Sports Femoral Hernia in a Young Female Weightlifter - The First Reported Case in the World
Article Information
Shariful Islam1,2*, Vinoo Bheem1, Patrick Harnarayan1,2, Yardesh Singh1,2, Vijay Naraynsingh2
1San Fernando Teaching Hospital, Trinidad and Tobago
2Department of Clinical Surgical Science, University of the West Indies, St. Augustine, Trinidad and Tobago
*Corresponding Author: Dr. Shariful Islam, Department of Clinical Surgical science, University of the West Indies, St Augustine, Trinidad and Tobago
Received: 04 Sep 2019; Accepted: 30 September 2019; Published: 28 November 2019
Citation: Shariful Islam, Vinoo Bheem, Patrick Harnarayan, Yardesh Singh, Vijay Naraynsingh. Sports Femoral Hernia in a Young Female Weightlifter - The First Reported Case in the World. Archives of Clinical and Medical Case Reports 3 (2019): 675-682.
View / Download Pdf Share at FacebookAbstract
A sports hernia is an increasingly recognized cause of chronic groin pain among many professional and non-professional athlete. It is a misnomer as there is no classic herniation of soft tissue. However, small occult inguinal hernias are documented during surgical exploration. It is more commonly seen in young male than female athletes. Diagnosis is usually challenging as most this pain has an insidious onset. It requires a high index of suspicious as clinically visible sports hernia has not yet been reported in the English literature. Similarly, a visible incarcerated femoral hernia in a young weightlifter has yet to be reported. We report the case of 27 years young professional female weightlifter who presented with having an aching pain in her left groin for one year. She had visited many GP’s and her pain temporary subsided with the use of NSAIDs. A Computerized Tomography of abdomen and pelvis revealed a left femoral hernia. Emergency femoral hernia repair was performed. The patient’s had an uneventful post-op recovery. At 36 months follow up the patient is doing well, participating in her professional weightlifting without any further complaints. This case highlights the typical presentation of the sports hernia i.e chronic groin pain and also illustrates how the diagnosis of this hernia is missed or delayed. We hereby report the world first case of incarcerated visible femoral hernia in a young professional weightlifter and a literature search was performed to highlight its management options.
Sports hernia articles, Sports femoral hernia articles, Young female patient articles, Young athletes articles
Femoral Hernia articles Femoral Hernia Research articles Femoral Hernia review articles Femoral Hernia PubMed articles Femoral Hernia PubMed Central articles Femoral Hernia 2023 articles Femoral Hernia 2024 articles Femoral Hernia Scopus articles Femoral Hernia impact factor journals Femoral Hernia Scopus journals Femoral Hernia PubMed journals Femoral Hernia medical journals Femoral Hernia free journals Femoral Hernia best journals Femoral Hernia top journals Femoral Hernia free medical journals Femoral Hernia famous journals Femoral Hernia Google Scholar indexed journals physiotherapist articles physiotherapist Research articles physiotherapist review articles physiotherapist PubMed articles physiotherapist PubMed Central articles physiotherapist 2023 articles physiotherapist 2024 articles physiotherapist Scopus articles physiotherapist impact factor journals physiotherapist Scopus journals physiotherapist PubMed journals physiotherapist medical journals physiotherapist free journals physiotherapist best journals physiotherapist top journals physiotherapist free medical journals physiotherapist famous journals physiotherapist Google Scholar indexed journals GP articles GP Research articles GP review articles GP PubMed articles GP PubMed Central articles GP 2023 articles GP 2024 articles GP Scopus articles GP impact factor journals GP Scopus journals GP PubMed journals GP medical journals GP free journals GP best journals GP top journals GP free medical journals GP famous journals GP Google Scholar indexed journals tachycardic articles tachycardic Research articles tachycardic review articles tachycardic PubMed articles tachycardic PubMed Central articles tachycardic 2023 articles tachycardic 2024 articles tachycardic Scopus articles tachycardic impact factor journals tachycardic Scopus journals tachycardic PubMed journals tachycardic medical journals tachycardic free journals tachycardic best journals tachycardic top journals tachycardic free medical journals tachycardic famous journals tachycardic Google Scholar indexed journals leukoencephalopathy articles leukoencephalopathy Research articles leukoencephalopathy review articles leukoencephalopathy PubMed articles leukoencephalopathy PubMed Central articles leukoencephalopathy 2023 articles leukoencephalopathy 2024 articles leukoencephalopathy Scopus articles leukoencephalopathy impact factor journals leukoencephalopathy Scopus journals leukoencephalopathy PubMed journals leukoencephalopathy medical journals leukoencephalopathy free journals leukoencephalopathy best journals leukoencephalopathy top journals leukoencephalopathy free medical journals leukoencephalopathy famous journals leukoencephalopathy