Short-Term Outcome of Hemorrhagic Stroke Patients Admitted to Medicine Ward in Dhaka Medical College Hospital
Article Information
Dr. Farzana Sultana1, Dr. Fazle Rabbi2, Dr. Amran Ahmed3, Dr. Molla Md. Rubaiat4, Dr. Aziza sultana5, Dr. Farhana sultana6, Dr. Atikur Rahman7, Dr. Bishnu Pada Saha8
1Senior Consultant, Department of Cardiology, National Institute of Cardiovascular Diseases & Hospital, Dhaka, Bangladesh
2Senior Medical Officer, ICU, Bangladesh Medical College & Hospital, Dhaka, Bangladesh.
3Consultant, Cardiac Surgeon, Labaid Cardiac Hospital, Dhaka, Bangladesh.
4Associate Professor, Department of Anaesthesiology, Armed Forces Medical College, Dhaka, Bangladesh.
5Lecturer, Department of Anatomy, Holy Family Red Crescent Medical College, Dhaka, Bangladesh.
6Medical officer, lecturer, Community Medicine, Shaheed Suhrawardy Medical College, Dhaka, Bangladesh.
7Assistant Registrar, Department of Cardiology, National Institute of Cardiovascular Diseases & Hospital, Dhaka, Bangladesh.
8Chief Consultant, Department of Cardiology, Shaheed Sheikh Abu Naser Specialized Hospital, Khulna, Bangladesh
*Corresponding author: Dr. Farzana Sultana, Senior Consultant, Department of Cardiology, National Institute of Cardiovascular Diseases & Hospital, Dhaka, Bangladesh.
Received: 08 August 2024; Accepted: 29 August 2024; Published: 23 September 2024
Citation: Farzana Sultana, Fazle Rabbi, Amran Ahmed, Molla Md. Rubaiat, Aziza sultana, Farhana sultana, Atikur Rahman, Bishnu Pada Saha. Short- Term Outcome of Hemorrhagic Stroke Patients Admitted to Medicine Ward in Dhaka Medical College Hospital. Cardiology and Cardiovascular Medicine. 8 (2024): 415-419.
View / Download Pdf Share at FacebookAbstract
Cardiovascular diseases are the leading cause of mortality worldwide, with a disproportionately high burden in low- and middle-income countries. Biomarkers play a crucial role in the early detection, diagnosis, and treatment of cardiovascular diseases by providing valuable insights into the normal and abnormal conditions of the heart and vascular system. The biomarkers derived from the cells and tissues can be identified and quantified in the blood and other body fluids and in tissues. Changes in their expression level under a pathological condition provide clinical information on the underlying pathophysiology that could have predictive, diagnostic, and prognostic value in the treatment of a disease process, and therefore incorporated in clinical guidelines. This enhances the effectiveness of biomarkers in risk stratification and therapeutic decisions in personalized medicine and improvement in patient outcomes. Biomarkers could be protein, carbohydrate, or genome-based and may also be derived from lipids and nucleic acids. Computational biology has emerged as a powerful discipline in biomarker discovery, leveraging computational techniques to identify and validate biological markers for disease diagnosis, prognosis, and drug response prediction. The convergence of advanced technologies, such as artificial intelligence, multi-omics profiling, liquid biopsies, and imaging, has led to a significant shift in the discovery and development of biomarkers, enabling the integration of data from multiple biological scales and providing a more comprehensive understanding of the complex signaling and transcriptional networks underlying disease pathogenesis. In this article, we reviewed the role of computational biology integrated with genomics, proteomics, and metabolomics, together with machine learning techniques and predictive modeling and data integration in the discovery of biomarkers in cardiovascular diseases. We discussed specific biomarkers, including epigenetic, metabolic, and emerging biomarkers, such as extracellular vesicles, miRNAs, and circular RNAs, and their role in the pathophysiology of the heart and vascular diseases.
