Specific Thresholds for Emerging Cardiometabolic Risk Markers of Elevated Carotid Intima – Media Thickness (Cimt) in Uncontrolled Hypertensive Patients in A Hospital Setting in Kinshasa, Dr Congo
Article Information
Yanda Tongo Stéphane1, Longo-Mbenza Benjamin2,5* , Lelo Tshikwela Michel1, Mawalala Malengele Héritier1, Tshimpi Wola Antoine3, Makulo Risasi Jean Robert4, Kisoka Lusunsi Christian5, Monkondjimobe Etienne5,6
1Department of Radiology and Medical Imaging, University Clinics of Kinshasa, University of Kinshasa, Democratic Republic of Congo.
2Cardiology Service, Department of Internal Medicine, University Clinics of Kinshasa, University of Kinshasa, Democratic Republic of Congo.
3Hepato-gastroenterology service, Department of Internal Medicine, University Clinics of Kinshasa, University of Kinshasa, Democratic Republic of Congo.
4Nephrology Service, Department of Internal Medicine, University Clinics of Kinshasa, University of Kinshasa, Democratic Republic of Congo.
5Department of Public Health, Lomo University for Research, Kinshasa, Democratic Republic of Congo.
6Marien Ngouabi University, Brazzaville, Republic of Congo.
*Corresponding author: : LONGO-MBENZA Benjamin. MD, PhD, Dsc. Head of Lomo University of Research. Faculty of Health, University of Kinshasa. Faculty of Health Science, Private Bay XI, Mthatha 5117, Eastern Cape, South Africa.
Received: 17 July 2023; Accepted: 26 July 2023; Published: 08 September 2023
Citation: Yanda Tongo Stéphane, Longo-Mbenza Benjamin, Lelo Tshikwela Michel, Mawalala Malengele Héritier, Tshimpi Wola Antoine, Makulo Risasi Jean Robert, Kisoka Lusunsi Christian, Monkondjimobe Etienne. Specific Thresholds for Emerging Cardiometabolic Risk Markers of Elevated Carotid Intima – Media Thickness (Cimt) in Uncontrolled Hypertensive Patients in A Hospital Setting in Kinshasa, Dr Congo. Cardiology and Cardiovascular Medicine. 7 (2023): 316-323.
View / Download Pdf Share at FacebookAbstract
Background: Acute rheumatic fever (ARF) is an important public health problem in developing countries. Subclinical carditis (SCC) that is detected only by echocardiogram without audible heart murmurs is relatively common in ARF. The aim of this study was to determine the pattern of SCC in patients of ARF in a specialized center in Bangladesh.
Methods: This cross-sectional study was conducted from April 2019 to May 2021 at the National Center for Control of Rheumatic Fever and Heart Diseases. Hundred consecutive diagnosed patients of acute rheumatic fever with SCC were included in the study. Diagnosis of ARF was done according to the revised Jones criteria in 2015. A total of 362 clinically suspected patients of ARF were screened and among them, 100 patients were detected of having SCC by Doppler echocardiography.
Results: Mean age of patients with ARF and SCC was 11.8 ±3.6 years and 10.8 ±3.3 years respectively and female was predominant (52.6% in ARF and 57.7% in SCC). Majority of patients (94%) with SCC had a mitral valve involvement and isolated mitral regurgitation was the most common (84%) valvular lesion. Detected valvular lesions mostly were not severe; all the aortic regurgitation and almost all mitral regurgitation (98.8%) were mild and trivial in nature of severity.
Conclusion: Common presence of SCC among ARF patients in our study agreed with the recommendations of revised Jones Criteria. Therefore, it is suggested that echocardiography should be done in every suspected patient with ARF for early detection of subclinical carditis and to reduce morbidity.
Keywords
CMTI; TyG Index; BMI; LVMI; Central Africa; Uncontrolled Hypertension.
