Sonographic Findings of NS1 Positive Dengue Fever Patients and Its Correlation with Platelet Count
Article Information
Dr. Mst. Maksuda Khatun1, Dr. Mohammad Shahin Akter2, Dr. Salma Shahnawaz Parvin3, Dr. Md. Towrit Reza4
1Assistant Professor, Department of Radiology and Imaging, Bangabandhu Sheikh Mujib Medical College (BSMMC), Faridpur, Bangladesh, orcid id: 0000-0001-6092-6946
2Assistant Professor, Department of Orthopedics, Bangabandhu Sheikh Mujib Medical College (BSMMC), Faridpur, Bangladesh, orcid id: 0000-0001-6092-6946
3Assistant Professor, Department of Radiology and Imaging, Bangabandhu Sheikh Mujib Medical College (BSMMC), Faridpur, Bangladesh, orcid id: 0000-0001-6092-6946
4Assistant Professor, Department of Radiology and Imaging, Bangabandhu Sheikh Mujib Medical College (BSMMC), Faridpur, Bangladesh, orcid id: 0000-0001-6092-6946
*Corresponding Author: Mst. Maksuda Khatun. Assistant Professor, Department of Radiology and Imaging, Bangabandhu Sheikh Mujib Medical College (BSMMC), Faridpur, Bangladesh
Received: 09 January 2023; Accepted: 19 January 2023; Published: 15 May 2023
Citation: Kamal SMS, Borhanuddin M, Fatema K, Akter SR, Shams F, Ferdous J, Shima KH. Sonographic Findings of NS1 Positive Dengue Fever Patients and Its Correlation with Platelet Count. Journal of Radiology and Clinical Imaging. 6 (2023): 118-122
View / Download Pdf Share at FacebookAbstract
Background: Dengue fever is a significant threat to human populations, particularly in tropical and subtropical regions. Usually, it is transmitted from human to human by the Aedes aegypti mosquito. In detecting dengue infections ultrasonography is used because of its ability to detect plasma leakage signs as well as prediction of disease severity. For the better management of dengue, we require more research-based information regarding the sonographic findings of NS1-positive dengue fever patients and its correlation with platelet count.
Aim of the study: This study aimed to assess the sonographic findings of NS1-positive dengue fever patients and their correlation with platelet count.
Methods: This prospective observational study was conducted in the Radiology & Imaging department, Kurmitola General Hospital, Dhaka, Bangladesh during the period from July 2019 to December 2019. In total450 NS1-positive dengue fever patients were enrolled in this study as study subjects. As per the inclusion criteria of this study, NS1antigen (for dengue) positive patients from different age groups of either gender, scheduled for USG of the Whole abdomen were included. According to the exclusion criteria of this study, patients without proper adequate diagnostic reports were excluded. All the demographic, clinical and diagnostic information of the participants was recorded and analyzed by using MS Excel and SPSS version 23.0 program as per necessity.
Results: In this study, as per the specific abnormal sonographic report, gallbladder wall thickness (49%), ascites (27%), and right pleural effusion (25%) were found in ≥25% of cases. In comparing the platelet count (x10³) between patient groups of normal and abnormal sonographic findings we found significantly (Extremely) lower platelet count in the abnormal sonographic findings group where the p<0.001. In comparing against specific abnormal sonographic findings cases, we observed that, in GB wall thickness, pericholecystic collection, fatty liver, hepatitis, ascites, right pleural effusion, left pleural effusion, bilateral pleural effusion and pericardial effusion cases, the platelet counts were extremely significantly lower than normal group patients where the p<0.001. In hepatomegaly cases, we found a significant correlation but in splenomegaly, we did not find any correlation with platelet count.
Conclusion: Gallbladder wall thickness, ascites and right pleural effusion are the most common abnormal sonographic findings of NS1-positive dengue fever patients.NS1-positive dengue fever patients have a significantly negative correlation with platelet count.
