Simplicity Denervation System for Pulmonary Artery Denervation in Patients with Residual Pulmonary Hypertension after Pulmonary Thromboembolism and Surgical Thrombectomy
Article Information
B. Rudenko1*, A. Shanoyan1, O. Drapkina1, N. Gavrilova1, S. Beregovskaya1, A. Akhadova1, D. Feshchenko1, F. Shukurov1, V. Vlasov1, S. Boytsov2, S. Dzemeshkevich3, Yu. Frolova3, A. Edemsky4
1National Center For Preventive Medicine, Moscow, Russia
2Russian Cardiology Scientific and Production Complex, Moscow, Russia
3Russian National Center of Surgery, Moscow, Russia
4Research Institute of Circulation Pathology, Novosibirsk, Russia
*Corresponding Author: Boris Rudenko, National Center For Preventive Medicine, Moscow, Russia
Received: 22 August 2017; Accepted: 05 September 2017; Published: 07 September 2017
View / Download Pdf Share at FacebookAbstract
Purpose: To study the safety and effectiveness of simplicity denervation system in lowering pulmonary artery pressure in patients with pulmonary hypertension after pulmonary thromboembolism and surgical thrombectomy.
Methods: We analyzed the 3-months results of 12 procedures of pulmonary artery denervation with the simplicity denervation system. The primary endpoints were the change of pulmonary artery pressure and 6 minutes walking test at 3 months follow-up.
Results: The procedure of pulmonary artery denervation was performed at the ostium of the right and left pulmonary arteries using the electrode from Simplicity denervation system. Using the coronary guiding technique, the tip of electrode was placed at the ostium of the pulmonary artery, then the radio frequency energy was applied (temperature >50°C, energy = 12 W, and time = 120), rotating the tip with pace of 2 mm at the ostium of each pulmonary artery. The proper position of the electrode (tight contact with the vessel wall) was checked automatically by resistance monitoring and manual tracking. At 3 months follow-up the pulmonary artery pressure decreased from 58 ± 6 to 33 ± 4 mm Hg (p < 0.01) and improvement of the 6 minutes walking test from 321 ± 19 m to 487 ± 29 m (p < 0.01) was observed.
Conclusion: The simplicity denervation system is proven to be safe and effective for pulmonary artery denervation. Further randomized study is needed to confirm the clinical benefit of this procedure in patients with pulmonary hypertension.
Keywords
Pulmonary Hypertensions; Pulmonary Artery Denervation; Pulmonary Thromboembolism; Symplicity Denervation System
Article Details
1. Introduction
Pulmonary embolism and obstruction of the major pulmonary arteries is associated with significant mortality and poor long-term prognosis [1]. One of the negative consequences of the acute and chronic thromboembolism is a development of pulmonary hypertension. For many patients pulmonary thrombectomy surgery is a life-saving operation, but often it doesn’t prevent the progression of the pulmonary hypertension in the long-term. Persistent chronic pulmonary hypertension may cause the development of heart failure and trigger the formation of the new clots.
In 1980 Juratsch et al. [2] first demonstrated effectiveness of surgical pulmonary denervation and chemical sympathectomy in decreasing abnormally elevated pulmonary vascular resistance (PVR) and mean pulmonary artery pressure (mPAP) caused by distension of the pulmonary artery (PA). Animal-based experiments [2, 3] and the development of renal denervation as a treatment for drug-resistant hypertension [4, 5] prompted the use of radiofrequency denervation for reducing the pressure in the vessels of the pulmonary circulation as well.
Intensive study of this technique in clinical trials began in 2012. Studies were carried out not only on animal models of pulmonary arterial hypertension (PAH) [6, 7], but also in the treatment of idiopathic pulmonary hypertension (IPAH) in humans [8]. In the first-in-man study authors used the radiofrequency system with special dedicated circular-tip catheter [8].
The goal of our study was to evaluate the safety and effectiveness of well-known Simplicity denervation system in lowering pulmonary artery pressure in patients with residual pulmonary hypertension after surgical treatment of pulmonary embolism.
2. Methods
Patients with the history of surgical treatment (thrombectomy) of acute pulmonary embolism and residual pulmonary hypertension (defined as mean pulmonary artery pressure > 25) were eligible for the study. A total of 12 patients were included. Before the procedure all 12 patients received diuretics (hydrochlorothiazide at a dose 25 mg per day) Ca+ channel blocker (amlodipine at a dose of 5 mg to 10 mg per day), sildenafil (20 mg, 3 times a day) or digoxin (0.125 mg per day). Written consent was obtained from all patients. Functional capacity was determined by the 6MWT. The 6MWT, Echocardiographic study and right heart catheterization were performed before and 12 months following the PADN procedure. Echocardiographic studies were done using a GE VIVID 7 system (General Electric Co) and all measurements were performed according to the recommendations of the American Society of Echocardiography [9]. The right heart catheterization was performed through the femoral or jugular vein depending on the presence or absence of the cava filter.