Keywords
Short-term outcome; Hemorrhagic stroke; Intracerebral hemorrhage; Cerebral vascular diseases
Article Details
1. Introduction
The human nervous system stands as the most intricate, extensively studied, yet incompletely understood physiological system known to humanity. Its structure and functions intricately intertwine with every facet of life—physical, cultural, and intellectual [1]. Cerebrovascular diseases represent the leading cause of disability in industrialized nations, imposing a significant social burden. The evolving incidence of stroke over recent decades is a matter of profound concern due to its substantial public health implications [2]. Current epidemiological insights underscore stroke as a prominent contributor to mortality and morbidity worldwide, affecting populations across both developed and developing nations [3]. According to World Health Organization (WHO) criteria, stroke is characterized by the rapid onset of focal or global cerebral function disturbances lasting more than 24 hours, with no apparent non-vascular origin. Stroke occurrences are further categorized as either first-ever, marking their initial incidence in a patient’s lifetime, or recurrent. Subtypes of stroke are delineated based on findings from computed tomography (CT) or magnetic resonance imaging (MRI) studies. Among patients experiencing first-ever strokes, classifications include cerebral infarction (CI), intra-cerebral hemorrhage (ICH), subarachnoid hemorrhage, and unclassifiable stroke. Unclassifiable stroke denotes events lacking sufficient information to conclusively meet WHO criteria for definite stroke, often occurring without neuroimaging confirmation [2]. Post-stroke outcomes are influenced by numerous factors including subtype, stroke severity, underlying predisposing factors, associated complications, access to specialized care, and availability of stroke care facilities [4]. Stroke ranks as the third leading cause of mortality in industrialized countries, following cardiovascular disease and cancer. Incidence rates vary across European nations, typically ranging from 100 to 200 new cases per 100,000 inhabitants annually [5]. In the United Kingdom, data from the Oxfordshire Community Stroke Project indicates a first stroke incidence rate of 1.6 per 1,000 person-years at risk, with risk escalating notably with advancing age [6,7]. East Asian countries such as Japan, China, and Taiwan exhibit higher stroke mortality rates exceeding 100 per 100,000, compared to rates of 50-80 per 100,000 in New Zealand and Australia. Conversely, Southeast Asian countries like Thailand, Malaysia, Indonesia, and the Philippines report lower stroke mortality rates below 20 per 100,000 [8]. The objective of this study was to assess the short-term outcome of hemorrhagic stroke patients.
2. Methodology