Article Details
1. Introduction
It is well established that a constellation of inter-correlated metabolic risk factors, termed cardiometabolic risk, promotes the incidence of atherosclerotic cardiovascular disease [1-4]. It is also established that cardiovascular diseases constitute a burden if not a public health problem in the world [5]. There are two types of cardiometabolic risk factors (CMR) as classic (aging, male sex, obesity, smoking, excess alcohol, physical inactivity and psychological stress) and emerging [6] thrombogenic conditions, homocysteine, markers of inflammation and infection, heredity (discomfort and susceptibility), chronic kidney disease and structural markers (medical imaging: thickening / CIMT / subclinical atherosclerosis without plaque against the manifest clinical atherosclerosis with plaque) [7]. Management of CMR uses sex-specific, optimal CMR thresholds [8] and ethnicity/race [9]: Framingham score for Americans, score for Europeans. With regard to sub-Saharan Africa, thresholds from Central African population studies and meta-analyses [10] have proposed optimal and specific thresholds for the whole of sub-Saharan Africa [11-13]. In the Democratic Republic of Congo (DRC), arterial hypertension, one of the major components of cardiometabolic risk, is also a health problem in hospitals and in the population of the west, north, east and south of the DRC [14-19]. Then again, hypertension is recently recognized as a cause of cardiovascular morbidity, overall mortality and cardiovascular mortality due to classic cardiovascular disease (CVD) risk factors and emerging CMR in hospitals and in populations in the DRC [20,21]. If the CMR factors emerging from the non-control of hypertension in the general population of the city of Boma, province of Kongo central, western DRC have recently been identified in the city [22], there are no scientific publications relating to the optimal and specific threshold of the CIMT of the non-control of hypertension in the hospital environment of Kinshasa, which justified the initiation of the present study with the objective of identifying the independent determinants of certain emerging CVD risk factors of the increase in CIMT discriminating between control and non-control of hypertension.
2. Materials and Methods
2.1 Nature, period and place of study
This was a cross-sectional study conducted between September 2018 and January 2021. The University Clinics of Kinshasa, the Monkole Mother and Child Hospital, the Biamba Marie Mutombo Hospital in view of their geographical location and their attendance and the richness of their technical platform served as a framework for this study. The following variables of interest were collected [number of children, duration of hypertension, Systolic blood pressure (SBP), diastolic bood pressure (DBP), Waist circumference (WC), Pulse pressure (PP), heart rate (HR), weight (W), height (H), Hip circumference (HC), fasting blood sugar, 24-hour proteinuria, albumin/creatinine ratio, CRP, total cholesterol (CT), High density lipoprotein cholesterol (HDL-C), lipoprotein cholesterol (LDL-C), triacylglycerol( TG), biological indices of adiposity]. A convenience sampling procedure was followed to select subjects. The available lifestyle data included self-reported alcohol and smoking habits. Patients who drank alcohol or smoked cigarettes regularly were considered drinkers and smokers. Data were also available for duration of hypertension, family and personal history of diabetes, hypertension, and current antihypertensive medications. After 5 minutes of relaxation, seated blood pressure (BP) was measured at each subject's left arm using an Omron MI digital electronic blood pressure monitor/pulse monitor (OMRON Corporation, Tokyo); 3 BP measurements were taken and averaged for analysis. According to the recommendations of the European Society for the Fight against Arterial Hypertension and the European Society of Cardiology issued in 2018 (SEH/SEC 2018), hypertension was defined as BP ≥ 140/90 mm Hg or current use of antihypertensives regardless of BP level(23). Cholesterol (Cholesterol Test Kit, Wybenga and Pileggi-One Step Method, Span Diagnostics Ltd) and Triglycerides (Triglyceride Test, GPO-PAP Enzymatic Method, Span Diagnostics Ltd) were measured using enzymatic methods. Low density lipoprotein cholesterol (LDL) was calculated according to Friedewald(24). The Combur test was used to assess proteinuria. Turbidimetry with automatic analyzer was used for CRP. Carotid intima-media thickness was measured at the level of the distal wall of two common carotid arteries, two centimeters upstream of the bifurcation, over a length of 10 to 20 mm using two high-definition ultrasound scanners (Acuson NX 3 from Siemens and Voluson E8 from General Electric) in Mode B with a high-frequency linear probe of 12 Mhz associated with a construction system with multi-incidence scans in order to reduce artefacts and increase the dynamics of contrast(25,26). Using automatic wall detection software loaded on the system, carotid peak and mean CIMT values were obtained. CIMT elevation was defined as an CIMT > 0.8 mm according to the generally accepted threshold(21)or > 75th percentile (0.8 mm). The patients were finally classified into two groups according to their CIMT: patients with CIMT > 0.8 mm and those with CIMT ≤ 0.8 mm.
