Severe Hypercalcaemia as a Consequence of Parathyroid Crisis - A Case Report
Article Information
Rafiqul Hasan1*, Md. Rezaul Alam2, Ferdous Jahan2, A. K. M Shahidur Rahman2, Md. Saiful Islam3
1Assistant Professor, Department of Medicine, Cox’s bazar Medical College, Cox’s bazar, Bangladesh
2Medical officer, Department of Nephrology, Bangabandhu Sheikh Mujib Medical University (BSMMU), Dhaka, Bangladesh
3Research Assistant, Department of Hepatology, Bangabandhu Sheikh Mujib Medical University (BSMMU), Dhaka, Bangladesh
*Corresponding Author: Dr. Rafiqul Hasan, Assistant Professor, Department of Medicine, Cox’s bazar Medical College, Cox’s bazar, Bangladesh
Received: 05 July 2021; Accepted: 22 July 2021; Published: 26 July 2021
Citation: Hasan R, Alam MR, Jahan F, Rahman AKMS, Islam MS. Severe Hypercalcaemia as a Consequence of Parathyroid Crisis - A Case Report. Archives of Clinical and Medical Case Reports 5 (2021): 567-574.
View / Download Pdf Share at FacebookAbstract
36-years old man presenting with the complaint of sudden severe upper abdominal pain, vomiting and polyuria with raised serum creatinine (2.74 mg/dl), serum calcium (19.68 mg/dl) and intact parathyroid hormone (iPTH) (2014.70 pg/ml) level. His ultrasound image of neck region demonstrated hypoechoic mass (12×10 mm) at left inferior parathyroid gland. Parathyroid schintography reported positive for parathyroid adenoma (left lower). He underwent medical management followed by parathyroidectomy. Optimum serum calcium concentration is essential for homeostasis and function of multiple organ systems. Severe hypercalcaemia is rare but life threatening complication of primary hyperparathyroidism (PHPT). In order to prevent mortality, it is necessary to provide immediate appropriate treatment by correcting hypercalcaemia and dehydration.
Keywords
Hypercalcaemia; Parathyroid Adenoma; Parathyroid Crisis; Parathyroid Hormone (PTH); Primary Hyperparathyroidism (PHPT)
Hypercalcaemia articles; Parathyroid Adenoma articles; Parathyroid Crisis articles; Parathyroid Hormone (PTH) articles; Primary Hyperparathyroidism (PHPT) articles
Hypercalcaemia articles Hypercalcaemia Research articles Hypercalcaemia review articles Hypercalcaemia PubMed articles Hypercalcaemia PubMed Central articles Hypercalcaemia 2023 articles Hypercalcaemia 2024 articles Hypercalcaemia Scopus articles Hypercalcaemia impact factor journals Hypercalcaemia Scopus journals Hypercalcaemia PubMed journals Hypercalcaemia medical journals Hypercalcaemia free journals Hypercalcaemia best journals Hypercalcaemia top journals Hypercalcaemia free medical journals Hypercalcaemia famous journals Hypercalcaemia Google Scholar indexed journals leukemia articles leukemia Research articles leukemia review articles leukemia PubMed articles leukemia PubMed Central articles leukemia 2023 articles leukemia 2024 articles leukemia Scopus articles leukemia impact factor journals leukemia Scopus journals leukemia PubMed journals leukemia medical journals leukemia free journals leukemia best journals leukemia top journals leukemia free medical journals leukemia famous journals leukemia Google Scholar indexed journals Parathyroid Adenoma articles Parathyroid Adenoma Research articles Parathyroid Adenoma review articles Parathyroid Adenoma PubMed articles Parathyroid Adenoma PubMed Central articles Parathyroid Adenoma 2023 articles Parathyroid Adenoma 2024 articles Parathyroid Adenoma Scopus articles Parathyroid Adenoma impact factor journals Parathyroid Adenoma Scopus journals Parathyroid Adenoma PubMed journals Parathyroid Adenoma medical journals Parathyroid Adenoma free journals Parathyroid Adenoma best journals Parathyroid Adenoma top journals Parathyroid Adenoma free medical journals Parathyroid Adenoma famous journals Parathyroid Adenoma Google Scholar indexed journals COVD-19 articles COVD-19 Research articles COVD-19 review articles COVD-19 PubMed articles COVD-19 PubMed Central articles COVD-19 2023 articles COVD-19 2024 articles COVD-19 Scopus articles COVD-19 impact factor journals COVD-19 Scopus journals COVD-19 PubMed journals COVD-19 medical journals COVD-19 free journals COVD-19 best journals COVD-19 top journals COVD-19 free medical journals COVD-19 famous journals COVD-19 Google Scholar indexed journals Parathyroid Crisis articles Parathyroid Crisis Research articles Parathyroid Crisis review articles Parathyroid Crisis PubMed articles Parathyroid Crisis PubMed Central articles Parathyroid Crisis 2023 articles Parathyroid Crisis 2024 articles Parathyroid Crisis Scopus articles Parathyroid Crisis impact factor journals Parathyroid Crisis Scopus journals Parathyroid Crisis PubMed journals Parathyroid Crisis medical journals Parathyroid Crisis free journals Parathyroid Crisis best journals Parathyroid Crisis top journals Parathyroid Crisis free medical journals Parathyroid Crisis famous journals Parathyroid Crisis Google Scholar indexed journals treatment articles treatment Research articles treatment review articles treatment PubMed articles treatment PubMed Central articles treatment 2023 