Spontaneous Intraperitoneal Bladder Rupture with Normal Renal Indices. A Case Report of Unusual, Confusing Presentation
Article Information
Mohammed Abdulkareem Ibrahim, Morshed Ali Salah
Associate Consultant Urologist, Al Wakra General Hospital, Hammad Medical Corporation, Qatar
*Corresponding Author: Mohammed Abdulkareem Ibrahim, Associate Consultant Urologist, Al Wakra General Hospital, Hammad Medical Corporation, Qatar
Received: 29 November 2021; Accepted: 20 December 2021; Published: 05 January 2022
Citation: Ibrahim MA, Salah MA. Spontaneous Intraperitoneal Bladder Rupture with Normal Renal Indices. A Case Report of Unusual, Confusing Presentation. Archives of Clinical and Medical Case Reports 6 (2022): 1-10.
View / Download Pdf Share at FacebookAbstract
Background: Spontaneous Bladder Rupture (SBR) is one of the rare causes of acute abdomen seen in the emergency room. Almost all the reported cases of atraumatic intraperitoneal bladder rupture were associated with a state of pseudo- acute kidney injury due to resorption of leaked urine urea and creatinine through peritoneum to the blood.
Case Presentation: 25-year old lady. Presented with few hours history of sudden attack of severe lower abdominal pain associated with nausea, no vomiting, with increasing abdominal distention, no history of trauma. Vital signs were stable; however, blood pressure was decreasing. Local abdominal examination showed generalized abdominal tenderness, rigidity and guarding. Labs showed normal renal indices as well as the inflammatory parameters. The patient reported history of TURBT for a single, small PUNLMP bladder tumor 10-months before her presentation. Abdomen CT finding, Retrograde cystogram, flexible cystoscope then exploratory laparotomy confirmed the diagnosis of intraperitoneal bladder rupture. The patient went through smooth post-operative and follow up course.
Conclusion: Intraperitoneal (SBR) still could be considered as one of the serious causes of acute abdominal condition even in the absence of elevated renal indices with strong emphasis on the history of previous bladder intervention.
Keywords
Bladder tumour; Renal; Urology
Bladder tumour articles; Renal articles; Urology articles
Bladder tumour articles Bladder tumour Research articles Bladder tumour review articles Bladder tumour PubMed articles Bladder tumour PubMed Central articles Bladder tumour 2023 articles Bladder tumour 2024 articles Bladder tumour Scopus articles Bladder tumour impact factor journals Bladder tumour Scopus journals Bladder tumour PubMed journals Bladder tumour medical journals Bladder tumour free journals Bladder tumour best journals Bladder tumour top journals Bladder tumour free medical journals Bladder tumour famous journals Bladder tumour Google Scholar indexed journals COVID-19 articles COVID-19 Research articles COVID-19 review articles COVID-19 PubMed articles COVID-19 PubMed Central articles COVID-19 2023 articles COVID-19 2024 articles COVID-19 Scopus articles COVID-19 impact factor journals COVID-19 Scopus journals COVID-19 PubMed journals COVID-19 medical journals COVID-19 free journals COVID-19 best journals COVID-19 top journals COVID-19 free medical journals COVID-19 famous journals COVID-19 Google Scholar indexed journals Renal articles Renal Research articles Renal review articles Renal PubMed articles Renal PubMed Central articles Renal 2023 articles Renal 2024 articles Renal Scopus articles Renal impact factor journals Renal Scopus journals Renal PubMed journals Renal medical journals Renal free journals Renal best journals Renal top journals Renal free medical journals Renal famous journals Renal Google Scholar indexed journals Urology articles Urology Research articles Urology review articles Urology PubMed articles Urology PubMed Central articles Urology 2023 articles Urology 2024 articles Urology Scopus articles Urology impact factor journals Urology Scopus journals Urology PubMed journals Urology medical journals Urology free journals Urology best journals Urology top journals Urology free medical journals Urology famous journals Urology Google Scholar indexed journals Ultra Sound articles Ultra Sound Research articles Ultra Sound review articles Ultra Sound PubMed articles Ultra Sound PubMed Central articles Ultra Sound 2023 articles Ultra Sound 2024 articles Ultra Sound Scopus articles Ultra Sound impact factor journals Ultra Sound Scopus journals Ultra Sound PubMed journals Ultra Sound medical journals Ultra Sound free journals Ultra Sound best journals Ultra Sound