2.2 Statistical analysis:
Categorical (qualitative) variables were represented as frequencies (n= number) and proportions (%) while quantitative variables were summarized as mean ± standard deviation. Pearson's Chi-square test or Fisher's test were used to compare the proportions between an increase in the CIMT and the absence of an increase. Student's t test was used to compare the means between the increase in the CIMT and the absence of increase. The Receiver Operating Characteristic (ROC) curves evaluated the diagnostic values of the CVD risks factors markers with optimal and specific thresholds being able to discriminate the increase in the CIMT. Binary logistic regression-type multivariate analysis with an ascending stepwise strategy was used to identify emerging morphological markers and emerging circulating markers independently associated with the increase in the CIMT after adjustment on the variables of confusion. The value P < 0.05 being considered as the threshold of statistical significance. All analyzes were performed using EPI-INFO 2000 software and Statistical Package for Social Science (SSPS) on Windows versions 16, 19 and 20 (SSPS Inc, Chicago, Illinois, USA).
3. Results
A total of 280 hypertensive patients were examined on 140 men matched to 140 women according to age.
Table 1 compares the means of the general characteristics between men and women who are not matched according to the CIMT, age, socioeconomic level [76.4% (n=214) with an irregular income versus 23.6 % (n=66) with a regular monthly income], marital status [72.5% (n=203) of married people; 2.9% (n=8) of divorcees; 18.9% (n=53) of widowers and 5.5% (n=16) of single people], smoking (0% of smokers), mobility (100% of sedentary people) and educational level [14.3 % (n=40) of primary level; 33.2% (n=93) secondary level; 23.9% (n=67) at higher level and 28.6% (n=80) at postgraduate level]; except for the majority of comparable general characteristics (P ≥ 0.05).
Table 1: Sex and markers
|
Variables |
Men |
Women |
P |
|
Mean ± SD |
Mean ± SD |
||
|
Years |
63±10.3 |
60.2 ± 10.6 |
0.025 |
|
IVA |
2.4 ± 1 |
3.9 ± 2.6 |
< 0.0001 |
|
CT (mg/dl) |
188.6±39.5 |
200.4 ±45.9 |
0.022 |
|
LDL-c (mg/dl) |
112.7±29.5 |
121.3±30.2 |
0.017 |
|
LVMI (g/m²) |
119.5±11.1 |
110.9 ±10.1 |
< 0.0001 |
|
TyG-BMI |
232.9±45 |
259.7±54.9 |
< 0.0001 |
|
HC (cm) |
95.5±11.2 |
99.4±13 |
0.008 |
|
WC/HC |
1.02 ± 0.06 |
0.97 ± 0.06 |
< 0.0001 |
Abbreviations IVA: Visceral adiposity index, CT: total cholesterol, LDL-c: Low density lipoprotein-cholesterol, LVMI: left ventricular mass index, TyG Triglyceride Glucose Index (TyG index), -BMI: Body mass index, HC: hip circumference, WC: waist circumference HC hip circumference.
Mean values of advancing age, visceral adiposity index were significantly (P < 0.05) higher in men than in women, while mean values of CT, LDL-c, Left Ventricular mass index (LVMI), trigluceride-glucose index (TyG) – Boby Mass Index (BMI), WC/HC were significantly higher in women.
There was a significant bivariate correlation between all structural markers, all biomarkers of CMR and the increase in CIMT ≥ 0.8 mm in the study population: WC/H (P=0.05), urinary albumin/creatinine ratio (P < 0.001), IVA (P < 0.049), TG/HDL (P < 0.001), LVMI (P= 0.026), Sololow-Lyon (P=0.007), TyG Index (P < 0.001), TyG-BMI (P < 0.001), TG/HDL (P < 0.001), CT/HDL (P=0.007), LDL-C/HDL-C (P=0.003), Non-HDL (P=0.005), HC ( P<0.001), SBP (P<0.001) (results not shown).
