Spontaneous Rupture of Spleen - A Rare Case Report
Article Information
Manohar Kachare1*, Naila Azmi2
1Professor and Head, Department of Radiodiagnosis, Government Medical College Miraj, Maharashtra, India
2Department of Radiodiagnosis, Government Medical College Miraj, Maharashtra, India
*Corresponding Author: Manohar Kachare, Professor and Head, Department of Radiodiagnosis, Government Medical College Miraj, Pandharpur Road, Maji Sainik Vasahat, Miraj, Maharashtra - 416410, India
Received: 11 May 2021; Accepted: 25 August 2021; Published: 01 October 2021
Citation: Manohar Kachare, Naila Azmi. Spontaneous Rupture of Spleen - A Rare Case Report. Journal of Radiology and Clinical Imaging 4 (2021): 125-131.
View / Download Pdf Share at FacebookAbstract
Spleen is highly vascular organ & non traumatic spleen rupture is rare association. Non traumatic splenic rupture has pathologic association with few diseases which cause splenomegaly followed by rupture. This case report describes the first and rare incidence of non-traumatic splenic rupture in a case of concealed perforated jejunal diverticulitis.
Keywords
Spleen; Rupture; Spontaneous; Diverticulitis; Splenectomy
Spleen articles; Rupture articles; Spontaneous articles; Diverticulitis articles; Splenectomy articles
Spleen articles Spleen Research articles Spleen review articles Spleen PubMed articles Spleen PubMed Central articles Spleen 2023 articles Spleen 2024 articles Spleen Scopus articles Spleen impact factor journals Spleen Scopus journals Spleen PubMed journals Spleen medical journals Spleen free journals Spleen best journals Spleen top journals Spleen free medical journals Spleen famous journals Spleen Google Scholar indexed journals Rupture articles Rupture Research articles Rupture review articles Rupture PubMed articles Rupture PubMed Central articles Rupture 2023 articles Rupture 2024 articles Rupture Scopus articles Rupture impact factor journals Rupture Scopus journals Rupture PubMed journals Rupture medical journals Rupture free journals Rupture best journals Rupture top journals Rupture free medical journals Rupture famous journals Rupture Google Scholar indexed journals Spontaneous articles Spontaneous Research articles Spontaneous review articles Spontaneous PubMed articles Spontaneous PubMed Central articles Spontaneous 2023 articles Spontaneous 2024 articles Spontaneous Scopus articles Spontaneous impact factor journals Spontaneous Scopus journals Spontaneous PubMed journals Spontaneous medical journals Spontaneous free journals Spontaneous best journals Spontaneous top journals Spontaneous free medical journals Spontaneous famous journals Spontaneous Google Scholar indexed journals Diverticulitis articles Diverticulitis Research articles Diverticulitis review articles Diverticulitis PubMed articles Diverticulitis PubMed Central articles Diverticulitis 2023 articles Diverticulitis 2024 articles Diverticulitis Scopus articles Diverticulitis impact factor journals Diverticulitis Scopus journals Diverticulitis PubMed journals Diverticulitis medical journals Diverticulitis free journals Diverticulitis best journals Diverticulitis top journals Diverticulitis free medical journals Diverticulitis famous journals Diverticulitis Google Scholar indexed journals Splenectomy articles Splenectomy Research articles Splenectomy review articles Splenectomy PubMed articles Splenectomy PubMed Central articles Splenectomy 2023 articles Splenectomy 2024 articles Splenectomy Scopus articles Splenectomy impact factor journals Splenectomy Scopus journals Splenectomy PubMed journals Splenectomy medical journals Splenectomy free journals Splenectomy best journals Splenectomy top journals Splenectomy free medical journals Splenectomy famous journals Splenectomy Google Scholar indexed journals peritonitis articles peritonitis Research articles peritonitis review articles peritonitis PubMed articles peritonitis PubMed Central articles peritonitis 2023 articles peritonitis 2024 articles peritonitis Scopus articles peritonitis impact factor journals peritonitis Scopus journals peritonitis PubMed journals peritonitis medical journals peritonitis free journals peritonitis best