Keywords
Dengue fever; Aedes aegypti mosquito; Platelet count; Ultrasonography; NS1 positive
Traumatic Brain articles, Computed Tomographyarticles
Dengue fever articles Dengue fever Research articles Dengue fever review articles Dengue fever PubMed articles Dengue fever PubMed Central articles Dengue fever 2023 articles Dengue fever 2024 articles Dengue fever Scopus articles Dengue fever impact factor journals Dengue fever Scopus journals Dengue fever PubMed journals Dengue fever medical journals Dengue fever free journals Dengue fever best journals Dengue fever top journals Dengue fever free medical journals Dengue fever famous journals Dengue fever Google Scholar indexed journals Aedes aegypti mosquito articles Aedes aegypti mosquito Research articles Aedes aegypti mosquito review articles Aedes aegypti mosquito PubMed articles Aedes aegypti mosquito PubMed Central articles Aedes aegypti mosquito 2023 articles Aedes aegypti mosquito 2024 articles Aedes aegypti mosquito Scopus articles Aedes aegypti mosquito impact factor journals Aedes aegypti mosquito Scopus journals Aedes aegypti mosquito PubMed journals Aedes aegypti mosquito medical journals Aedes aegypti mosquito free journals Aedes aegypti mosquito best journals Aedes aegypti mosquito top journals Aedes aegypti mosquito free medical journals Aedes aegypti mosquito famous journals Aedes aegypti mosquito Google Scholar indexed journals Platelet count articles Platelet count Research articles Platelet count review articles Platelet count PubMed articles Platelet count PubMed Central articles Platelet count 2023 articles Platelet count 2024 articles Platelet count Scopus articles Platelet count impact factor journals Platelet count Scopus journals Platelet count PubMed journals Platelet count medical journals Platelet count free journals Platelet count best journals Platelet count top journals Platelet count free medical journals Platelet count famous journals Platelet count Google Scholar indexed journals Ultrasonography articles Ultrasonography Research articles Ultrasonography review articles Ultrasonography PubMed articles Ultrasonography PubMed Central articles Ultrasonography 2023 articles Ultrasonography 2024 articles Ultrasonography Scopus articles Ultrasonography impact factor journals Ultrasonography Scopus journals Ultrasonography PubMed journals Ultrasonography medical journals Ultrasonography free journals Ultrasonography best journals Ultrasonography top journals Ultrasonography free medical journals Ultrasonography famous journals Ultrasonography Google Scholar indexed journals NS1 positive articles NS1 positive Research articles NS1 positive review articles NS1 positive PubMed articles NS1 positive PubMed Central articles NS1 positive 2023 articles NS1 positive 2024 articles NS1 positive Scopus articles NS1 positive impact factor journals NS1 positive Scopus journals NS1 positive PubMed journals NS1 positive medical journals NS1 positive free journals NS1 positive best journals NS1 positive top journals NS1 positive free medical journals NS1 positive famous journals NS1 positive Google Scholar indexed journals Traumatic brain injury articles Traumatic brain injury Research articles Traumatic brain injury review articles Traumatic brain injury PubMed articles Traumatic brain injury PubMed Central articles Traumatic brain injury 2023 articles Traumatic brain injury 2024 articles Traumatic brain injury Scopus articles Traumatic brain injury impact factor journals Traumatic brain injury Scopus journals Traumatic brain injury PubMed journals Traumatic brain injury medical journals Traumatic brain injury free journals Traumatic brain injury best journals Traumatic brain injury top journals Traumatic brain injury free medical journals Traumatic brain injury famous journals Traumatic brain injury Google Scholar indexed journals low and middle-income countries articles low and middle-income countries Research articles low and middle-income countries review articles low and middle-income countries PubMed articles low and middle-income countries PubMed Central articles low and middle-income countries 2023 articles low and middle-income countries 2024 articles low and middle-income countries Scopus articles low and middle-income countries impact factor journals low and middle-income countries Scopus journals low and middle-income countries PubMed journals low and middle-income countries medical journals low and middle-income countries free journals low and middle-income countries best journals low and middle-income countries top journals low and middle-income countries free medical journals low and middle-income countries famous journals low and middle-income countries Google Scholar indexed journals subdural hematoma articles subdural hematoma Research articles subdural hematoma review articles subdural hematoma PubMed articles subdural hematoma PubMed Central articles subdural hematoma 2023 articles subdural hematoma 2024 articles subdural hematoma Scopus articles subdural hematoma impact factor journals subdural hematoma Scopus journals subdural hematoma PubMed journals subdural hematoma medical journals subdural hematoma free journals subdural hematoma best journals subdural hematoma top journals subdural hematoma free medical journals subdural hematoma famous journals subdural