After adjustment for WC/H, IVA, TG/HDL-C, Sokolow-Lyon, TyG-index, TyG-BMI, CT/HDL, LDL/HDL and Non-HDL-c as confounding variables in the multivariate regression type model binary logistic, only the quantitative values of urinary albumin/creatinine ratio, BMI, LVMI, TyG Index, HC and SBP were identified as independent, important and highly significant determinants of subclinical atherosclerosis according to the CIMT ≥ 0.8 mm in the study population (Table 2).
Table 2: Logistic regression predicting CIMT ≥ 0.8 mm by some independent determinants (Hosmer and Lemeshow test = 17.508; P= 0.025)
|
B |
SE |
Wald |
DL |
Exp(B) (95% CI) |
P |
|
|
Independent determinants |
||||||
|
Urinary albumin/creatinine (mg/g) |
0.757 |
0.31 |
5,950 |
1 |
2.131 (1.160-3.915) |
0.015 |
|
BMI |
-0.06 |
0.02 |
8,899 |
1 |
0.942 (0.905-0.980) |
0.003 |
|
LVMI (g/m²) |
-0.032 |
0.015 |
4,388 |
1 |
0.968 (0.939-0.998) |
0.036 |
|
TyG-Index |
2,072 |
0.426 |
23,666 |
1 |
7,938 (3,445-18,288) |
< 0.0001 |
|
Constant |
-22.028 |
3,601 |
37,417 |
1 |
< 0.0001 |
Abbreviations : Body Mass Index (BMI), Left ventricular mass index (LVMI), Triglyceride Glucose Index (TyG index).
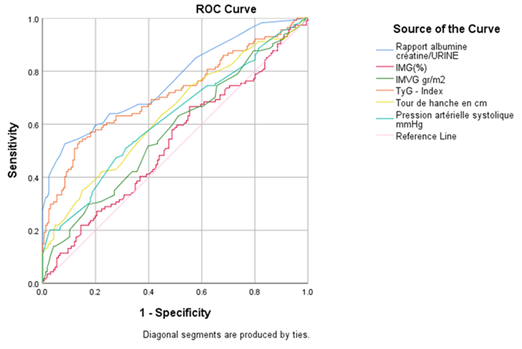
Thus Table 3 and Figure 1 with the ROC curves were used to produce the optimal and specific thresholds for predicting subclinical atherosclerosis according to the CIMT ≥ 0.8 mm in hypertensives in a Kinshasa hospital setting: albumin/creatinine ratio urine ≥ 24.5 mg/g (sensitivity = 65% and specificity = 64%), LVMI ≥ 115 g/m² (sensitivity = 60.2% and specificity = 52%); TyG Index ≥ 8.6 (sensitivity = 70.2% and specificity = 56%), HC ≥ 97 cm (sensitivity = 63.2% and specificity 55%) and SBP ≥ 140 mm Hg (sensitivity = 60% and specificity = 63%).
Table 3: Characteristics of ROC curves discriminating the presence and absence of subclinical atherosclerosis according to CIMT ≥ 0.8 mm
|
Area /zone |
ES |
CI (95%) |
P |
|
|
Urinary albumin/creatinine |
0.763 |
0.03 |
0.705-0.821 |
< 0.0001 |
|
LVMI |
0.573 |
0.035 |
0.505-0.642 |
0.037 |
|
TyG Index |
0.714 |
0.33 |
0.650-0.777 |
< 0.0001 |
|
HC |
0.637 |
0.034 |
0.570-0.704 |
< 0.0001 |
|
SBP |
0.621 |
0.035 |
0.554-0.689 |
< 0.0001 |
Abbreviations: Receiver Operating Characteristic (ROC) Left ventricular mass index (LVMI), Triglyceride Glucose Index (TyG index), Hip circumference (HC), Systolic blood pressure (SBP).
3. Discussion
This study explored the specific thresholds of structural markers and emerging circulating markers (biomarkers) discriminating the increase and the absence of the increase in the CIMT in controlled and uncontrolled arterial hypertension in Kinshasa hospital setting.