journals peritonitis top journals peritonitis free medical journals peritonitis famous journals peritonitis Google Scholar indexed journals Anticoagulants articles Anticoagulants Research articles Anticoagulants review articles Anticoagulants PubMed articles Anticoagulants PubMed Central articles Anticoagulants 2023 articles Anticoagulants 2024 articles Anticoagulants Scopus articles Anticoagulants impact factor journals Anticoagulants Scopus journals Anticoagulants PubMed journals Anticoagulants medical journals Anticoagulants free journals Anticoagulants best journals Anticoagulants top journals Anticoagulants free medical journals Anticoagulants famous journals Anticoagulants Google Scholar indexed journals Therapeutic thrombolysis articles Therapeutic thrombolysis Research articles Therapeutic thrombolysis review articles Therapeutic thrombolysis PubMed articles Therapeutic thrombolysis PubMed Central articles Therapeutic thrombolysis 2023 articles Therapeutic thrombolysis 2024 articles Therapeutic thrombolysis Scopus articles Therapeutic thrombolysis impact factor journals Therapeutic thrombolysis Scopus journals Therapeutic thrombolysis PubMed journals Therapeutic thrombolysis medical journals Therapeutic thrombolysis free journals Therapeutic thrombolysis best journals Therapeutic thrombolysis top journals Therapeutic thrombolysis free medical journals Therapeutic thrombolysis famous journals Therapeutic thrombolysis Google Scholar indexed journals Lithotripsy articles Lithotripsy Research articles Lithotripsy review articles Lithotripsy PubMed articles Lithotripsy PubMed Central articles Lithotripsy 2023 articles Lithotripsy 2024 articles Lithotripsy Scopus articles Lithotripsy impact factor journals Lithotripsy Scopus journals Lithotripsy PubMed journals Lithotripsy medical journals Lithotripsy free journals Lithotripsy best journals Lithotripsy top journals Lithotripsy free medical journals Lithotripsy famous journals Lithotripsy Google Scholar indexed journalsArticle Details
1. Introduction
Spleen being extremely vascular structure, splenic rupture is a fatal medical emergency [1, 2]. Although traumatic association is most common, rupture due to underlying malignancy or infection of Infectious mononucleosis, malaria besides chronic haematological abnormality which can cause splenic enlargement leading to thinning of cortex & hence making susceptible to even minor trauma is not uncommon [3]. The spontaneous rupture of spleen is rare incidence. This case is being reported from a tropical country with spontaneous spleen rupture being not attributable to malaria or infectious mononucleosis. Between 1917 to 1948 number of 64 cases and between 1950 to 2011 approximately 613 cases of spontaneous spleen rupture are well documented [3, 4].
2. Case History
A 60-year-old man admitted in hospital with a complaint of pain in left paraumbilical region & fever for 1 week. On USG abdomen there was collection in left paracolic gutter in paraumbilical region. CECT imaging had revealed – diffusely enlarged pancreas with inhomogeneous hypoen-hancement with mild peripancreatic peritoneal reflection thickening. Duodenum had nodular thickening in D2 & D3 segments. There were multiple jejunal outpouchings present from mesenteric border of jejunal loops predominantly in left lumbar & iliac regions. There was localised perforation of few of diverticula secondary to a possible background diverticulitis. There was clustering of small bowels in left half of abdomen associated with moderate localised inflam-matory changes. The diagnosis of localised perforated peri-tonitis was ascertained. There was a small rim enhancing encysted fluid collection. Free fluid collection was noted extending into left paracolic gutter reaching to left iliac fossa. There was reactive inflammation of descending colon & proximal sigmoid colon associated with congested vessels around. Imaging findings of background jejunal diverticulosis with secondary diverticulitis were seen. Localised concealed perforation of the few of the recently infla-med diverticula with resultant localised peritonitis & subacute interstitial oedematous pancreatitis was ascertained.
