Lower Bound |
Upper Bound |
|||
|
20 - 30 yrs. |
17 |
21.62±6.70 |
18.18 |
25.07 |
0.419ns |
|
31 - 45 yrs. |
69 |
22.18±7.43 |
20.39 |
23.96 |
|
|
>45 yrs. |
9 |
18.22±7.42 |
12.52 |
23.93 |
|
Table 5: Mean vitamin D levels by age (N=95)
Table 5 showed, regarding Vitamin D status, the mean value of age groups 20-30 years was 21.62±6.70, 31-45 years was 22.17±7.43 years, and >45 years 18.22±7.42 years respectively. The p-value was 0.419.
|
Characteristics |
Vitamin D Status |
p-Value |
|||||
|
Deficiency (<20) |
Insufficiency (20- 24.9) |
Sufficiency (≥25) |
|||||
|
n |
Mean ±SD |
n |
Mean ±SD |
n |
Mean ±SD |
||
|
Fibroid |
30 |
4.57± 2.55 |
29 |
5.17±2.94 |
36 |
5.20±2.33 |
0.334ns |
|
Follow up Fibroid |
30 |
4.78±2.99 |
29 |
4.57±3.29 |
36 |
4.93±2.96 |
0.831ns |
Table 6: Association of Vitamin D with uterine fibroids (N=95)
In Table 6 it was disseminated that after serving vitamin D fibroid size was significantly changed in the vitamin D insufficient and sufficient group.
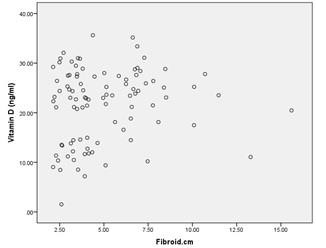
Figure 6: Vitamin D scatterplot before intervention
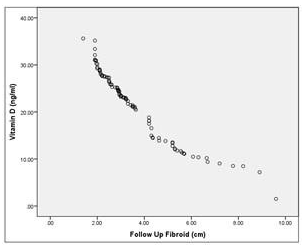
Figure 7: Vitamin D scatterplot after intervention
|
Vitamin D Status |
Fibroids Size |
||||||||
|
Small(<2.5cm) |
Medium (2.5-4.9cm) |
Large (≥5cm) |
|||||||
|
n |
% |
p-Value |
n |
% |
p-Value |
n |
% |
p-Value |
|
|
Deficiency (<20) |
4 |
36.4 |
17 |
37.8 |
9 |
23.1 |
|||
|
Insufficiency (20-24.9) |
3 |
27.2 |
0.996ns |
14 |
31.1 |
0.602ns |
12 |
30.7 |
0.350ns |
|
Sufficiency (≥25) |
4 |
36.4 |
14 |
31.1 |
18 |
46.2 |
|||
Table 7: Fibroid’s size-wise Vitamin D status of the participants (N=95)
|
Vitamin D Status |
Follow up Fibroid Size |
||||||||
|
Small(<2.5cm) |
Medium (2.5-4.9cm) |
Large (≥5cm) |
|||||||
|
n |
% |
p-Value |
n |
% |
p-Value |
n |
% |
p- Value |
|
|
Deficiency (<20) |
6 |
30 |
0.036s |
13 |
31 |
11 |
33.3 |
0.938ns |
|
|
Insufficiency (20-24.9) |
6 |
30 |
15 |
35.7 |
0.883ns |
8 |
24.3 |
||
|
Sufficiency (≥25) |
8 |
40 |
14 |
33.3 |
14 |
42.4 |
|||
Table 8: Follow up Fibroid size in Vitamin D status of the participants after Vitamin D supplementation (N=95)
Following Tables 7 & 8 showed the impact on fibroids considering Vitamin D status, we observed p-Value of the Vitamin D insufficiency group (20-24.9) has significantly changed in the small size of fibroids (>2.5 cm) after Vitamin D supplementations. [p= 0.036].
|
Vitamin D Status |
Fibroids Size |
||||||||
|
Deficiency (<20) |
Insufficiency (20-24.9) |
Sufficiency (≥25) |
|||||||
|
n |
% |
p-Value |
n |
% |
p-Value |
n |
% |
p-Value |
|
|
Small(<2.5cm) |
4 |
13.3 |
3 |
10.3 |
4 |
11.1 |
|||
|
Medium (2.5- 4.9cm) |
17 |
56.7 |
0.043s |
14 |
48.3 |
0.479ns |
14 |
38.9 |
0.273ns |
|
Large (≥5cm) |
9 |
30 |
12 |
41.4 |
18 |
50 |
|||
Table 9: Fibroids Size in Vitamin D status of the participants (N=95)
|
Vitamin D Status |
Follow up Fibroid Size |
||||||||
|
Deficiency (<20) |
Insufficiency (20-24.9) |
Sufficiency (≥25) |
|||||||
|
n |
% |
p-Value |
n |
% |
p-Value |
n |
% |
p-Value |
|
|
Small(<2.5cm) |
6 |
20 |
6 |
20.7 |
8 |
22.2 |
|||
|
Medium (2.5- 4.9cm) |
13 |
43.3 |
0.187ns |
15 |
51.7 |
0.227ns |
14 |
38.9 |
0.493ns |
|
Large (≥ 5cm) |
11 |
36.7 |
8 |
27.6 |
14 |
38.9 |
|||
Table 10: Follow up Fibroid Size in Vitamin D status of the participants (N=95)
Following Table 9 & 10 impacts on fibroids considering fibroids size after Vitamin D supplementations, p-Value significantly changed in the Vitamin D insufficiency group (20-24.9) [p=0.227].