hematoma Google Scholar indexed journals CT scan articles CT scan Research articles CT scan review articles CT scan PubMed articles CT scan PubMed Central articles CT scan 2023 articles CT scan 2024 articles CT scan Scopus articles CT scan impact factor journals CT scan Scopus journals CT scan PubMed journals CT scan medical journals CT scan free journals CT scan best journals CT scan top journals CT scan free medical journals CT scan famous journals CT scan Google Scholar indexed journals skull fracture articles skull fracture Research articles skull fracture review articles skull fracture PubMed articles skull fracture PubMed Central articles skull fracture 2023 articles skull fracture 2024 articles skull fracture Scopus articles skull fracture impact factor journals skull fracture Scopus journals skull fracture PubMed journals skull fracture medical journals skull fracture free journals skull fracture best journals skull fracture top journals skull fracture free medical journals skull fracture famous journals skull fracture Google Scholar indexed journals
Article Details
1. Introduction
Traumatic brain injury (TBI), a form of acquired brain injury, occurs when a sudden trauma causes damage to the brain. TBI can result when the head suddenly and violently hits an object, or when an object pierces the skull and enters brain tissue. It remains the most common cause of death following trauma, with particularly high mortality and morbidity in low and middle-income countries (LMIC) like Bangladesh [1]. Head injury according to WHO will surpass many diseases as the major cause of death and disability by the year 2020 [2]. High illness and death rates in low and middle-income countries are present to traumatic head injuries [3]. Traumatic brain injury can be defined as changed brain function, confusion, coma and change in consciousness or neuromotor deficit [4]. TBI is very much related to traumatic head injuries which occur mostly due to RTA in young people and fall history in children [5, 6]. Male are highly involved because they are mostly outdoors like driving, vehicles, and working outdoors [6-10]. Previous study found intra-cerebral hematoma (46.33%), skull fracture (62.04%), subdural hematoma (19.37%), brain swelling and edema (63.35%), midline shift (24.34%), subarachnoid hematoma (28.79%), epidural hematoma (30.36%) and neurocranium (12.04%) [11]. In Bangladesh, the annual incidence of head injury found was 814.8/1, 00,000 people with mortality rate of 23.39/100,000 population [12]. All types of injuries but basically death and disability mostly occur due to brain injuries [13]. Brain injuries involve contusions, intracranial injuries, skull fracture, bruising, hematomas, brain swelling, edema and hemorrhages [11, 14]. Patients with brain injuries usually involve symptoms of loss of consciousness, short-term memory loss, amnesia, behaviour change, irritability, vomiting and headache all after traumatic injuries but the post injuries include traffic accidents, slipping down, fall down injuries etc. [15-17]. CT scan examination may be important in some cases however in most cases it is challenging to achieve as for the troubles with radioactivity contact and bulk motions. In addition, if no intracranial abnormality is detected immediately after injury, irregular findings might seem several hours later [18].
2. Materials and Methods:
It is a retrospective cross-sectional study, a total of 147 patients had head injuries who were admitted to the the Department of Radiology and Imaging from January 2021 to December 2021 in Bangabandhu Sheikh Mujib Medical College (BSMMC), Faridpur, Bangladesh. Patients included in this study were those who met the inclusion criteria. Data was collected from emergency departments with consent.
2.1 Inclusion criteria
- Patient with traumatic brain injury
- RTA and history of fall with a scale of 13-15 GCS with symptoms of dizziness
- GCS with symptoms of nausea
- GCS with symptoms of headache
- Patients who had vomiting and altered state of consciousness
2.2 Exclusion criteria
All data were presented in a suitable table or graph according to their affinity. A description of each table and graph was given to understand them clearly. Collected information is compiled, analyzed, and edited using the software SPSS (version 24.0) (IBM) Chicago, Illinois.
3. Results
A total of 147 patients were enrolled and analyzed in this retrospective cross-sectional study. In this study, most of the 55(37.41%) patients were from the age group 1-14 years and only 12(8.16%) patients were aged above 65 years (Table 1). Table 2 shows the distribution of the study, 105(71.43%) patients were male and 42(28.57%) patients were female. According to the CT scan finding, 82% of patients had a scalp hematoma, 65(44.22%) patients had normal pain, almost 30% of patients had skull fractures and only 4% of patients had inflammatory changes (Table 3). Table 4 shows the cause of injuries, 94(63.95%) patients fell from height and 53(36.05%) patients had an accidental case. Figures 1 (H/O RTA), 2 (Vomiting), 3 (Headache) & 4 (FITS) show the patient’s CT-scan images.
Age range (Years)
Frequency
Percentage
Jan-14
55
37.41
15-30
38
25.85
31-50
18
12.24
51-65
24
16.33
Above 65
12
8.16
Total
147
100
Table 1: Age distribution of the study population.