Under USG guidance approximately 60 cc of pus was drained from left paracolic gutter collection and patient was treated with antibiotics and anti-inflammatory for 1 week and was discharged. After 13 days patient again came with acute pain in abdomen in left hypochondriac region in afternoon. Pain had suddenly aggravated overnight. As the patient was deteriorated his abdomen was again investigated with CECT which revealed spleen of size 197 × 98 X 156 mm in mixed density, non-enhancing lesion noted in left subdiaphragmatic space in splenic fossa in subcapsular region of the spleen causing medial displacement & compr-ession of residual, normally enhancing spleen. Jejunal loops were thickened persistently although the adjacent collection was merely of 30 X 15 mm with thick enhancing wall. The imaging findings were consistent with spleen rupture. Patient was hence shifted to tertiary care centre. Hemogram revealed decreased haemoglobin to 7 gm% & leucocytosis (TLC=21000); rest of the haematological, Serum lipase was found to be 1.4 times the upper normal limit; rest of the biochemical as well as microbiological investigations were normal. Emergency splenectomy was done. Intra-operative findings showed rupture of spleen with large hematoma. The splenic vessels at hilum were normal. The enlarged ruptured spleen measured 13 × 8 × 4 cm with congestion and focal capsular tear was seen. Specimen was given for histopathological examination which revealed congested sinusoids, subcapsular haemorrhage without any other specific lesion. Splenectomy was uneventful. In between the two episode of symptoms patient had no history of trauma or any surgical intervention. Thus this case can be considered as a spontaneous rupture of spleen.
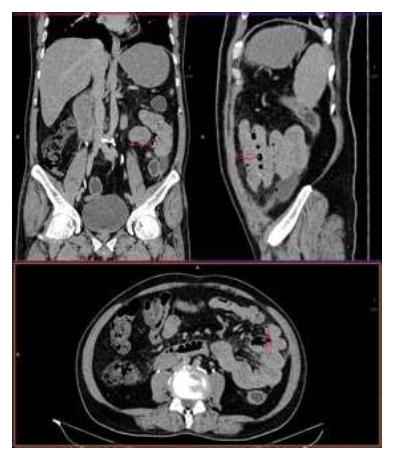
Figure 1: Perforated Jejunal diverticulum with collection and air noted within.

Figure 2: Axial CECT showing spleen with coronal & sagittal reformats 14 days prior to spontaneous rupture of spleen.
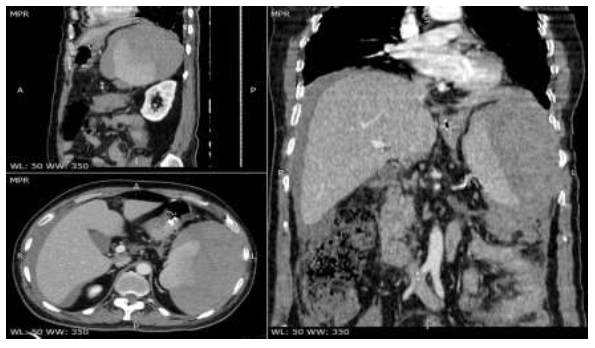
Figure 3: Post contrast study showing ruptured spleen large intrasplenic hematoma, causing a mass effect, and extensive intraperitoneal free fluid.
3. Discussion
Spleen is very vascular & functionally diverse organ meant for haematopoiesis & immunosurveillance while making interactions between the circulatory, reticuloendothelial, and immune systems [5, 6]. Traumatic spleen rupture has been well documented. Spontaneous splenic rupture is rare and predisposing conditions include haematological diseases with splenic infiltration, splenic infarcts, male gender, massive splenomegaly, angiosarcoma of the spleen & certain infections more commonly like EBV & malaria. Between 1917 to 1948 number of 64 cases and between 1950 to 2011 approximately 613 cases of spontaneous spleen rupture are well documented [3, 4].
Orloff and Peskin recognized four-step criteria for the diagnosis of spontaneous rupture consisting of 1. no history of trauma, 2. no perisplenic adhesions which support previous trauma, 3. no disease affecting the spleen, and 4. on gross and histologic examinations there is presence of a normal spleen [7]. Crate and Payne then added a fifth criterion i.e.: Full virologic studies of acute phase and convalescent sera should show no significant rise in antibody titres which suggests recent viral infection of types known to have splenic involvement [8]. The number of cases which fulfil Orloff and Peskin’s criterion is by far less. In a systemic review by F Kris Aubrey and Nicholas Sowers of 613 cases of non-traumatic spleen rupture 18% have been attributed to medical procedures while 23% being attributed to infectious disease [3]. Our case fulfilled all Orloff and Peskin’s criterion hence is reported as spontaneous spleen rupture case. Causes of Spontaneous splenic rupture is varied and although not complete the list is comprehensive [3, 9] [Table 1].