|
Characteristics |
Vitamin D |
|
|
r |
p-Value |
|
|
Fibroids |
0.125 |
0.228 |
|
Follow up Fibroid |
0.023 |
0.825 |
Table 11: Correlation of clinical & biochemical variables among participants
Discussion
Uterine fibroids are the most prevalent benign tumor in women of reproductive age (5.4% to 77%). They develop in premenopausal women's uterine muscle.1, 2 During the course of a woman's reproductive life, it is likely to develop one or more uterine fibroids.3 Leiomyoma risk factors include obesity, family history of fibroids and null parity.4, 5 They can induce abnormal bleeding, pelvic pressure, infertility, and growth/regression. Leiomyoma causes hysterectomy in millions of women.6 Depending on the patient's age, purpose for treatment, reproductive concerns, and personal preference, treatment includes pharmacological therapy, surgery, and uterine artery embolization or ablative procedures.7-9 As a result, it seems that the adverse effects of less harmful therapies and interventions should be considered. Some research focused on the impact of diet on the prevalence of leiomyoma.10-13 Vitamin D affects myometrial and fibroid cell growth in vitro, according to Blauer et al.2009. Normal myometrial and fibroid cell development were reduced by physiologic vitamin D.14 Halder et al. discovered that therapy with 1.25- dihydroxy vitamin D3 dramatically decreased uterine fibroid tumor sizes, extending this vitamin D theory.15 Leiomyomas tend to overexpress cyclin D1, whose action is needed for the cell cycle to move from the G1 phase to the S phase, and proto-oncogene MYC, which makes cells multiply and has been linked to many types of cancers. Uterine leiomyomas treated with vitamin D were found to have significantly lower levels of cyclin D1 and MYC than those in the control group. The Eker rat research suggests that vitamin D's antiproliferative and pro-apoptotic pathways may decrease uterine fibroids. After menopause, estrogen and progesterone cause uterine leiomyomas to diminish. The "Eker rat model" revealed that vitamin D-treated fibroids reduced the expression of Estrogen Receptor 1 (ESR1), Progesterone Receptor A (PGR-A), and Progesterone Receptor B. (PGR-B). This method of reducing uterine fibroids with vitamin D may be effective. According to research Catechol-O-methyltransferase, an enzyme in the biological estrogen pathway, is elevated in uterine fibroids.16 Vitamin D inhibited the proliferation of human uterine leiomyoma cells by 47+/-.03 percent at 1 M and by 38+/-.02 % at.01M compared to controls, and it did so through reduce catechol- O-methyl transferase. Similar to earlier research, the injection of vitamin D lowered the expression of kinases, BCL-2, BCL-w, CDK1, and PCAN. By noticing a drop in catechol-O- methyl transferase, this study shows that the estrogen pathway may be how vitamin D limits fibroid development.17, 18 According to this study at the initial stage, among total patient’s 11.6% (n=11) patients were found small size of UFs (<2.5 cm), 47.4% (n=45) were medium (2.5-4.9 cm) and 41.0% (n=39) were found large in size of UFs (≥5 cm) respectively.
The mean size of fibroids in a total of 95 patients was 4.99±2.59 and Supplementation with vitamin D had lowered it to 4.77±3.04. These findings are similar to many other studies conducted around the world. Ethnic groups with lower serum Vitamin D levels were shown to have higher UFs, according to a study. Vitamin D insufficiency may play a role in the development of UFs.19 In this study, it has been found that maximum patients 55(57.9%) had vitamin D insufficiency [25(OH)D level (20-29.9) ng/ml] and 30(31.6%) had deficiency [25(OH)D level (<20) ng/ml]. Whereas, only 10(10.5%) had sufficient level [25(OH)D level (>30) ng/ml] of vitamin D. In many studies vitamin D deficiencies were found as a key reason of fibroids in women, especially in the third world. In searching the evidence of vitamin D levels, it has been found some noticeable records of vitamin D deficiencies in fibroids women. In a study, 25-hydroxyvitamin D3 levels were lower in fibroids than in controls.19 62.5 % of women with fibroids and 26.39 % of controls had vitamin D3 insufficiency (10 ng/dl). 20 Only 2.7% of fibroids patients had adequate vitamin D3 levels (30 ng/dl), compared to 23.6% of controls. 20 The odds ratio (OR) of fibroid with blood vitamin D3 level of 10 ng/dl was 4.64 (95% CI: 2.28-9.44) (p = 0.0001).20 In this study it has been found, that vitamin D deficiency (<20), insufficiency (20-29.9), and sufficiency (>30) in 31.6%,57.9%, and 10.5% participants respectively. So according to the findings of this study and the data from some similar recent research, women in Bangladesh may be at risk for fibroid growth due to vitamin D deficiency and insufficiency.