Gender
Frequency
Percentage
Male
105
71.43
Female
42
28.57
Total
147
100.00
Table 2: Gender distribution of the study population.
Findings
Frequency
Percentage
Extra Dural hematoma
7
4.76
Non-hemorrhagic contusion
6
4.08
Hemorrhagic contusion
18
12.24
Scalp hematoma
121
82.31
Subarachnoid hemorrhage
12
8.16
Age-related cerebral atrophy
25
17.01
Subdural Hematoma
20
13.61
Inflammatory changes
6
4.08
Normal plain CT examination of the brain
65
44.22
Skull fracture
44
29.93
Table 3: Findings seen in CT scan.
Cause of injury
Frequency
Percentage
Fall from height
94
63.95
Road traffic accident
53
36.05
Total
147
100.00
Table 4: Cause of injuries.
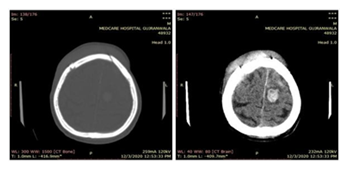
Figure 1: Male patient’s CT Brain (75 Years), H/O RTA (Google source)
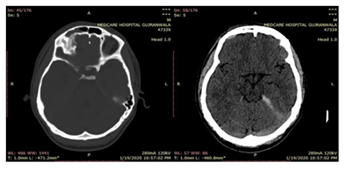
Figure 2: Male patient’s H/O RTA (20 Year), Vomiting (Google source)
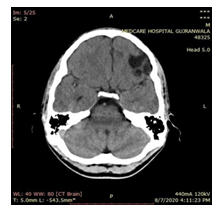
Figure 3: Male patient’s H/O Fall, (15 Year) Unbalance, Headache (Google source)
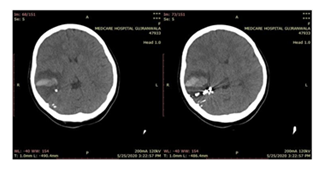
Figure 4: Male patient’s H/O Fall (15 Year), FITS (Google source)
4. Discussion
In our consequences, it is reliable throughout prior studies that showed head injury is common in RTA the majority dynamic time of years. A study reported that head injury during RTA was seen in 63% [19]. Whereas in another study it was reported that 59-69% of head injuries happen in adolescents [20]. Another research, it accomplished that behind head injury to affect results age is the solitary reason. The result was not as good as through the rising generation. In a recent study, the result shows that about 71.5% of injuries occur in males compared to females, which were about 28.5%, and mostly the incidence is present from age 1-14 years about 37%. From a Bangladeshi study, there are three leading causes found were transport injury 30.6% followed by falls 26.2% and violence 14.9% [12]. In our study, we found 53(36.05%) road accident injuries which is near to the previous study. CT-scan had become the one to find the changes that occur in the brain after trauma. Our research reports that most trauma occurs in men compared to women. It is concluded that extradural hematoma was about 4.5%, non-hemorrhagic contusion was 4%, age-related cerebral atrophy at 17%, inflammatory changes were seen at about 4%, and fracture in the skull was seen at about 30%. It was initially stated that head trauma sufferers were mostly men as compared to females because they have more outside exposures on roads and other activities that are outdoors compared to females seen in Bangladesh. In another research, the men were largely occupied with head injuries (86%) [19]. One study found that epidural hematomas were associated with skull fractures in approximately 91% of patients [21].
Limitations of the study:
The study was conducted in a single hospital with small sample size. So, the results may not represent the whole community
5. Conclusion and Recommendations
According to our research, the prevalence of percentage of non-hemorrhage contusions and extradural hematoma have almost an equivalent frequency. Males have a higher rate of intracranial hemorrhage than females. Patients who have been in road traffic accidents \have a higher risk of developing a scalp hematoma than those who have had other types of traumatic injuries. GCS reliability is insufficient since computed tomography is needed for diagnosis and confirmation of the patient's condition. According to our results, it is suggested that patients who have suffered a brain injury must undergo an acute non-contrast computed tomography to determine the best course of treatment. It is very helpful in unconscious patients who have allergies to contrast media. In order to determine the mode of injury, the patient's history should be thoroughly examined. A follow-up scan should be performed within 24-48 hours of the incident to identify the effects of bleeding. The GCS ranking system isn't enough for accident classification. For such patients, a CT scan is prescribed as the first line of examination
Funding:
No funding sources
Conflict of interest:
None declared.