top journals Ultra Sound free medical journals Ultra Sound famous journals Ultra Sound Google Scholar indexed journals treatment articles treatment Research articles treatment review articles treatment PubMed articles treatment PubMed Central articles treatment 2023 articles treatment 2024 articles treatment Scopus articles treatment impact factor journals treatment Scopus journals treatment PubMed journals treatment medical journals treatment free journals treatment best journals treatment top journals treatment free medical journals treatment famous journals treatment Google Scholar indexed journals CT articles CT Research articles CT review articles CT PubMed articles CT PubMed Central articles CT 2023 articles CT 2024 articles CT Scopus articles CT impact factor journals CT Scopus journals CT PubMed journals CT medical journals CT free journals CT best journals CT top journals CT free medical journals CT famous journals CT Google Scholar indexed journals Protein-losing enteropathy articles Protein-losing enteropathy Research articles Protein-losing enteropathy review articles Protein-losing enteropathy PubMed articles Protein-losing enteropathy PubMed Central articles Protein-losing enteropathy 2023 articles Protein-losing enteropathy 2024 articles Protein-losing enteropathy Scopus articles Protein-losing enteropathy impact factor journals Protein-losing enteropathy Scopus journals Protein-losing enteropathy PubMed journals Protein-losing enteropathy medical journals Protein-losing enteropathy free journals Protein-losing enteropathy best journals Protein-losing enteropathy top journals Protein-losing enteropathy free medical journals Protein-losing enteropathy famous journals Protein-losing enteropathy Google Scholar indexed journals surgery articles surgery Research articles surgery review articles surgery PubMed articles surgery PubMed Central articles surgery 2023 articles surgery 2024 articles surgery Scopus articles surgery impact factor journals surgery Scopus journals surgery PubMed journals surgery medical journals surgery free journals surgery best journals surgery top journals surgery free medical journals surgery famous journals surgery Google Scholar indexed journals Torticollis articles Torticollis Research articles Torticollis review articles Torticollis PubMed articles Torticollis PubMed Central articles Torticollis 2023 articles Torticollis 2024 articles Torticollis Scopus articles Torticollis impact factor journals Torticollis Scopus journals Torticollis PubMed journals Torticollis medical journals Torticollis free journals Torticollis best journals Torticollis top journals Torticollis free medical journals Torticollis famous journals Torticollis Google Scholar indexed journals
Article Details
Abbreviations:
b/m: beat/ minute; BP: Blood Pressure; CRP: C- Reactive Protein; Hb: Hemoglobin; HR: Heart Rate; INR: International Normalization Ration; KUB US: Kidney, Ureter, Bladder Ultra Sound; NR: Normal Range; OR: Operation Room; PUNLMP: Papillary Urothelial Neoplasm of Low Malignant Potential; SBR: Spontaneous Bladder Rupture; Temp.: Temperature; TURBT: Transurethral Resection of Bladder Tumor; WBC: White Blood Cells
1. Introduction
Spontaneous Bladder Rupture (SBR) is a rare and life-threatening condition making up less than 1% of all bladder injuries. Bladder rupture in the absence of trauma is a rare and serious event with a mortality rate approaching 47% due to delayed diagnosis as it could be easily missed, or difficult to be distinguished from other causes of acute abdominal pain [1]. The patients in the reported cases of (SBR) had laboratory finding of acute kidney injury with elevated serum urea nitrogen and creatinine level, which actually resulted from peritoneal resorption of urea nitrogen and creatinine from the collected urine in the peritoneal cavity, which is the key feature of urinary ascites [2]. The predisposing conditions for (SBR) are primarily either those which increase the intravesical pressure, or others which affect the bladder wall thickness and strength [3]. Moreover, delayed spontaneous bladder perforations were reported in 2-cases post Radical transurethral Resection of Bladder Tumor (TURBT) 6-months following the resection [4]. Here, we are reporting an unusual presentation of delayed (SBR) in a young lady who had positive history of previous TURBT for a small, single low malignant potential bladder tumor, unexpectedly, she had normal renal indices in the whole course of management, with minimal microscopic hematuria.