Conclusion
Supplementation with Vitamin D in women with fibroid uterus may regress the fibroid size and it is more effective significantly in smaller fibroid sizes (p=0.036). In this study, the smaller size of uterine fibroid was reduced after supplementation of Vitamin D among the participants. It was significant (p<0.05) of fibroid uterus size changed after Vitamin D was supplemented. Uterine fibroids could benefit from vitamin D supplementation that is both safe and inexpensive, but further research is needed to confirm this.
References
- Lippman SA, Warner M, Samuels S, et Uterine fibroids and gynecologic pain symptoms in a population-based study. Fertil Steril 2003; 80: 1488-94.
- Flake GP, Andersen J, Dixon D. Etiology and pathogenesis of uterine leiomyomas: a review. Environ Health Perspect 2003; 111: 1037-54.
- Baird DD, Dunson DB, Hill MC, Cousins D, Schectman JM. High cumulative incidence of uterine leiomyoma in black and white women: ultrasound American journal of obstetrics and gynecology. 2003;188(1):100- 107. PMID: 12548202.
- Kjerulff K, Langenberg P, Seidman J, Stolley P, Guzinski Uterine leiomyomas: racial differences in severity, symptoms and age at diagnosis. J Reprod Med 1996; 41: 483-90.
- Bouyer J, Job-Spira N, Pouly J, et al. Fertility following radical, conservative-surgical or medical treatment for tubal pregnancy: a population-based 2000; 107: 714-21.
- Pérez-López FR, Ornat L, Ceausu I, et EMAS position statement: management of uterine fibroids. Maturitas 2014; 79; 106-16.
- Parker Etiology, symptomatology and diagnosis of uterine myomas. Fertil Steril 2007; 87: 725-36.
- Olive DL, Lindheim SR, Pritts Non- surgical management of leiomyoma: impact on fertility. Curr Opin Obstet Gynecol 2004; 16: 239-43.
- Walker CL, Stewart EA. Uterine fibroids: the elephant in the room. Science 2005; 308: 1589-
- Wise LA, Radin RG, Palmer JR, et al. Intake of fruit, vegetables, and carotenoids in relation to risk of uterine leiomyomata. Am J Clin Nutr 2011; 94: 1620-31.
- Wise LA, Palmer JR, Ruiz-Narvaez, Reich DE, Rosenberg Is the observed association between dairy intake and fibroids in African Americans explained by genetic ancestry Am J Epidemiol 2013; 178: 1114-9.
- Wise LA, Radin RG, Kumanyika SK, et Prospective study of dietary fat and risk of uterine leiomyomata. Am J Clin Nutr 2014; 99: 1105-16.
- Shen Y, Xu Q, Xu J, Ren ML, Cai Environmental exposure and risk of uterine leiomyoma: an epidemiologic survey. Eur Rev Med Pharmacol Sci 2013; 17: 3249-56.
- Bläuer M, Rovio PH, Ylikomi T, Heinonen PK (2009) Vitamin D inhibits myometrial and leiomyoma cell proliferation in Fertil Steril 91: 1919-1925.
- Halder SK, Sharan C, Al-Hendy A (2012) 1,25-dihydroxyvitamin D3 treatment shrinks uterine leiomyoma tumors in the Eker rat Biol Reprod 86: 116.
- Salama SA, Shu-Leong Ho, Hui-Qun W, Tenhunen J, Tilgmann C, et (2006) Hormonal regulation of Catechol-O-methyl transferase activity in women with uterine leiomyomas. Fertil and Steril 86: 259-262.
- Sharan C, Halder SK, Thota C, Jaleel T, Nair S, et al. (2011) Vitamin D inhibits proliferation of human uterine leiomyoma cells via catachol- O-methyltransferase. Fertil Steril 95: 247-253.
- Artaza JN, Norris KC (2009) Vitamin D reduces the expression of collagen and key profibrotic factors by inducing an antifribrotic phenotype in mesenchymal multipotent cells. J Endocrinol 200: 207-221.
- Sabry M, Halder SK, Allah AS, Roshdy E, Rajaratnam V, Al-Hendy A. Serum vitamin D3 level inversely correlates with uterine fibroid volume in different ethnic groups: a cross- sectional observational Int J Womens Health. 2013;5:93-100.
- Singh V, Barik A, Imam N. Vitamin D3 Level in Women with Uterine Fibroid: An Observational Study in Eastern Indian J Obstet Gynaecol India. 2019;69(2):161-165. doi:10.1007/s13224-018- 1195-4.
