Spontaneous Subcapsular Liver Hematoma Complicating Heparin Overdose: An Unusual Complication
Article Information
Rida Touab, M.D1*, Ayoub Bouayda, M.D1, Mohammed Rabii Andaloussi, M.D1, Chakib Chouikh, Ph.D1, Khalil Mounir, Ph.D1, Abdelhamid Eljaafari Ph.D1, Hicham Balkhi, Ph.D1
1Department of anesthesiology and critical care, Military Training Hospital Mohamed V, Rabat, Morocco
*Corresponding author: Rida Touab, Depatment of anesthesiology and critical care, military traning hospital Mohamed V, Rabat, Morocco.
Received: 31 May 2024; Accepted: 10 June 2024; Published: 20 June 2024
Citation: Rida Touab, M.D, Ayoub Bouayda, M.D, Mohammed Rabii Andaloussi, M.D, Chakib Chouikh, Ph.D, Khalil Mounir, Ph.D, Abdelhamid Eljaafari Ph.D, Hicham Balkhi, Ph.D. Spontaneous Subcapsular Liver Hematoma Complicating Heparin Overdose: An Unusual Complication. Archives of Internal Medicine Research. 7 (2024): 134-135.
View / Download Pdf Share at FacebookAbstract
Introduction:
Spontaneous subcapsular liver haematoma have a significant morbidity.
Case report:
Women 56 years old, was admitted for the management of severe community-acquired pneumonia. Evolution had marqued by phlebitis treated with heparin complicating by an overdose and a subcapsular liver hematoma.
Conclusion:
Through this case we describe a liver hematoma that an exceptional complication of heparin therapy.
Keywords
Subcapsular hematoma; Phlebitis; Heparin; Overdose; Antagonism
Article Details
Introduction:
Spontaneous Subcapsular liver haematoma is a rare disease with significant morbidity [1], defined as any non-traumatic liver bleeding with subcapsular localization [2], described mainly during pregnancy complicating a HELLP syndrome with or without preeclampsia, but may be secondary to tumor pathology [2], all coagulation abnormalities, amyloidosis [3], hepatic peliosis [4] and certain connective tissue diseases [5].
Through this observation, we describe a rare localization of a bleeding event complicating heparin therapy.
Case report:
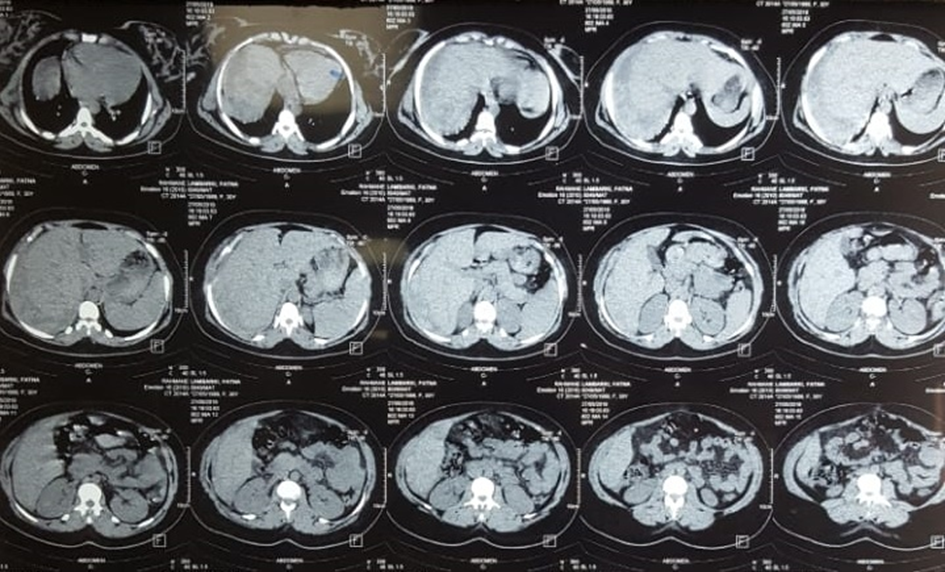
A women 56 years old, had a history of type II diabetes treated with metformin, hypertension treated with an angiotensin II receptor blocker, complicated by chronic kidney disease. She was admitted to the intensive care unit for the management of acute respiratory failure with severe community-acquired pneumonia. Physical examination had objectified a conscious patient, tachypneic at 33 cycles per minute, 88% saturation to room air, with rales crackling in focus on the right, her heart rhythm at 110 beats per minute, with blood pressure at 137/87 mmHg on admission, with no evidence of deep vein thrombosis, and abdominal and neurological examination were normal. Hourly dieresis was normal and the patient had a blood glucose imbalance with a capillary blood glucose level of 2.7 g/L. Initial management consisted of ventilatory support and oxygenation by means of intermittent non-invasive ventilation for 30 minutes every 4 hours, relayed by a reservoir mask allowing a pulsed oxygen saturation of 94%, third generation cephalosporin combined with a fluoroquinolone as an empiric therapy, with prevention of complications during her stay in intensive care unit. The paraclinical assessment was based on thoracic radiography with an appearance of pneumonia, gasometry showing hypoxemia with PaO2 at 55 mmHg in air and PaCO2 at 33, hyperleukocytosis at 15,300/mm3, an inflammatory syndrome with a reactive protein C at 235 mg/l, and renal failure with uremia at 1.8 g/l and a creatinine level at 33 mg/l. The evolution was marked by the development of arterial hypotension, hencing introduction of norepinephrine as a continuous intravenous infusion via a femoral venous catheter to maintain a mean