2. Case Presentation
25 years old lady, newly married, not pregnant with no known medical illness. Presented to the emergency room with few hours history of sudden attack of sever lower abdominal pain felt while she was in a social event participating in a traditional group-dancing of low activity profile. The pain started in the suprapubic area then distributed to both iliac regions. She was nauseated, without vomiting or fever. She didn’t report event of fall or trauma. She noticed progressive abdominal distention with increasing abdominal pain severity. She had difficulty in passing urine after the onset of abdominal pain, however she did not feel her bladder distended.
The patient had history of irritative voiding symptoms for about a year, investigations showed single, small, abut 1-cm, papillary bladder growth seen on the bladder dome during outpatient diagnostic flexible cystoscopy (Figure 1). 10-months before here emergency presentation, one-week after the diagnosis, she underwent cystoscopy, cold-cup biopsy for that growth with deep resection of its base by monopolar resectoscope (TURBT) in another hospital. Histopathology results showed Papillary Urothelial Neoplasm of Low Malignant Potential (PUNLMP), with no invasion to muscularis properia. Her vitals were: BP 111/72 mmHg, HR 88 b/m, Temp. 37.3 C’. Abdominal examination showed signs of peritoneal irritation, as generalized abdominal tenderness, rigidity and guarding. Laboratory parameters: WBC 9.9 x 10ˆ3/ul, Hb 12.5 g/dL, Blood Urea 5.3 mmol/L (N.R. 2.5-6.7 mmol/L), Serum Creatinine 83 umol/L (N.R. 50-98 umol/L), INR 1.3, Potassium 3.9 mmol/L, CRP < 0.3 mg/L, Urine microscopy RBC 20 /uL, WBC 14 /uL.
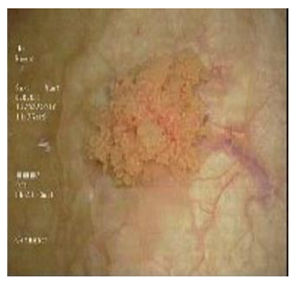
Figure 1: One-cm single bladder growth on the bladder dome.
Abdominal US showed moderate pelvic and upper abdominal ascites, partially filled urinary bladder with suspicious tubular lesion in the right iliac fossa with features suggesting acute appendicitis.Foley catheter inserted and hardly drained 100-ml of clear yellow urine. General surgeon was consulted first who requested abdominal CT with contrast to confirm the US finding of appendicitis. The Abdominal CT report was “the appendix is normal, Moderate to severe free fluid in the abdomen and pelvis, with evidence of defect seen along the inferior edge of a right-sided corpus luteal cyst. Minimal right-sided pleural effusion. Inadequately distended urinary bladder, however no obvious intraluminal lesion seen. No evidence of pneumoperitoneum” (Figure 2), accordingly the gynecologist was consulted. There was a clear discrepancy between the clinical, laboratory and radiological findings. Gynecologist and general surgeon consultations couldn’t explain clearly the underlying pathology. In light with the patient’s history of TURBT, the urologist was consulted who requested Retrograde Cystogram, which showed a bladder diverticulum seen superimposed on the dome of the urinary bladder (Figure 3) & there was leakage of contrast into the pelvis at first then into the abdominal cavity outlining the bowel loops (intraperitoneal) (Figure 4) suggest urinary bladder rupture.

Figure 2: Generalizes intraperitoneal fluid collection (Urinary Ascites).

Figure 3: Retrograde cystogram showed Diverticulum on the bladder dome, at the site of the previous TURBT.

Figure 4: Retrograde cystogram showed Intraperitoneal contrast leak around the bowel.