Google Scholar indexed journals treatment articles treatment Research articles treatment review articles treatment PubMed articles treatment PubMed Central articles treatment 2023 articles treatment 2024 articles treatment Scopus articles treatment impact factor journals treatment Scopus journals treatment PubMed journals treatment medical journals treatment free journals treatment best journals treatment top journals treatment free medical journals treatment famous journals treatment Google Scholar indexed journals Neurology articles Neurology Research articles Neurology review articles Neurology PubMed articles Neurology PubMed Central articles Neurology 2023 articles Neurology 2024 articles Neurology Scopus articles Neurology impact factor journals Neurology Scopus journals Neurology PubMed journals Neurology medical journals Neurology free journals Neurology best journals Neurology top journals Neurology free medical journals Neurology famous journals Neurology Google Scholar indexed journals lymphadenopathy articles lymphadenopathy Research articles lymphadenopathy review articles lymphadenopathy PubMed articles lymphadenopathy PubMed Central articles lymphadenopathy 2023 articles lymphadenopathy 2024 articles lymphadenopathy Scopus articles lymphadenopathy impact factor journals lymphadenopathy Scopus journals lymphadenopathy PubMed journals lymphadenopathy medical journals lymphadenopathy free journals lymphadenopathy best journals lymphadenopathy top journals lymphadenopathy free medical journals lymphadenopathy famous journals lymphadenopathy Google Scholar indexed journals Mechanical atherothrombectomy articles Mechanical atherothrombectomy Research articles Mechanical atherothrombectomy review articles Mechanical atherothrombectomy PubMed articles Mechanical atherothrombectomy PubMed Central articles Mechanical atherothrombectomy 2023 articles Mechanical atherothrombectomy 2024 articles Mechanical atherothrombectomy Scopus articles Mechanical atherothrombectomy impact factor journals Mechanical atherothrombectomy Scopus journals Mechanical atherothrombectomy PubMed journals Mechanical atherothrombectomy medical journals Mechanical atherothrombectomy free journals Mechanical atherothrombectomy best journals Mechanical atherothrombectomy top journals Mechanical atherothrombectomy free medical journals Mechanical atherothrombectomy famous journals Mechanical atherothrombectomy Google Scholar indexed journals patient articles patient Research articles patient review articles patient PubMed articles patient PubMed Central articles patient 2023 articles patient 2024 articles patient Scopus articles patient impact factor journals patient Scopus journals patient PubMed journals patient medical journals patient free journals patient best journals patient top journals patient free medical journals patient famous journals patient Google Scholar indexed journals
Article Details
1. Introduction
The term “sports hernia” is a misnomer as there is typically no true hernia or defect in the groin or abdominal wall [1]. However, it is now widely used by the media, as well as by the medical profession. A variety of other terms have been used to describe this condition including ‘sportsman’s hernia’, ‘hockey groin’, ‘athletic pubalgia, and Gilmore's groin. Sports hernias were first described in the early 1980s, and usually present with a whole range of problems affecting their hips, impingement of the ilioinguinal nerve or one of its branches, or a weakness in the abdominal wall muscle but there is no visible hernia. However; small asymptomatic occult inguinal hernias are documented during surgical exploration. It is commonly seen in the elite athletes and is more common in males than females. Females account only 3-15% of all sports hernia referrals [2, 3]. The diagnosis is difficult and often not recognized for several months or even years. Many of these patients will have made several visits to their GP and or physiotherapist and treated as a chronic ‘groin strain’. Early detection and prompt treatment are of paramount importance in the management of these hernias. However, it requires a high index of suspicion and a multi-disciplinary team approach consisting of GPs, surgeons, physiotherapists, and radiologists.
2. Case Presentation
A 27 years old female, professional national weightlifter presented to the Emergency Department with progressively worsening pain in her left groin for the last few weeks. History revealed that the patient had aching pain for the last one year. She claimed that she only feels the pain after the heavyweight lift but denied off any pain with regular weightlifting. The patient visited many GP's and her pain temporary subsided with the use of NSAIDs. The patient had one child and was born by normal vaginal delivery. She had no co-morbid condition and denied any trauma or surgery in the past. Over the last few weeks, the pain worsened and the patient went to a general surgeon. A CT of abdomen and pelvis with intravenous contrast was performed which revealed a left femoral hernia with a partial small bowel obstruction (Figure 1). The patient was then referred to the general hospital for further management.