2.1 Pulmonary Artery Denervation Procedure
The pulmonary artery catheterization procedure was performed through 6-Fr sheath, installed into the right femoral or the right jugular vein. First the pig-tail catheter was inserted into the RA, RV and PA consequently. Hemodynamic measurements and blood oxygen saturation data from the RA, RV, and PA were done before the PADN procedure. The PVR [PVR = (mean PAP ? PAOP) /CO] was calculated. These measurements were also done 12 months after the procedure.
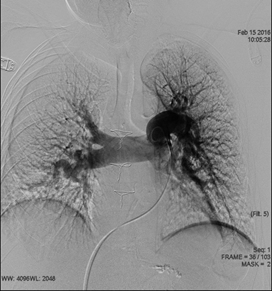
A baseline PA angiography was performed to identify the PA bifurcation level and evaluate the PA diameter (Figure 1).
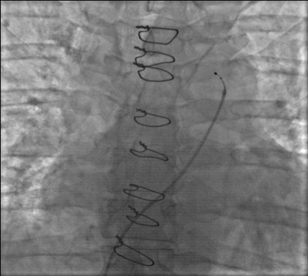
Then the pig-tail catheter was exchanged for coronary guiding catheter (JR 4, 6 Fr), which was placed at the ostium of the left PA, <2 mm distal to orifice. Then Simplicity 6 Fr-compatible radiofrequency ablation catheter was inserted through the guiding catheter to the ostium of the left PA (Figure 2).
After withdrawing slightly the guiding catheter and pushing forward the Simplicity catheter, the steerable tip would be released from the guiding catheter (Figure 3).
Then, by pulling the steering handle, the angulation at the tip would be made for the proper contact with the vessel wall (Figure 4,5).
To ensure that the electrode was tightly in contact with the endovascular surface, generator Symplicity had a contiuous monitoring system, switching automatically in case of sudden drop of impedance or rise of temperature. After ablation at this spot, the tip of the catheter would be straightened up by pushing the handle. Slightly rotating the handle in the clockwise or counterclockwise direction, the tip would be placed 1-2 mm from initial spot, angulation would be made and the next ablation performed. Altogether, the 7 to 10 ablation spots would be made, rotating the tip of the catheter around the vessel’s ostium. The same procedure would be performed at the ostium of the right PA.
The following ablation parameters were applied at each spot: temperature >50°C, energy = 10 W, and time = 120 s. The electrocardiogram and hemodynamic pressure were monitored and continuously recorded throughout the procedure. Procedural success was defined as a reduction in the mean PAP >10 mm Hg (as measured by guiding catheter at the end of ablation), and there were no complications. The patients were monitored in the cardiac care unit for at least 12 h after the PADN procedure.
2.2 Endpoints
The primary endpoints were: changes in the functional capacity (measured by the 6MWT), changes in systolic pulmonary pressure (measured by Ecocardiography) and mean PAP, PVR (calculated during right heart catheterization) at 12 months. The secondary endpoints were clinical adverse events (all-cause death, PA perforation, acute thrombus formation in the PA or in veins and bleeding).
2.3 Statistical analysis
Continuous variables are expressed as mean ± SD. Differences in continuous variables were analyzed using paired-sample Student t tests. The categorical variables were compared using the Fisher exact test. Statistical significance was defined as p value < 0.05. All analyses were performed using the statistica program SPSS version 20.0 for Windows (SPSS Institute, Chicago, Illinois).
3. Results
A total of 12 patients with residual pulmonary hypertension and clinical symptoms of chronic heart failure were included between March 2015 and October 2015 (Table 1). All patients presented with dyspnea, fatigue, peripheral edema. The average time interval between the thrombectomy operation to pulmonary denervation was 8.5 years.
|
|
PADN group (n=12) |
|
Age, yr |
42 ± 13 |
|
Male, n(%) |
6 (50) |
|
Time from diagnosis from surgical trombectomy to PADN, yr |
8,5 ± 2.4 |
|
Presentation, n (%) |
1 (8.3) |
|
Medication, n (%) |
12 (100) |
|
Functional class, n (%) |
1 (8.3) |
|
Systolic pulmonary artery pressure |
|
|
Mean pulmonary artery pressure |
58 ± 6 |
|
Pulmonary vessel resistance |
|
|
6 minutes walking test |
321 ± 19 |
Table 1: Baseline clinical characteristics of all patients
During and immediately following the PADN procedure, no complications (death, arrhythmias, PA perforation, acute thrombus formation in the PA or at the access site, bleeding) were recorded. All patients were monitored in the intensive care unit at least 12 hours and released from hospital after 2 days.