The patient immediately transferred to the OR for urgent exploration. Immediately before starting laparotomy incision, diagnostic flexible cystoscopy performed and showed a small diverticulum-like defect in the bladder wall on its dome with a small perforation in the very thin lining of this diverticulum (Figure 5). A lower midline laparotomy incision had been done. When the peritoneum entered, a large amount of light-yellow fluid drained from the peritoneal cavity. There was a small perforation noticed in the urinary bladder dome from the peritoneal cavity, there was no visible tumor seeding on the peritoneal cavity (Figure 6). The bladder incised anteriorly and the perforating segment of the bladder wall was excised with the covering peritoneal layer and sent for histopathology, which came free from malignant cells. Bladder and abdominal wall closed on the standard method, with urinary diversion through a urethral catheter. Her immediate post-operative and recovery period were smooth and she discharged home with the urethral Foley catheter which removed 14-days post- surgery, after the retrograde cystogram showed no contrast leak (Figure 7 and 8). Renal function tests kept normal all over the course of management. Peritoneal fluid cytology and culture showed no malignant cells and no bacterial growth, respectively.
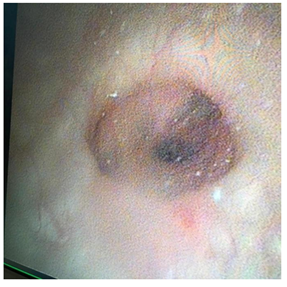
Figure 5: Perioperative Cystoscopic view of the bladder diverticulum with the perforation in the middle.
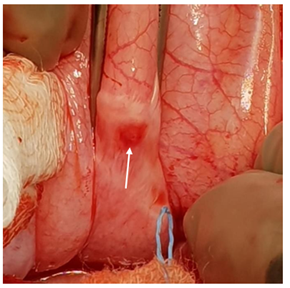
Figure 6: Intraperitoneal small bladder perforation.

Figure 7: 14-days Post- operative retrograde cystogram.
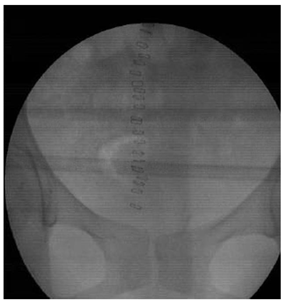
Figure 8: 14-days Post- operative retrograde cystogram (post voiding).
3. Discussion
During the initial stages of SBR, the clinical manifestations remain minimal, vague, and diffuse. Such a presentation might lead to delayed diagnosis and might be mistaken for other abdominal pathologies [5]. Therefore, clinical diagnosis of SBR requires a high index of suspicion to avoid serious morbidity or even mortality. Previous reports showed that the early diagnosis and treatment of atraumat ic SBR is strongly associated with favorable outcomes [6]. Predisposing conditions for SBR could be either those associated with increased intra-vesical pressure, as in chronic urinary retention due to neurologic or obstructive bladder disorders, or those associated with decreased strength or thickness of the bladder wall, such as diverticula, chronic inflammation, tumors and radiation cystitis [2].
Other reported cases were related to certain specific predisposing factors including binge alcohol drinking, pregnancy, diabetes, and postpartum complications [7]. Rupture of a urinary bladder from diverticulum is extremely rare, and only few cases have been reported in the literature [8]. The presentation and management of this case highlight the following important aspects: First, elevated serum creatinine is not necessarily seen in the early stages of intraperitoneal bladder rupture, as a kidney with near normal glomerular filtration rate can easily excrete the excess creatinine that is resorbed in the serum from the urinary ascites. The serum creatinine increases when the excretory capacity is overwhelmed by the resorbed creatinine load from the urinary ascites in case of delay in presentation or diagnosis [9]. Second, any therapeutic procedure performed to the bladder might predispose to SPR [10,11]. Herkommer K. et al. in 2012, described in his research that the risk of bladder rupture after TURBT was associated with female gender, decreasing body mass index, higher tumor stage, deeper infiltration and higher resection weight when risk factors were separately analyzed [12].
We noticed in our case that the resected part of the bladder wall was not healed properly resulted in iatrogenic diverticulum formation (Figure 9), which represented a significant point of weakness in the bladder wall [13]. In TURBT, although obtaining a sample of the muscle layer from the tumor base is crucial for proper staging, we believe that a deep cold cup biopsy from the tumor base, rather than deep resection by resectoscope, can provide proper histological details, especially for a single, small, suspected to be of low grade bladder tumor. Additionally, cold cup biopsy of the base of this small tumor carry a less chance of immediate or delayed perforation relate to its location in the thinnest part of the bladder wall [15]. Third, Cystoscopy, preferably flexible cystoscopy, is an informative, easy and rapid way of peri-operative assessment of a bladder rupture which can localize the lesion in relation to the position of the trigone and ureteral orifices. A lack of bladder distension during cystoscopy suggests a large perforation [14].