This was a prospective observational study that was conducted in the Medicine In-patients Department of Dhaka Medical College Hospital, Dhaka, Bangladesh from October 2009 to March 2010. A total of 60 cases of hemorrhagic stroke were selected as study subjects using purposive sampling. The research protocol received ethical approval from the Bangladesh College of Physician and Surgeons, Dhaka, prior to commencement. Written consent was obtained from all participants before initiating data collection. According to the inclusion criteria, this study enrolled patients aged 18 years or older who provided consent and agreed to participate, exhibited clinical features of stroke confirmed by computed tomography scan indicating hemorrhagic stroke, and experienced their first hemorrhagic stroke event. Exclusion criteria included patients who declined participation, those with intracranial space-occupying lesions presenting with stroke-like symptoms, infectious diseases affecting the brain and meninges, and patients diagnosed with ischemic stroke. Data analysis was performed using MS Office tools.
3. Result
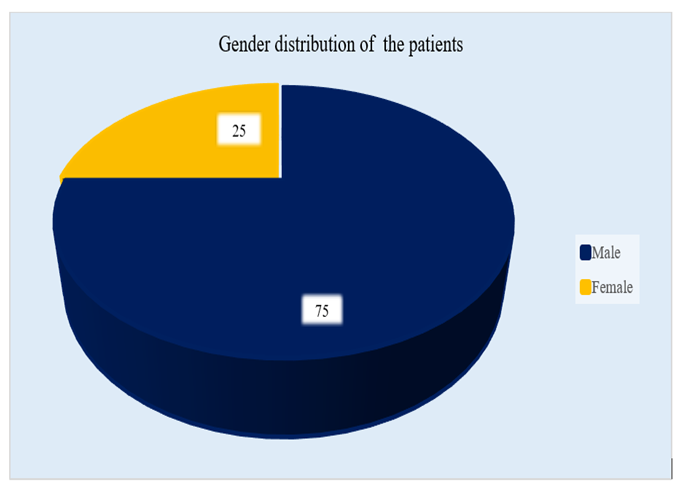
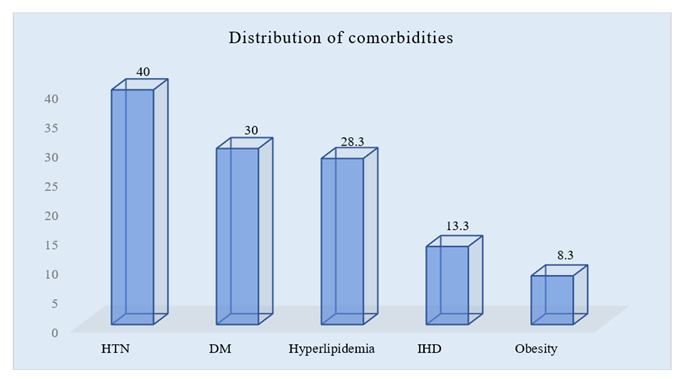
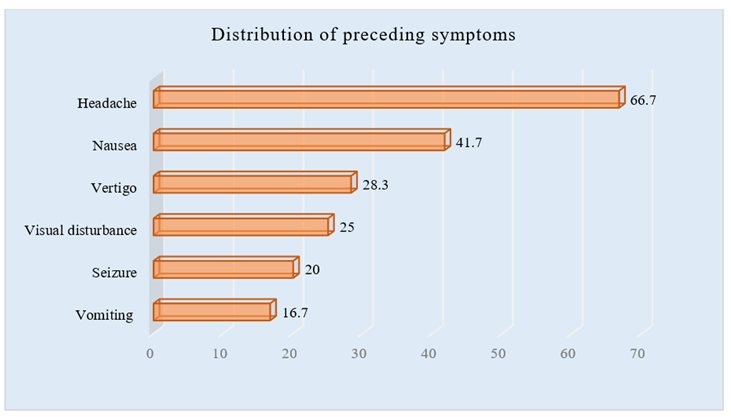
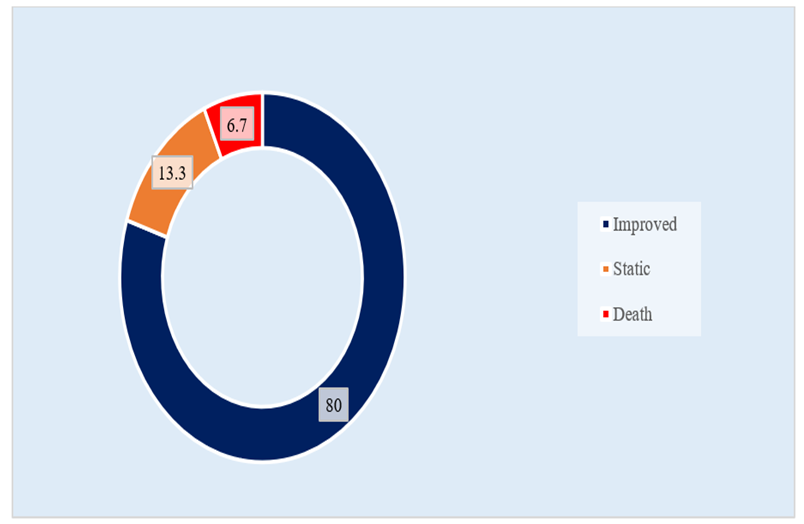
In this study, one-third of the participants were from the age group of 40-50 years. Among the total participants, 45 (75.0%) were male and 15 (25.0%) were female. The onset of illness among patients occurred during sleep (28.3%), work (20.0%), excitement (15.0%), rest (16.7%), eating (8.3%), and other activities (11.7%). The mode of onset was sudden in 58.3% of cases and gradual in 41.7%. At presentation, most patients were conscious (66.7%), followed by drowsy (16.7%), and unconscious (8.3%); an additional 8.3% were unconscious but later recovered. In this study, 40% of participants had hypertension (HTN), 30% had diabetes mellitus (DM), 13.3% had ischemic heart disease (IHD), 28.3% had hyperlipidemia, and 8.3% had obesity as the comorbidities. Headache (66.7%), vertigo (28.3%), nausea (41.7%), vomiting (16.7%), visual disturbance (25.0%), and seizures (20.0%) were noted as preceding symptoms among the participants. Neurological examinations revealed that out of 60 patients, 66.7% were oriented and 33.3% were not. Normal consciousness was found in 66.7% of cases, while 21.7% had Grade I consciousness, 3.3% had Grade II, 5.0% had Grade III, and 3.3% had Grade IV. Speech was normal in 70.0% of cases, with dysarthria and dysphasia in 8.3% and 13.3%, respectively. Memory impairment was present in 10.0% of patients, while 81.7% had no memory issues. Muscle bulk was normal in 91.7% of patients, with only 8.3% showing muscle wasting. Muscle tone was normal in 13.3% of cases, hypertonic in 80.0%, and hypotonic in 6.7%. According to the distribution of CT findings, 51.7% of patients with hemorrhagic stroke had right-sided intracerebral hemorrhage, 40.0% had left-sided intracerebral hemorrhage, 5.0% had pontine hemorrhage, and 3.3% had brain stem hemorrhage. In our study, as the distribution of the outcome of the patients, it was observed that out of 60 patients, the condition of 48 (80.0%) participants were improved, 8 (13.3%) were static and the rest 4 (6.7%) died.