3.1 Uncontrolled high blood pressure:
As reported in sub-Saharan Africa, this study reported 72.9% of uncontrolled hypertensive patients in hospitals in Kinshasa, DR Congo [11,22,27]. Extent of uncontrolled high blood pressure in hospitals in Kinshasa, DR Congo could be explained by poverty [12,22], ignorance of hypertension, therapeutic non-compliance and the political commitment of the health system [22,28]. On the other hand, the prevalence of uncontrolled hypertension in the present study presented an epidemic and multiple appearance (72.9% for this study conducted from September 2018 to January 2021) compared to the other studies [22].
3.2 Subclinical atherosclerosis according to the CIMT:
The present study established the optimal and specific threshold of subclinical atherosclerosis in uncontrolled hypertensives of the order of CIMT > 0.8 mm, an emerging structural marker of subclinical atherosclerosis.
The cut-off for CIMT > 0.8 mm in this study was comparable to the cut-off reported in the literature [29].
3.3 Emerging markers of subclinical atherosclerosis risk:
The present study demonstrated the superiority of emerging markers compared to traditional markers in terms of cardiometabolic risk according to CIMT > 0.8 mm (subclinical atherosclerosis). Indeed, the WC/H, IVA, TG/HDL, Sokolow-Lyon, TyG-index, TyG-IMC, CT/HDL, LDL-C/HDL-C and Non-HDL-C were only univariate associated factors of the CIMT > 0.8 mm whereas the emerging markers urinary albumin/creatinine, BMI, LVMI, TyG Index were identified as independent and significant determinants of subclinical atherosclerosis according to the CIMT > 0.8 mm in the present study.
3.4 The albumin/creatinine ratio:
Several recent studies have identified the albumin/creatinine ratio as an independent determinant of CIMT > 0.85 mm [13]. Indeed, an CIMT value > 0.8 mm suggests microangiopathy, macroangiopathy around subclinical atherosclerosis, diabetes mellitus, renal impairment and mortality in several countries [14,29]. Several studies in affluent populations have also demonstrated that the urinary albumin/creatinine ratio is similar to brachial-ankle pulse wave velocity (Ba-PWV) and Abnormal ankle-brachial index (ABI) in predicting peripheral vascular disease [15].
3.5 Body Mass Index (BMI), as visceral obesity:
As reported by the literature, the present study demonstrated a positive and very significant correlation between the increase in BMI and the increase in CIMT which is also a risk factor for ischemic heart disease and stroke in globally hypertensive patients. Uncontrolled [16]. The IMG, a significant reflection of trunk fat, is more powerful than the body mass index (general and global obesity) [16], waist circumference (abdominal fat) and WC/HC ratio in the prediction of metabolic syndrome and ischemic heart disease [30].
3.6 Left ventricular mass index (LVMI):
An important, positive and significant association between the increase in CIMT and an increase in LVMI, a structural marker of trunk fat, has been demonstrated by the present study while corroborating certain results reported in the literature [16]. Thus the increase in LVMI leads to a dysfunction of the left ventricular function evaluated by the systolic ejection fraction [16], left ventricular hypertrophy and myocardial infarction. There is a strong correlation between LVMI and diabetes mellitus, hypertension, active smoking, advancing age and general obesity [16].
3.7 Triglyceride Glucose Index (TyG index)
As recently demonstrated by several scientific works in the literature [31], the elevation of the TyG index, a biomarker reflecting insulin resistance (IR) and menopause [17] and severity of coronary damage was significantly correlated with CIMT, a structural marker of subclinical atherosclerosis [17]. The present study did not show a confounding effect of sex on the association between the proportional increase in TyG index and subclinical atherosclerosis measured by CIMT in some studies in the literature [17] whereas studies in the literature show a disparity in the proportion of subclinical atherosclerosis defined by the CIMT between the group of patients with a high TyG index and the group of patients with a low TyG index according to sex: deleterious impact linked to the female sex in this disparity [17]. The TyG index threshold (≥ 8) observed in the present study was also comparable to the thresholds of 0.75 – 8.8 respectively observed in Congo-Brazzaville and in other non-African countries [32].