During 12-months of follow-up one patient died for non-cardiac reason (severe gastric bleeding). The rest of the patients reported no deterioration of the symptoms and no complications were registered. No rehospitalization was required. 9 patients noticed s
|
|
Before the PADN |
12 months follow-up |
P |
|
Systolic pulmonary artery pressure, mm Hg |
64,7±21,4 |
48,4±20,2 |
p < 0.01 |
|
Mean pulmonary artery pressure, mm Hg |
58 ± 6 |
33 ± 4 |
p < 0.01 |
|
PVR, Wood units |
8,6±2,1 |
3,2 ± 1,4 |
p < 0.01 |
|
6 MWT, m |
321 ± 19 |
487 ± 29 |
p < 0.01 |
After 12 months all patients underwent right heart catheterization, echocardiographic and functional capacity measurements. At 12 months follow-up the reduction of mean pulmonary artery pressure was reported (from 58 ± 6 to 33 ± 4 mm Hg) (p < 0.01) and improvement of the 6 minutes walking test from 321 ± 19 m to 487 ± 29 m (p < 0.01) was observed (Table 2).
Table 2: Results at 12 months follow-up
4. Discussion
In spite of successful surgical treatment patients after acute pulmonary embolism often develop pulmonary arterial hypertension. The pathogenesis of pulmonary artery pressure (PAP) elevation and pulmonary vascular resistance (PVR) is believed to be due to small branch emboli’s that cannot be removed mechanically. Patients with residual pulmonary arterial hypertension have a poor long-term prognosis because of unsatisfactory clinical response to medication and rapid deterioration of cardiac function.
The small branch embolism might trigger the mechanism of pulmonary arterial hypertension by enhancing activity of the sympathetic nerve fibers localized in or near the bifurcation area of the main pulmonary artery.
Several recent studies have demonstrated that local destruction of these nerve fibers might significantly modulate the sympathetic activity and lead to reduction of PAP and PVR. Study of this technique in clinical trials began in 2012. Studies were carried out not only on animal models of pulmonary arterial hypertension (PAH) [6, 7], but also in the treatment of idiopathic pulmonary hypertension (IPAH) in humans [8].
One of the first experimental study investigated the hemodynamic response of the occlusion of left interlobar pulmonary artery in animals before and after pulmonary artery denervation [6]. The balloon-induced occlusion increased PAP and PVR to the peak values after 5 min, and this pressure response was completely abolished after PADN at the MPA bifurcation level.
In 2013 Chen et al. published results of the first phase PADN-1 study [8]. The purpose of the study was to evaluate effectiveness and safety of radiofrequency pulmonary artery denervation in patients with idiopathic pulmonary hypertension. In this study were included only patients with IPAH refractory to medical therapies. Out of a total of 21 patients, 13 patients received the pulmonary artery denervation (PADN) procedure; the other 8 patients who refused the PADN procedure were assigned to the control group.
The primary end points were the change of hemodynamic (mPAP) and clinical parameters (functional capacity by the 6-minute walk test 6MWT). Procedures were performed by special designed 7.5F multiple-function (temperature-sensor and ablation) catheter with circular tip and 10 pre-mounted electrodes. PADN was performed at the three points of PA (bifurcation, ostial right and left PA).
Authors reported at 3 month follow-up according echocardiography significant reduction of mean PAP (from 55±5 mmHg to 36±5 mmHg, p<0.01) and significant improvement of the 6MWT (from 324±21 m to 491±38 m, p<0.006) in the group who underwent the PADN procedure. There were no procedural complications during study.
Second phase of PADN-1 study lasted for 2 years (2012-2014) and 66 patients were prospectively followed up [10]. The main objective of second phase was to demonstrate the long-term efficacy and safety of the new method. The findings correlated with the results of first phase. The new method proved its safety.
During the study investigators found that the main decrease in hemodynamic parameters were observed during the first 6 months with the next stabilization of result in the following 6 months. This may indirectly indicate a positive effect of denervation on vascular remodeling.
The Symplicity system has been used for the treatment of resistant arterial hypertension for many years. It consists of radiofrequency generator and steerable 6-Fr compatible catheter. Generator Symplicity is equipped with continually monitoring system, switching automatically in case of sudden drop of impedance or rise of temperature. This is one of system advantage, which minimizes the risk of artery perforation. No such complication has been reported so far.