arterial pressure above 80 mmHg with radial arterial catheterization for invasive blood pressure monitoring. At day three of admission, after hemodynamic stabilization, signs of phlebitis appeared, and was confirmed by venous doppler objectiving an ipsilateral femoral thrombosis to the catheter, leading to the initiation of anticoalulation with unfractionated heparin in continuous infusion and withdrawal of the catheter from the femoral route. The infusion rate was adjusted according to APTT with difficulty in finding a target dose. Two days after anticoagulation initiation, patient presented right hypochondrial pain, with tenderness on physical examination, explored by ultrasound, objectifying a liver’s hematoma supplemented by a CT scan confirming the diagnosis of a sub-capsular hematoma on a healthy liver (Figure 1), with an APTT that was 4 x the control and a mild cholestasis. The conduct was to stop the heparin, antagonize the dose for the last four hours with protamine sulfate, and monitor hemodynamic status and hemoglobin levels. Thrombosis was treated by mechanical means in the lower limb with discussion in order to place a filter cava. Ultrasound monitoring of the haematoma, performed every 48 hours or when symptoms occurred, showed that these dimensions had stabilized and then progressively resorbed. Anticoagulation was introduced five days later with unfractionated heparin with armed monitoring.
Discussion:
Liver Spontaneous hemorrhage is a rare condition whose etiology is largely dominated, outside the peripartum, by tumor lesions first: hepatocellular adenomas and carcinomas[6,7]. In our case it could be related to an overdose of heparin, constituting an acquired hemostasis disorder. Cases complicating vesicular surgery have been reported, with surgical trauma and non-steroidal anti-inflammatory drugs as common risk factors [8]. The discovery may be fortuitous, or on the occasion of clinical signs ranging from pain - in our patient's case - to hemodynamic instability secondary to rupture of the hematoma, a dreadful complication requiring urgent action: surgical hemostasis or embolization [2].
In our patient, there were therapeutic dilemmas between the risk of hemorrhage from sub scapular hematoma and the thrombotic risk from deep venous thrombosis, and the difficult question of the ideal timing to safely resume anticoagulation, with choices between a pure expectant attitude or radio-guided evacuation8 or surgical evacuation in an emergency situation. The answer was one: attitude that showing by profit-risk balances.
Conclusion:
We have reported one case of intrahepatic hemorrhage as a bleeding event from heparin treatment of deep vein thrombosis: a rare complication of anticoagulation.
References
- Boulouis et al. Diagnostic and Interventional Imaging. http://dx.doi.org/10.1016/j.diii.2012.09.004.
- Davidson B, Carratta R, Paccione F, et al. Surgical emergencies in liver disease. Baillieres Clin Gastroenterol 5 (1991):737-758.
- Ades CJ, Strutton GM, Walker NI, et al. Spontaneous rupture of the liver associated with amyloidosis. J Clin Gastroenterol 11 (1989): 85-87.
- Choi SK, Jin JS, Cho SG, et al. Spontaneous liver rupture in a patient with peliosis hepatis: a case report. World J Gastroenterol 15 (2009): 5493-5497.
- Haslock I. Spontaneous rupture of the liver in systemic lupus erythematosus. Ann Rheum Dis 33 (1974): 482-484.
- Battula N, Madanur M, Priest O, et al. Spontaneous rupture of hepatocellular carcinoma: a Western experience. Am J Surg 197 (2009): 164-167.
- Arvind N, Duraimurugan D, Rajkumar JS. Hepatic adenomatosis — a rare double complication of multiple adenoma rupture and malignant transformation. Indian J Gastroenterol 25 (2006): 209-210.
- Brown V, et al. BMJ Case Rep (2015).