In the Banotous of Brazzaville, Republic of Congo, increased neck circumference and TyG index are also associated with insulin resistance [32]. The TyG index associated with subclinical atherosclerosis measured by CIMT is higher in hypertensives than in non-hypertensives in Taiwan [33]. Indeed, the transformation of the increase in CIMT into plaque formation (> 1.5 mm) of the carotid artery is formed by the aggregation of mechanisms involving platelets, vascular smooth muscles, oxidation of lipids and the increase in TyG index which is based on the IR in the present study and in other studies [33,34].
3.8 Strengths and limitations of the study:
The present study was limited by a hospital-based approach and a small sample size without considering time as suggested by other studies in the literature [17,34]. On the other hand, the strength of the use of mathematical models such as ROC curves and logistic regression has been demonstrated by the present study in Bantu hypertensives in Central Africa globally with uncontrolled arterial hypertension.
Implications in public health:
The results relating to the structural markers and to the biomarkers of imaging of the CIMT produced by the present study will be necessary for the prediction of insulin resistance, metabolic syndrome, ischemic heart disease, stroke, micro and macro-angiopathy. , peripheral vascular pathology in hypertensive patients in hospitals in Kinshasa, DR Congo(34). Subclinical atherosclerosis and advanced manifest atherosclerosis in the form of plaques in the carotid artery should be recognized as a multifactorial disease so that medical imaging specialists and clinicians including cardiologists recognize personalized medicine, precision medicine and preventive medicine according to certain complex factors such as blood flow turbulence, inflammation and the deposition of lipids in the intima media(18).
The results of the present study, based on the pathophysiology of infra-clinical atherosclerosis according to the increase in the CIMT, will help the early and precise diagnosis followed by an early and scientific treatment in hypertensive patients in a hospital environment in Kinshasa.
Conclusion:
The present study identified the independent determinants of the increase in CIMT in globally uncontrolled hypertensives in a hospital setting in Kinshasa, DR Congo.
Thus, the optimal and specific thresholds for subclinical atherosclerosis were as follows: the urinary albumin/creatinine ratio, TyG Index, BMI and LVMI in the sense of health promotion and the prevalence of atherosclerosis in taking in charge of hypertensives in hospitals in Kinshasa, DR Congo.
State of knowledge on the subject
- Importance and scientific knowledge provided by this study according to the literature
- The importance of the present study was underlined during the section of the introduction relating to the problem as opposed to the problem of the thickness CIMT as a marker of infra clinical atherosclerosis and the cardiometabolic risk in Caucasian population and Asians.
Contribution of our study to knowledge
- Thus, it is the first time that the CIMT threshold ≥ 0.8 mm is defined as a state of subclinical atherosclerosis/cardiometabolic risk in uncontrolled hypertensive patients in Kinshasa according to the ROC curve.
- This is also the first time that the determinants of CIMT ≥ 0.8 mm have been identified herein.
List of Abbreviation
Abnormal ankle-brachial index (ABI)
Brachial-ankle pulse wave velocity (Ba-PWV)
Body Mass Index (BMI),
Cardiometabolic risk factors (CMR)
Carotid intima – media thickness (CIMT)
Centre Hospitalier Mère et Enfant Monkole (CHME)
Classic cardiovascular disease (CVD)
Cliniques Universitaires de Kinshasa (CUK),
Diastolic bood pressure (DBP)
Heart rate HR
Height (H)
Hip circumference (HC)
High density lipoprotein cholesterol (HDL-C)
Hôpital Biamba Marie Mutombo (HBMM)
Left ventricular mass index (LVMI)
Lipoprotein cholesterol (LDL-C)
Pulse pressure (PP)
Systolic blood pressure (SBP)
Total cholesterol (CT)
Triacylglycerol (TG)
Triglyceride Glucose Index (TyG index)
Receiver Operating Characteristic (ROC)
Waist circumference (WC)
Weight (W)
Declarations
Ethics approval and consent to participate
To carry out this study, the protocol was submitted to the scientific committee of the Department of Internal Medicine of the University Clinics of Kinshasa and to the ethics committee of the School of Public Health of the University of Kinshasa acting as National Ethics Committee. (Approval Number: ESP/CE/076B/2018).
After explanation of the objectives of the study, its conduct, its safety and its merits, informed consent was obtained from the study participants respecting confidentiality in accordance with the Helsinki protocol.
Consent for publication:
not applicable.