On examination, the patient was mildly tachycardic with a pulse of 110 beats per minute and her mucous membranes were pink but mildly dehydrated. Her abdomen was minimally distended, tympanic with no guarding or rebound tenderness. There was just a barely visible, tender swelling over the left femoral canal (Figure 2). The overlying skin was normal and there was no inguinal lymphadenopathy. The digital rectal examination and per vaginal examination was normal.

Figure 1: CT scan of abdomen and pelvis with intravenous contrast showing obvious left femoral hernia.

Figure 2: Photograph of the groin- the arrow indicating the position of the left femoral hernia.
After resuscitation, the patient was taken to the OR for emergency exploration of the groin. Under GA and the patient in the supine position entire abdomen and groin was cleaned and draped. A right oblique inguinal incision was made and a 4x4 cm sac of left femoral hernia was noted (Figure 3). A trans-inguinal approach was used for the surgery. The content of the sac was a loop was small bowel and it was noted to be viable (Figure 4). The sac was closed and the hernia was reduced. A Mc Vay Cooper's repair was done with non- absorbable sutures along with on-lay mesh hernioplasty. The patient had an uneventful recovery. At 36 months follow up the patient is doing well, participating in her professional weightlifting without any further complaints.
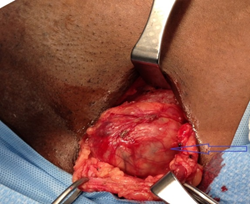
Figure 3: Intraop photograph showing left femoral hernia sac.
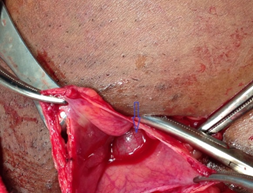
Figure 4: Intraop photograph showing small bowel as the content of the femoral hernia sac.
3. Discussion
The sports hernia is defined as any condition causing persistent groin pain without any demonstrable hernia. It most often occurs during sports that require sudden changes of direction or intense twisting movements. Although a sports hernia may lead to a traditional, abdominal hernia, it is a different injury. Although clinically there is no inguinal hernia, a small number of occult hernias are reported in different series and these often identified at the time of surgery. Over the last decades, this condition has become more commonly described as several well-known professional athletes have undergone surgical treatment of this condition.
Sports hernia was first described in Europe but has now become a common diagnosis in the professional athletes in the USA. Sports hernias typically affect young males who actively participate in sport. Females account only 3-15% of all sports hernia referrals [2, 3]. It is rare in children and older people. However, sports hernia is not confined to professional athletes alone. It has also been described in youths, school, college and recreational athletes. It is more common in patients that participate in football, hockey, and athletics [4].
The prevalence of hip and groin abnormalities amongst the professional US male soccer players is 54.7% [5]. Approximately 37.5% of the US Men's National Soccer Team players had surgery for sports hernia, and 12.5% of them have had bilateral sports hernia surgery. In 66% of these cases, they had a dual diagnosis [6]. The etiology and pathophysiology of sports hernia are varied in the literature. It involves a set of complex injuries to the abdominal and pelvic musculature leading to weakness of the posterior wall of the inguinal canal [2]. A study in 2007; suggests that any heavy work even with is a single strenuous attempt can predispose to sudden inguinal herniation [7]. Weightlifting is also a known cause of increased intra-abdominal pressure besides many other causes. The increased the intra-abdominal pressure after any strenuous activity can force against the inguinal canal or any other weak point of the abdomen and can increase the chance of herniation [8].
Hip and groin issues very rarely occur as a result of an acute injury. This is typically a gradual process and had a complex relationship between these problems. When athletes develop one of these problems, they begin to lose range of motion in their hips leading to complex series of events which further restrict the range of motion as they continue to play, causing a labral tear, more weakness in the anterior abdominal wall, and secondary adductor pain.
The real problem in sports hernia patient is not an abdominal wall muscle strength issue; rather the abdominal wall in a particular region is too thin, allowing the hernia to form [7, 8].
The femoral canal is a region in the lower abdomen, just below the groin. The canal is located in the femoral triangle. It the most medial compartment of this triangle. The opening of this canal is known as the femoral ring, usually covered by areolar tissue. The femoral ring is bounded superiorly by the inguinal ligament, inferiorly by the pectineal ligament, medially by the pubic tubercle and laterally by the femoral vein. This area of the abdomen is prone to weakening of the abdominal wall, allowing an out-pouching, or a hernia, to form especially in the elderly multiparous female.