References
-
- Patients who died before the stage of Computed tomography
- Arriving at the hospital 24 hours after injury and drinking alcohol.
- Hyder AA, Wunderlich CA, Puvanachandra P, et al. The impact of traumatic brain injuries: a global perspective. NeuroRehabilitation 22(2007): 341-353.
- Murray CJ, Lopez AD, World Health Organization. The global burden of disease: a comprehensive assessment of mortality and disability from diseases, injuries, and risk factors in 1990 and projected to 2020: summary. World Health Organization 1 (1996).
- Onwuchekwa CR, Alazigha, NS. Computed tomography pattern of traumatic head injury in Niger Delta, Nigeria: A multicenter evaluation. International journal of critical illness and injury science 7 (2017): 150.
- Paci M, Infante-Rivard C, Marcoux J. Traumatic brain injury in the workplace. Canadian journal of neurological sciences 44 (2017): 518-524.
- Hans P, Mehrotra A, Kumar P, et al. Role of Computerized Tomography as Prime Imaging Modality in the Evaluation of Traumatic Brain Injury. Int J AdvInteg Med Sci 2 (2017): 17-23.
- Hassan N, Ali M, Haq N, et al. Etiology, clinical presentation and outcome of traumatic brain injury patients presenting to a teaching hospital of Khyber Pakhtunkhwa. Journal of Postgraduate Medical Institute (Peshawar- Pakistan) 31 (2017).
- AHMAD I, RAZA MH, ABDULLAH A, et al. Intracranial CT scan Findings in the Patients of Head Injury: An Early Experience at Dera Ghazi Khan Teaching Hospital. Pakistan Journal of Neurological Surgery 24 (2020): 248-252.
- Khan M, Yaqoob U, Hassan Z, et al. Immediate Outcomes of Traumatic Brain Injury at a Tertiary Care Hospital of Pakistan-A Retrospective Study 10 (2020)
- Naheed K, Pal MI, Naeem M, et al. ANALYSIS OF DEATHS DUE TO ROAD TRAFFIC ACCIDENTS IN FAISALABAD CITY-PAKISTAN. Journal of University Medical & Dental College 10 (2019): 38-43.
- Mehta RA, Bambhaniya AB. Profile of Fatal Head Injuries in and Around Jamnagar Region. Indian Journal of Forensic Medicine and Pathology 11 (2018): 187.
- Gupta PK, Krishna A, Dwivedi AN, et al.. CT scan findings and outcomes of head injury patients: A cross sectional study. Journal of Pioneering Medical Sciences 1 (2011): 78.
- Hossain MJ, Ferdoush J, Shawon RA, et al. PW 2842 Epidemiology of traumatic head injury-nationally conducted survey findings from bangladesh. Injury Prevention 24 (2018): A195.
- El Hendawy MM, Mohammed MS, Saad AH. Surgical Management of Open Traumatic Head Injury. The Egyptian Journal of Hospital Medicine 78 (2020): 42-47.
- Ibrahim SY. Study of Traumatic Head Injuries Using Computerized Tomography Among Sudanese. International J of Biomedicine 11(2021).
- Kong MH, Jang SY, Kim JH, et al. The usefulness of brain magnetic resonance imaging with mild head injury and the negative findings of brain computed tomography. Journal of Korean Neurosurgical Society 54 (2013): 100-106.
- Polinder S, Cnossen MC, Real RG, et al. A multidimensional approach to post-concussion symptoms in mild traumatic brain injury. Frontiers in neurology 9 (2018): 1113.
- Cnossen MC, van der Naalt J, Spikman JM, et al. Prediction of persistent post-concussion symptoms after mild traumatic brain injury. Journal of neurotrauma 35 (2018): 2691-2698.
- Shiomi N, Echigo T, Hino A, et al. Criteria for CT and initial management of head injured infants: a review. Neurologia medico-chirurgica 56 (2016): 442-448
- Bharti P, Nagar AM, Umesh T. Pattern of trauma in western Uttar Pradesh. Neurology India 41(1993): 49-50.
- Reverdin A. Head injury in children. NIMS: Head injury, clinical management and research. Elizabeth Frost (ed), Geneva, Switzerland: Airsen 10 (1990):193-204.
- Phonprasert CH, Suwanwela CH, Hongsaprabhas CH, et al. Extradural hematoma: analysis of 138 cases. The Journal of trauma 20 (1980):679-683.
-