Several studies including randomized ones have demonstrated the clinical effectiveness of renal denervation [4,11, 12). Many of them reported the significant lowering arterial blood pressure, resulting in reducing or discontinuation multicomponent drug therapy. Although the clinical effectiveness of renal denervation in the Simplicity III trial remains controversial, this study proved the clinical safety of the procedure [5]. The complication rate did not differ between the main group and the control group with the imitation of the denervation (sham-procedure).
The postulated that the similar anatomical characteristics (the diameter of the artery, the thickness at the arterial wall) are suitable for the use of Simplicity denervation system in the pulmonary vessels. The steering tip of the simplicity catheter allows creating sharp angle sufficient for the proper contact with vessel wall. Rotating handle of the catheter provides the opportunity of applying radiofrequency energy in the circular way with the pace of 2 mm. The performed the radiofrequency ablation at the ostium of each pulmonary artery (right and left, approximately 1-2 mm distally to the orifice) with average spot number from 7 to 10 to each ostium.
The results of the pulmonary denervation with dedicated circular tip catheter and our study with Simplicity denervation system have demonstrated that this procedure might be good alternative to drug treatment in patients with residual pulmonary hypertension. Different medications have been developed in recent times for the treatment of pulmonary hypertension [1, 13]. Although there have been several reports of functional capacity improvement in patients receiving medical treatment, the long-term effects of many medications remain unclear. Also potential limitations to long-term drug therapy are the high cost and severe side effects.
5. Conclusion
The Simplicity denervation system is proven to be safe and effective for pulmonary artery denervation. Further randomized study is needed to confirm the clinical benefit of this procedures in patients with pulmonary hypertension.
References
- Galiè N, Hoeper M, Humbert M, Torbicki A, Vachiery JL, et al. ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension: The Joint Task Force for the Diagnosis and Treatment of Pulmonary Hypertension of the European Society of Cardiology and of the European Respiratory Society. Eur Heart J 37 (2016): 67-119.
- Juratsch CE, Jengo JA, Castagna J, Laks MM. Experimental pulmonary hypertension produced by surgical and chemical denervation of the pulmonary vasculature. Chest 77 (1980): 525?530.
- Laks MM, Juratsch CE, Garner D, Beazell J, Criley JM. Acute pulmonary artery hypertension produced by distention of the main pulmonary artery in the conscious dog. Chest 68 (1975): 807?813.
- Esler MD, Krum H, Sobotka PA, Schlaich MP, Schmieder RE, et al. Renal sympathetic denervation in patients with JACC 63 (2014): 611-618.
- Bhatt DL, Kandzari DE, O’Neill WW, D’Agostino R, Flack JM, et al. A controlled trial of renal denervation for resistant hypertension. N Engl J Med 370 (2014): 1393-1401.
- Chen SL, Zhang YJ, Zhou L, et al. Percutaneous pulmonary artery denervation completely abolishes experimental pulmonary arterial hypertension in vivo. EuroIntervention 22 (2013): 269?276.
- Zhou L, Zhang J, Jiang X-M, et al. Pulmonary artery denervation attenuates pulmonary arterial remodeling in dogs with pulmonary arterial hypertension induced by dehydrogenized monocrotaline. J Am Coll Cardiol Intv 8 (2015): 2013?2023.
- Chen SL, Zhang FF, Xu J, et al. Pulmonary artery denervation to treat pulmonary arterial hypertension: a single-center, prospective, first-in- man PADN-1 study (first-in-man pulmonary artery denervation for treatment of pulmonary artery hypertension). J Am Coll Cardiol 62 (2013): 1092?1100.
- Lang RM, Bierig M, Deverus RB, et al. Recommendations for chamber quantification: a report from the American Society of Echocardiography's Guidelines and Standards Committee and the Chamber Quantification Writting Group. J Am Soc Echocardiogr 18 (2005): 1440-1463.
- Chen SL, Zhang H, Xie DJ, Zhang J, Zhou L, et al. Hemodynamic, functional, and clinical responses to pulmonary artery denervation in patients with pulmonary arterial hypertension of different causes: phase II results from the Pulmonary Artery Denervation-1 Study. Circ Cardiovasc Interv 8 (2015): e002837.
- S HTN, Investigators. Catheter-based renal sympathetic denervation for resistant hypertension: durability of blood pressure reduction out to 24 months. Hypertension 57 (2011): 911?917.
- Schlaich MP, Hering D, Sobotka P, Krum H, Lambert GW, et al. Effects of renal denervation on sympathetic activation, blood pressure, and glucose metabolism in patients with resistant hypertension. Front Physiol 3 (2012): 10.
- Galiè N, Palazzini M, Leci e, Manes A. Current Therapeutic Approaches to Pulmonary Arterial Hypertension. Rev Esp Cardiol 63 (2010): 708-724.