The symptom of sports hernia includes pain in the groin or lower abdomen or in the testicle (in males). It typically begins with the gradual onset of aching pain in the lower abdomen or in the groin. However, these symptoms are usually exacerbated by various types of physical activities such as forward bending, jogging and running and even with sneezing or coughing. It is commonly seen in athletes who have to maintain a forward bending position i.e hockey players. Groin pain is one of the most common presentations in these types of patients. Some of the possible sources of groin pain are adductor muscle strains, hip labral tears, osteitis pubis and stress fractures in the pelvis. Sports hernia is a relatively uncommon cause of groin pain. In soccer players, kicking the ball may cause a sharp pain. This pain may radiate. Thirty percent of males experience testicular pain, and 40% have tenderness in the adductor region [2]. The pain may become chronic and bilateral over time [6, 7].
Diagnosis of sports hernia can often be challenging. It's hard for a single clinician to make a correct diagnosis; therefore a multi-specialty team approach is strongly advocated for these patients. The diagnosis of a sports hernia should be entertained based on the patient's clinical history, physical examination, and diagnostic tests. Research has suggested that the incidence of these injuries by more than 25% in soccer [6].
History and physical examination need to be thorough and systematic. Speak to the trainers and others who may have worked with the athlete to get their perspectives as well. After the range-of-motion maneuver and dynamic testing; x-rays of the pelvis, hips and lower back can give an initial idea. Studies have reported that routine x- rays were able to pick up 68% cam deformities in male and 50% in the female which was silent on the US Men's National Soccer team and two Major League Soccer teams. Most players didn't even know it [5]. The main two imaging modalities used to assist in the diagnosis of sports hernia are MRI and ultrasound. MRIs are now being commonly used to diagnose the sports hernia. It has become the gold standard test for the diagnosis of the sports hernia. MRI with gadolinium can better illuminate the labral tears, any loose bodies, and other characteristics of femoro-acetabular impingement. In some cases like ours; the CT scan of abdomen and pelvis can also help in the diagnosis. When contemplating the management options of sports hernia, a brief period (6–12 weeks) of non-surgical treatment should be initially attempted [9]. When the patient is pain-free following this they should attempt to return to sport; if this is unsuccessful, operative intervention should be considered. Non-operative management consists of a combination of: rest; non-steroidal anti-inflammatory drugs (NSAIDs); corticosteroid injections; and physiotherapy. Physical therapy should be instituted focusing on core stabilization, postural retraining, and normalization of the dynamic relationship of the hip and pelvic muscles [10].
There are very little data regarding the effectiveness of non-surgical treatment for athletic pubalgia / sports hernia. A prospective, randomized study of athletes with chronic groin pain/sports hernia compared physical therapy with surgical repair (laparoscopic mesh repair) for sports hernias. Seven of 30 patients in the nonsurgical arm switched to the surgical arm secondary to continued symptoms, and only 50% returned to sport at 1-year follow-up 24. In the surgical arm, 29 of 30 athletes returned to full sports and were pain free at 1-year follow-up [11]. It causes a chronic, activity-related groin pain that rarely responds to non-operative treatment but significantly improves with operative intervention [7].
Surgical Treatment and Outcomes- Various surgical techniques have been described for sports hernia with > 80% return rates to sporting activities. These are basically modifications of the classic Shouldice, Bassini, or Lichtenstein hernia repair techniques. The main aim of these is to reinforce the abdominal muscles or fascia near the inguinal ligament.6 These include repair of the external oblique, transversus abdominus, transversalis fascia; repairs with mesh reinforcement; laparoscopic repairs; mini-open repairs; and broad pelvic floor repairs with or without adductor releases and neurectomies [11, 12]. Laparoscopic repair (the preferred approach) involves reinforcement of the posterior abdominal wall with mesh; this may be either total extraperitoneal (TEP) or trains abdominal pre-peritoneal (TAP) [11-14].
4. Preventative Measures
There are some simple preventative measures that one can take to help prevent getting a hernia.
- Start each workout with a good warm up. Lift light weights before taking part in competitive sports or attempting any heavy lifting. A regular weight lifting routine can actually help prevent hernias from occurring in the first place. Weightlifters and bodybuilders have a stronger abdominal wall lining compared to sedentary individuals, and thus are less likely to tear that lining when lifting.
- Progress slowly and do so in small increments rather than trying to make too big of a jump and lifting too much too soon.
- Don’t do forced Reps rather take a rest break, and then perform an additional set. Doing another set is better than forced reps because the total volume of work performed by your muscles is actually more, and your risk of injury is greatly reduced.
- Breathe into your belly – The best way to breathe when lifting weights is abdominal breathing. This style of breathing is not only safer, but it will make you feel stronger as well because it helps to stabilize your torso when lifting.