|
Complaints |
n |
% |
|
Onset of illness |
||
|
Sleep |
17 |
0.283 |
|
Work |
12 |
0.2 |
|
Excitement |
9 |
0.15 |
|
Rest |
10 |
0.167 |
|
Eating |
5 |
0.083 |
|
Others |
7 |
0.117 |
|
Mode of onset |
||
|
Sudden |
35 |
0.583 |
|
Gradual |
25 |
0.417 |
|
Level of consciousness |
||
|
Conscious |
40 |
0.667 |
|
Drowsy |
10 |
0.167 |
|
Unconscious |
5 |
0.083 |
|
Unconscious but recovered |
5 |
0.083 |
Table 1: Distribution of presenting complaints (N=60).
|
Findings |
n |
% |
|
Higher psychic function |
||
|
Orientated |
40 |
0.667 |
|
Not orientated |
20 |
0.333 |
|
Level of consciousness |
||
|
Normal |
40 |
0.667 |
|
Grade I |
13 |
0.217 |
|
Grade II |
2 |
0.033 |
|
Grade III |
3 |
0.05 |
|
Grade IV |
2 |
0.033 |
|
Speech |
||
|
Normal |
42 |
0.7 |
|
Dysarthria |
5 |
0.083 |
|
Dysphasia |
8 |
0.133 |
|
Memory impairment |
||
|
Impair |
6 |
0.1 |
|
Not impair |
49 |
0.817 |
|
Motor functions Bulk of the muscle |
||
|
Normal |
55 |
0.917 |
|
Wasted |
5 |
0.083 |
|
Muscle tone |
||
|
Normal |
8 |
0.133 |
|
Hypertonic |
48 |
0.8 |
|
Hypotonic |
4 |
0.067 |
Table 2: Findings of neurological examinations (N=60).
|
CT findings |
n |
% |
|
Right-sided ICH |
31 |
0.517 |
|
Left-sided ICH |
24 |
0.4 |
|
Pontine haemorrhage |
3 |
0.05 |
|
Brain stem haemorrhage |
2 |
0.033 |
|
Total |
60 |
1 |
Table 3: Distribution of CT scan of head findings (N=60).
4. Discussion
One-third of participants fell within the 40-50 age bracket. The mean age was 50.33 ± 8.93 years, with an age range from 30 to 84 years. Hsiang et al. [9] conducted a study involving 60 consecutive Chinese patients, noting a younger age profile compared to Western studies. Ong and Raymond [10] reported a median age of 65 years in their research. Juvela et al. [11] conducted a prospective study to identify independent prognostic factors, including preictal variables, for spontaneous intracerebral hemorrhage outcomes, involving 156 patients aged 16 to 60 years. Adnan et al. [12] highlighted a younger age of onset in men compared to women. It was observed that among our participants, 45 (75.0%) were male and 15 (25.0%) were female. Ong and Raymond [10] conducted a study aimed at identifying major risk factors for stroke and predictors of one-month mortality, including 246 patients (139 male and 107 female) with a male-to-female ratio of 1:0.77. Juvela et al. [11] undertook a prospective follow-up study to determine independent prognostic factors, including preictal variables, for spontaneous intracerebral hemorrhage outcomes. Their study included 156 consecutive patients (96 men and 60 women), resulting in a male-to-female ratio of 1:0.63. Such variations may be influenced by geographic factors. In our study, regarding the distribution of CT findings among patients with hemorrhagic stroke, it was observed that 51.7% had right-sided intracerebral hemorrhage, 40.0% had left-sided intracerebral hemorrhage, 5.0% had pontine hemorrhage, and 3.3% had brain stem hemorrhage. Regarding the outcomes of the patients in our study, out of 60 participants, it was observed that the condition of 48 (80.0%) improved, 8 (13.3%) remained stable, and 4 (6.7%) died. Hemorrhagic stroke is associated with more severe morbidity and higher mortality rates compared to ischemic stroke. Only 20% of patients regain functional independence, and the 30-day mortality rate for hemorrhagic stroke ranges from 40% to 80%. Approximately half of all deaths occur within the first 48 hours. Primary intracerebral hemorrhage (PICH) is particularly linked to higher mortality and increased disability among survivors. In the present study of 60 patients, 80.0% showed improvement, 13.3% remained static, and 6.7% died. Ong and Raymond [10] studied predictors of one-month mortality and reported a mortality rate of 20.3% at one month. A recent investigation conducted by Zia et al. [13] involving 474 intracerebral hemorrhage (ICH) patients revealed that male gender was predictive of poorer outcomes among those under 75 years of age. Within 28 days, mortality rates were 20.0% for women and 23.0% for men (P=0.38). For patients aged 75 years or older, mortality rates were 26.0% for women and 41.0% for men (P=0.02). Yonghong et al. [14] explored the relationship between admission blood pressure and in-hospital mortality or disability in acute stroke patients in Inner Mongolia, China. The study included 2178 acute ischemic stroke and 1760 hemorrhagic stroke patients confirmed by computed tomography or magnetic resonance imaging.