|
Cause |
Disease |
|
Infections |
Infectious mononucleosis |
|
HIV |
|
|
Hepatitis A/B/C |
|
|
Rubella |
|
|
Varicella |
|
|
Legionellosis |
|
|
Bartenellosis |
|
|
Infective endocarditis (Staphylococcus, Streptococcus, Clostridium, Actinomycosis, Pseudomonas among the top causes) |
|
|
Enteric fever |
|
|
Tuberculosis |
|
|
Syphilis |
|
|
Malaria |
|
|
Kalaazar |
|
|
Hematologic and neoplastic causes |
Haemophilia |
|
Anticoagulation |
|
|
Hemolytic anemia |
|
|
Angiosarcoma |
|
|
Choriocarcinoma |
|
|
Myeloid metaplasia/fibrosis |
|
|
Lymphoma and leukemia |
|
|
Multiple myeloma |
|
|
Polycythemia vera |
|
|
Inflammatory |
Crohn’s disease |
|
Pancreatitis |
|
|
Polyarteritis nodosa |
|
|
Lupus erythematosus |
|
|
Rheumatoid arthritis |
|
|
Infiltrative causes |
Amyloidosis |
|
Felty’s syndrome |
|
|
Sarcoidosis |
|
|
Iatrogenic |
Anticoagulants - Warfarin / Heparin |
|
Granulocyte colony stimulating factor |
|
|
Therapeutic thrombolysis |
|
|
Dialysis |
|
|
Lithotripsy |
|
|
Primary splenic disorders |
Splenic cyst |
|
Splenic angiomatosis |
|
|
Splenic peliosis |
|
|
Splenic infarctions or venous thrombosis |
|
|
Portal hypertension |
|
|
Congenital malposition (i.e. short splenic pedicle) |
|
|
Internal trauma |
Pregnancy |
|
Cough / Vomiting |
Table 1: Causes of spontaneous rupture of spleen.
The possible mechanism of spleen rupture is hypothesised as -
References
- Redmond HP, Redmond JM, Rooney BP, et al. Surgical anatomy of the human spleen. British journal of surgery 76 (1989): 198-201.
- Rhee SJ, Sheena Y, Imber C. Spontaneous rupture of the spleen: a rare but important differential of an acute abdomen. The American journal of emergency medicine 26 (2008): 733-e5.
- Aubrey-Bassler FK, Sowers N. 613 cases of splenic rupture without risk factors or previously diagnosed disease: a systematic review. BMC emergency medicine 12 (2012): 11.
- Hershey FB, Lubitz JM. Spontaneous rupture of the malarial spleen: case report and analysis of 64 reported cases. Annals of surgery 127 (1948): 40.
- De Porto AP, Lammers AJ, Bennink RJ, et al. Assessment of splenic function. European journal of clinical microbiology & infectious diseases 29 (2010): 1465-1473.
- Chadburn A. The spleen: anatomy and anatomical function. InSeminars in hematology 37 (2000): 13-21.
- Orloff M, Peskin G. Spontaneous rupture of the normal spleen; a surgical enigma. InInternational abstracts of surgery 106 (1958).
- Crate ID, Payne MJ. Is the diagnosis of spontaneous rupture of a normal spleen valid?. Journal of the Royal Army Medical Corps 137 (1991): 50-51.
- Amonkar SJ, Kumar EN. Spontaneous rupture of the spleen: three case reports and causative processes for the radiologist to consider. The British journal of radiology 82 (2009): e111-e113.
- Rice JP, Sutter CM. Spontaneous splenic rupture in an active duty Marine upon return from Iraq: a case report. Journal of medical case reports 4 (2010): 353.
- Leighton WE. Spontaneous rupture of the malarial spleen, with abstract of cases reported between 1842 and 1921. Annals of surgery 74 (1921): 13.
- Schattner A, Meital A, Mavor E. Red-flag syncope: spontaneous splenic rupture. The American journal of medicine 127 (2014): 501-502.
- Debnath D, Valerio D. Atraumatic rupture of the spleen in adults. Journal of the Royal College of Surgeons of Edinburgh 47 (2002): 437-445.
- Toubia NT, Tawk MM, Potts RM, et al. Cough and spontaneous rupture of a normal spleen. Chest 128 (2005): 1884-1886.
- King H, Shumacker Jr HB. Splenic studies: I. Susceptibility to infection after splenectomy performed in infancy. Annals of surgery 136 (1952): 239.
- Coccolini F, Montori G, Catena F, et al. Splenic trauma: WSES classification and guidelines for adult and pediatric patients. World Journal of Emergency Surgery 12 (2017): 40.