Informed consent and data privacy:
The authors declare that the article does not contain any personal data that could identify the patient.
Declaration of interests:
The authors declare that they have no conflicts of interest.
Funding:
This study received no specific funding from any public, commercial or non-profit agency.
All authors certify compliance with the criteria of the International Committee of Medical Journal Editors regarding their contribution to the article.
Authors' contributions
Yanda S., Longo-mbenza B., Lelo M., Makulo JR. Tshimpi A., Mawalala H., Kisoka C. and Monkondjimobe E. made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; All authors gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Acknowledgements:
Not applicable
References
- Ponte-Negretti CI, Wyss F, Piskorz D, et al. Consenso latinoamericano para el manejo del riesgo residual cardiometabólico. Consenso realizado por la Academia Latinoamericana de Lipidología y Riesgo Cardiometabólico (ALALIP), con el aval de la Sociedad Interamericana de Cardiología (SIAC), la Sociedad Interamericana de Aterosclerosis (IAS) y el Colegio Panamericano de Endotelio (PACE). ACM 92 (2021): 6601.
- Kinoshita M, Yokote K, Arai H, et al. Japan Atherosclerosis Society (JAS) Guidelines for Prevention of Atherosclerotic Cardiovascular Diseases 2017. J Atheroscler Thromb 25 (2018): 846-984.
- Florido R, Zhao D, Ndumele CE, et al. Physical Activity, Parental History of Premature Coronary Heart Disease, and Incident Atherosclerotic Cardiovascular Disease in the Atherosclerosis Risk in Communities (ARIC) Study. JAHA [Internet] 5 (2022). 003505
- Bays HE, Taub PR, Epstein E, et al. Ten things to know about ten cardiovascular disease risk factors. American Journal of Preventive Cardiology5 (2021): 00149.
- Roth GA, Mensah GA, Johnson CO, et al. Global Burden of Cardiovascular Diseases and Risk Factors, 1990–2019. Journal of the American College of Cardiology76 (2020): 2982-3021.
- Keage HAD, Feuerriegel D, Greaves D, et al. Increasing Objective Cardiometabolic Burden Associated With Attenuations in the P3b Event-Related Potential Component in Older Adults. Front Neurol 11 (2020): 643.
- Pacifico L, Perla FM, Tromba L, et al. Carotid Extra-Media Thickness in Children: Relationships With Cardiometabolic Risk Factors and Endothelial Function. Front Endocrinol 11 (2020): 574216.
- de Jong M, Oskam MJ, Sep SJS, et al. Sex differences in cardiometabolic risk factors, pharmacological treatment and risk factor control in type 2 diabetes: findings from the Dutch Diabetes Pearl cohort. BMJ Open Diab Res Care 8 (2020): 001365.
- Amabile N, Cheng S, Renard JM, et al. Association of circulating endothelial microparticles with cardiometabolic risk factors in the Framingham Heart Study. European Heart Journal 35 (2014): 2972-2979.
- Schram A, Labonté R, Sanders D. Urbanization and International Trade and Investment Policies as Determinants of Noncommunicable Diseases in Sub-Saharan Africa. Progress in Cardiovascular Diseases 56(2013): 281-301.
- Mohamed SF, Uthman OA, Caleyachetty R, et al. Uncontrolled hypertension among patients with comorbidities in sub-Saharan Africa: protocol for a systematic review and meta-analysis. Syst Rev 9 (2020): 16.
- Sumaili EK, Cohen EP, Zinga CV, et al. High prevalence of undiagnosed chronic kidney disease among at-risk population in Kinshasa, the Democratic Republic of Congo. BMC Nephrol 10 (2009): 18.
- Kweon SS, Shin MH, Lee YH, et al. Higher normal ranges of urine albumin-to-creatinine ratio are independently associated with carotid intima-media thickness 112 (2012).
- Poredos P, Jezovnik MK. Preclinical carotid atherosclerosis as an indicator of polyvascular disease: a narrative review. Annals of Translational Medicine 9 (2021): 10.
- Liu S, Niu J, Wu S, et al. Urinary albumin-to-creatinine ratio levels are associated with subclinical atherosclerosis and predict CVD events and all-cause deaths: a prospective analysis. Open access 11 (2021): 040890.