5. Limitation of the Study
The current study was conducted over a short period due to time constraints. The study population was recruited from a single hospital in Dhaka city, which may limit the generalizability of the findings to the broader population. Additionally, a small sample size was another limitation of the study.
6. Conclusion and Recommendation
Right-sided intracerebral hemorrhage is more prevalent among patients experiencing hemorrhagic stroke. Despite advancements in medical science, approximately one-fifth of hemorrhagic stroke patients in Bangladesh continue to face persistent morbidity or mortality. This underscores the ongoing challenges in managing and treating hemorrhagic stroke effectively, highlighting the need for enhanced strategies in acute care, rehabilitation, and long-term management to improve outcomes for affected individuals. Continued efforts in public health initiatives and healthcare infrastructure development are crucial to addressing these issues and reducing the burden of hemorrhagic stroke in Bangladesh.
References
- Williams PL, Bannister LH, Berry MM, et al. Gray’s anatomy: The anatomical basis of medicine and surgery. 38th Edition, Churchill Livingstone, New York (1995).
- Intisoa D, Stampatorea P, Zarrellia MM, et al. Incidence of first-ever ischemic and hemorrhagic stroke in a well-defined community of southern Italy, 1993–1995. European Journal of Neurology 10 (2003): 559-565.
- Asplund K, Stegmayr B, Peltonen M. Stroke in the 21st Century: A Snapshot of the Burden, Epidemiology, and Quality of Life. In: Ginsberg MD, Bogousslavsky J, eds. cerebrovascular disease - pathophysiology, diagnosis and management. Boston: Blackwell Science (1998): 901-18.
- Barber M, Wright F, Stott DJ, et al. Predictors of early neurological deterioration after ischaemic stroke: a case-control study. Gerontology 50 (2004): 102-109.
- Heidelberg WH, Helsinki MK, Lausanne JB, et al. Ischaemic Stroke: Prophylaxis and Treatment. Information for doctors in hospitals and practice. European Stroke Initiative. Recommendations (2003).
- Sirtori CR, Gianfranceschi G, Gritti I, et al. Decreased high-density lipoprotein-cholesterol levels in male patients with transient ischemic attacks. Atherosclerosis 32 (1979): 205-211.
- Taggart H, Stout RW. Reduced high-density lipoprotein in stroke: relationship with elevated triglyceride and hypertension. Eur J Clin Invest 9 (1979): 219-221.
- Khor GL. Cardiovascular epidemiology in the Asia-Pacific region. Asia Pacific Journal of Clinical Nutrition 10 (2001): 76-80.
- Hsiang J, Zhu X, Wong L, et al. Putaminal and thalamic hemorrhage in ethnic Chinese living in Hong Kong. Surgical Neurology 46 (2009): 441-445.
- Ong TZ, Raymond AA. Risk Factors for Stroke and Predictors of One-Month Mortality. Singapore Med J 43 (2002): 517-521.
- Juvela S. Risk Factors for Impaired Outcome After Spontaneous Intracerebral Hemorrhage. Arch Neurol 52 (1995): 1193-1200.
- Adnan IQ, Suri AKM, Safdar, K, et al. Michael RF. Intracerebral Hemorrhage in Blacks: Risk Factors, Subtypes, and Outcome. Stroke 28 (1997): 961-964.
- Zia E, Engstrom G, Svensson PJ, et al. Three-year survival and stroke recurrence rates in patients with primary intracerebral hemorrhage. Stroke 40 (2009): 3567-73.
- Yonghong Z, Reilly KH; Tong, Weijun; Xu, Tan; Chen, Jing; Bazzano, Lydia A; Qiao, Dawei; Ju, Zhong; Chen, Chung-Shiuan; He, Jiang Blood pressure and clinical outcome among patients with acute stroke in Inner Mongolia, Chin a. Journal of Hypertension 2008; 26(7):1446-1452.