- Always maintain a healthy body weight as overweight is a big risk factor for hernias.
- Avoid Smoking.
- Move your bowels- Eat food rich in fibers i.e- whole grains, fruits and vegetables and drink plenty water (about 1 gallon per day for bodybuilders and athletes).
5. Weightlifting after Surgery
According to the Hernia Center of Southern California, weightlifters can gradually begin lifting small amounts of weights within the first week of surgery. They can resume regular training after eight weeks.
6. Conclusion
Sports hernia is an increasingly recognized cause of chronic groin pain among many professional and non-professional athletes. Diagnosis is usually challenging. It requires a high index of suspicion. Early detection and prompt treatment are of paramount importance in the management of these hernias. Any delayed or miss diagnosis can have a significant impact on their athletic career from time lost to significant disability. A careful history, through physical examination, and imaging are required for an accurate diagnosis. A brief period of conservative treatment should be started while waiting for the diagnosis. Surgery should be performed as early as possible once the diagnosis of a sports hernia is confirmed. A multi-disciplinary team approach should be taken for the management of these sports hernia patients. After successful rehabilitation, the athlete can resume back to his regular sporting activities.
7. Learning Points
- Sports hernias are a real entity that should form part of the differential diagnosis of athletic patients presenting with groin pain.
- Patients should be referred to a general surgeon with a particular interest in sports hernias.
- In cases of diagnostic uncertainty, it would also be appropriate to make a referral to a specialist.
- Persistent symptoms despite non-operative therapy; surgical intervention would be suitable.
- Early detection and instigation of the correct treatment are essential in the management of sports hernia.
- The diagnosis and appropriate treatment require a high index of suspicion and a multi-professional approach, consisting of GPs, surgeons, physiotherapists, and radiologists.
Conflicts of Interest
The authors declare no conflicts of interest.
Author contribution
All authors have contributed significantly to designing and organizing to write the manuscript, collecting data as well help in critically analyzing the manuscript. All authors have approved the final version of this manuscript.
Funding
No fund was received to publish this article.
Consent
Patient consent was obtained.
Guarantor
The corresponding author will accept the full responsibility for the work.
References
- Minnich JM, Hanks JB, Muschaweck U, et al. Sports hernia: diagnosis and treatment highlighting a minimal repair surgical technique. Am J Sports Med 39 (2011):1341-1349.
- Meyers WC, McKechnie A, Philippon MJ, et al. Experience with ‘sports hernia’ spanning two decades. Ann Surg 248 (2008): 656-665.
- Garvey JFW, Read JW, Turner A. Sportsman hernia: what can we do? Hernia 14 (2010): 17-25.
- Meyers WC, Foley DP, Garrett WE, et al. Management of severe lower abdominal or inguinal pain in high-performance athletes. PAIN (Performing Athletes with Abdominal or Inguinal Neuromuscular Pain Study Group). Am J Sports Med 28 (2000): 2-8.
- Gerhardt MB, Romero AA, Silvers HJ, et al. The prevalence of radiographic hip abnormalities in elite soccer players. Am J Sports Med 40 (2012): 584-548.
- Mandelbaum B, Silvers HJ, et al. American Academy of Orthopaedic Surgeons. Femoro-Acetabular Impingement (2017).
- Harmon KG. Evaluation of groin pain in athletes. Curr Sports Med Reports 6 (2007): 354-361.
- Sriram Ramgopal, et al. Does Lifting Weights Affect an Inguinal Hernia? (2017).
- Caudill P, Nyland J, Smith C, et al. Sports hernias: a systematic literature review. Br J Sports Med 42 (2008): 954-964.
- Muschaweck U, Berger L. Minimal repair technique of sportsmen’s groin: an innovative open suture repair technique to treat chronic inguinal pain. Hernia 14 (2010): 27-33.
- Paajanen H, Brinck T, Hermunen H, Aero I. Laparoscopic surgery for chronic groin pain in athletes is more effective than nonoperative treatment: a randomized clinical trial with magnetic resonance imaging of 60 patients with sportsman’s hernia (athletic pubalgia). Surgery 150 (2011): 99-107.
- Christopher M. Larson, Sports Hernia/Athletic Pubalgia. Evaluation and Management. Sports Health 6 (2014): 139-144.
- Gilmore’s groin. Sports med Soft Tissue Trauma 3 (1992): 12-14.
- Ziprin P, Prabhudesai SG, Abrahams S, et al. Trans-abdominal pre-peritoneal laparoscopic approach for the treatment of sportsman’s hernia. J Laparoendosc Adv Surg Tech A 18 (2008): 669-672.