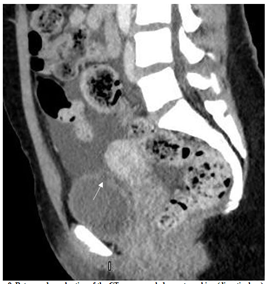
Figure 9: Retrograde evaluation of the CT scan revealed an outpouching (diverticulum) on the bladder doom at the site of previous deep resection corresponding to the cystoscopy and laparotomy findings.
4. Conclusion
The initial period following intraperitoneal bladder rupture is the most important and difficult part in the course of management owing to the indistinguishability of SBR from other causes of acute abdomen. Diagnosis of urinary ascites would be difficult in the primary stage of clinical presentation due to normal level of serum creatinine, however history of previous bladder intervention should raise the index of suspicion. Deep resection during TURBT could render the resected segment heal with a very thin mucosal layer which can perforate with simple, unexpected, increase in intravesical pressure, which we think it worth more study and investigations.
Consent
Written informed consent was obtained from the patient and her husband for publication of this Case report and any accompanying images. A copy of the written consent is available for review by the Editor of this journal.
References
- Dana Kivlin, A Case Series of Spontaneous Rupture of the Urinary Bladder. Curr Urol 8 (2014): 53-56.
- Dees A, Kluchert SA, van Vliet AC. Pseudo-renal failure associated with internal leakage of urine. Neth J Med 37 (1990): 197-201.
- Mitchell T, Al-Hayek S, Patel B, et al. Acute abdomen caused by bladder rupture attributable to neurogenic bladder dysfunction following a stroke: a case report. J Med Case Rep 5 (2011): 254.
- Kim, Yang. Delayed spontaneous perforation of urinary bladder with intraperitoneal seeding following radical transurethral resection of invasive urothelial cancer: a case report. BMC Research Notes 7 (2014): 167.
- Alhamzawi HH, Abdelrahman HM, Abdelrahman KM, et al. Delayed presentation of traumatic intraperitoneal rupture of urinary bladder. Case Rep Urol 2012 (2012): 430746.
- Daignault MC, Saul T, Lewiss RE. Bedside ultrasound diagnosis of atraumatic bladder rupture in an alcohol-intoxicated patient: a case report. Crit Ultrasound J 4 (2012): 9.
- Pradhan AA. Spontaneous rupture of bladder: a rare clinical entity. Med J Armed Forces India 3 (2007): 92-93.
- Leahy O, Grummet J. Splash! The spontaneous rupture of a bladder diverticulum: a rare cause of an acute abdomen. ANZ J Surg 83 (2013): 792-793.
- Matsumura M, Ando N, Kumabe Aet al. Pseudo-renal failure: bladder rupture with urinary ascites BMJ Case Rep (2015).
- Hayashi W, Nishino T, Namie S, et al. Spontaneous bladder rupture diagnosis based on urinary appearance of mesothelial cells: a case report. J Med Case Rep 8 (2014):46.
- Kim JH, Yang WJ. Delayed spontaneous perforation of urinary bladder with intraperitoneal seeding following radical transurethral resection of invasive urothelial cancer: a case report. BMC Res Notes 7 (2014): 167.
- Herkommer K, Hofer C, Gschwend JE, et al. Gender and body mass index as risk factors for bladder perforation during primary transurethral resection of bladder tumors. J Urol 187 (2012): 1566-1570.
- Rovner ES. Bladder and female diverticula; in Wein AJ, Kavoussi LR, Novick AC, Partin AW, Peters CA (eds): Campbell-Walsh Urology, ed 10. Elsevier Saunders (2012): 2262-2263.
- Alperin M, et al. Conservative management of postoperatively diagnosed cystotomy. Urology 73 (2009): 1163.
- Thiruchelvam J, Chong KT. Is the Use of Cold-Cup Biopsy Necessary at the End of Transurethral Resection of Bladder Tumors? Urol Nephrol Open Access J 6 (2018): 00202.