- Evensen K, Sarvari SI, Rønning OM, et al. Carotid artery intima-media thickness is closely related to impaired left ventricular function in patients with coronary artery disease: a single-centre, blinded, non-randomized study 7 (2014): 39.
- Lu YW. Gender difference in the association between TyG index and subclinical atherosclerosis: results from the I-Lan Longitudinal Aging Study 20 (2021): 206.
- Andelovic K, Winter P, Jakob PM, et al. Evaluation of Plaque Characteristics and Inflammation Using Magnetic Resonance Imaging 9 (2021): 185.
- Katchunga PB, Mirindi P, Baleke A, Ntaburhe T, et al. The trend in blood pressure and hypertension prevalence in the general population of South Kivu between 2012 and 2016: Results from two representative cross-sectional surveys-The Bukavu observational study. PLoS One 14 (2019): 0219377.
- Longo-Mbenza B, Ngoma DV, Nahimana D, et al. Screen detection and the WHO stepwise approach to the prevalence and risk factors of arterial hypertension in Kinshasa. Eur J Cardiovasc Prev Rehabil 15(2008): 503-508.
- M’Buyamba-Kabangu J, Disashi T, Kayembe PK, et al. Pulse pressure, renal function and mortality in hospitalized Congolese patients with arterial hypertension. Annales africaines de medicine 2 (2009): 231-239.
- Nimi BM, Nkemfuni TM, Zeba GK, et al. Factors of Uncontrolled Blood Pressure in Hypertensive Patients with Chronic Kidney Disease in the City of Boma. European Journal of Preventive Medicine 10 (2022): 1-6.
- Williams B, Mancia G, Spiering W, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur Heart J 39 (2018): 3021-3104.
- Wt F, Ri L, Ds F. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clinical chemistry [Internet] 18 (2022): 499-502.
- Takiuchi S, Kamide K, Miwa Y, et al. Diagnostic value of carotid intima-media thickness and plaque score for predicting target organ damage in patients with essential hypertension. J Hum Hypertens 18 (2004): 17-23.
- Herinirina NF, Rajaonarison LHNON, Herijoelison AR, et al. Carotid intima-media thickness and cardiovascular risk factors. The Pan African Medical Journal [Internet] 21 (2015): 153.
- Essayagh T, Essayagh M, El Rhaffouli A, et al. Prevalence of uncontrolled blood pressure in Meknes, Morocco, and its associated risk factors in 2017. PLoS One 14 (2019): 0220710.
- Longo-mbenza B, Agongola F, Kasiam MJ bosco, et al. Positive correlation between waist circumference, HDL-Cholesterol and Total Cholesterol in central africans with congestive heart failure: reverse epidemiology and u-relationship in cardiovascular risk 26 (2007): 183-190.
- Longo-Mbenza B, Nsenga JN, Mokondjimobe E, et al. Helicobacter pylori infection is identified as a cardiovascular risk factor in Central Africans. Vasc Health Risk Manag 6 (2012): 455-461.
- Park JK, Park H, Kim KB. The relationship between distribution of body fat mass and carotid artery intima-media thickness in Korean older adults. J Phys Ther Sci 27 (2015): 3141-3146.
- Wei A, Liu J, Wang L, et al. Traditional and novel risk factors of premature coronary heart disease and correlation between Triglyceride-glucose index and multivessel disease 12 (20220):
- Mafuta-Munganga D, Sakou RFEL, Longo-Mbenza B, et al. Neck Circumference Is Better Associated Than Waist Circumference at Insulin Resistance in Bantu Population from Brazzaville in Republic of Congo. Science Journal of Clinical Medicine 10 (2021): 7.
- Alizargar J, Bai CH. Comparison of Carotid Ultrasound Indices and the Triglyceride Glucose Index in Hypertensive and Normotensive Community-Dwelling Individuals: A Case Control Study for Evaluating Atherosclerosis. Medicina (Kaunas) 54 (2018): 71.
- Wang A, Tian X, Zuo Y, et al. Change in triglyceride-glucose index predicts the risk of cardiovascular disease in the general population: a prospective cohort study. Cardiovasc Diabetol 20 (2021): 113.