articles treatment 2024 articles treatment Scopus articles treatment impact factor journals treatment Scopus journals treatment PubMed journals treatment medical journals treatment free journals treatment best journals treatment top journals treatment free medical journals treatment famous journals treatment Google Scholar indexed journals CT articles CT Research articles CT review articles CT PubMed articles CT PubMed Central articles CT 2023 articles CT 2024 articles CT Scopus articles CT impact factor journals CT Scopus journals CT PubMed journals CT medical journals CT free journals CT best journals CT top journals CT free medical journals CT famous journals CT Google Scholar indexed journals Genotype articles Genotype Research articles Genotype review articles Genotype PubMed articles Genotype PubMed Central articles Genotype 2023 articles Genotype 2024 articles Genotype Scopus articles Genotype impact factor journals Genotype Scopus journals Genotype PubMed journals Genotype medical journals Genotype free journals Genotype best journals Genotype top journals Genotype free medical journals Genotype famous journals Genotype Google Scholar indexed journals Parathyroid Hormone articles Parathyroid Hormone Research articles Parathyroid Hormone review articles Parathyroid Hormone PubMed articles Parathyroid Hormone PubMed Central articles Parathyroid Hormone 2023 articles Parathyroid Hormone 2024 articles Parathyroid Hormone Scopus articles Parathyroid Hormone impact factor journals Parathyroid Hormone Scopus journals Parathyroid Hormone PubMed journals Parathyroid Hormone medical journals Parathyroid Hormone free journals Parathyroid Hormone best journals Parathyroid Hormone top journals Parathyroid Hormone free medical journals Parathyroid Hormone famous journals Parathyroid Hormone Google Scholar indexed journals Primary Hyperparathyroidism articles Primary Hyperparathyroidism Research articles Primary Hyperparathyroidism review articles Primary Hyperparathyroidism PubMed articles Primary Hyperparathyroidism PubMed Central articles Primary Hyperparathyroidism 2023 articles Primary Hyperparathyroidism 2024 articles Primary Hyperparathyroidism Scopus articles Primary Hyperparathyroidism impact factor journals Primary Hyperparathyroidism Scopus journals Primary Hyperparathyroidism PubMed journals Primary Hyperparathyroidism medical journals Primary Hyperparathyroidism free journals Primary Hyperparathyroidism best journals Primary Hyperparathyroidism top journals Primary Hyperparathyroidism free medical journals Primary Hyperparathyroidism famous journals Primary Hyperparathyroidism Google Scholar indexed journals
Article Details
1. Introduction
Hypercalcaemia is a clinical disorder that most generally results from malignancy or primary hyperparathyroidism (PHPT) [1-4]. Other causes incorporate tertiary hyperparathyroidism, familial hypocalciuric hypercalcaemia, hyperthyroidism, drug impacts, sarcoidosis, tuberculosis, and immobilization [1]. Hypercalcemic emergency (severe hypercalcaemia) doesn't have a definite definition, albeit stamped height of serum calcium, typically in excess of 14 mg/dl, is related with intense signs and side effects of hypercalcaemia. The symptoms are as often as possible vague reflecting of multi-organ involvement with gastrointestinal, renal, neuromuscular and focal sensory system dysfunction [5].
Primary hyperparathyroidism is the unregulated over production of parathyroid hormone (PTH), bringing about strange calcium homeostasis. Parathyroid emergency is likewise known as parathyroid crisis; an uncommon and possibly lethal inconvenience of primary hyperparathyroidism (PHPT), wherein patients usually have severe hypercalcaemia with signs and side effects of various organ dysfunctions. Patients frequently show metabolic encephalopathy, renal insufficiency, gastrointestinal manifestations and cardiovascular dysrhythmia [6]. Prognosis is poor: mortality is almost 100% in non-operable cases and 20% cases in which parathyroidectomy is performed [7]. Therefore proper evaluation, early diagnosis and appropriate therapy are vital.
2. Case Report
A-36 years old man, married, known to be non-diabetic, normotensive hailing from Gulshan, Dhaka, admitted in Department of Medicine, Dhaka Medical College Hospital (DMCH), Dhaka, Bangladesh with the complaints of sudden severe upper abdominal pain and repeated vomiting for 4 days. The pain was diffuse, constant, radiated to the back, aggravated by taking meal and partially relieved by leaning forward position and antispasmodic. Patient noticed several episodes of vomiting for one day before hospital admission. Vomiting was non-projectile, contained ingested food materials, not mixed with blood or bile and not associated with food intake or headache. He also noticed nausea, anorexia, weakness and lethargy during the course of illness. On query; patient gave the history of frequent passage of large volume urine for last 3 days, which was more than 3 liter/24 hours, associated with dryness of mouth and increased with water intake. His bowel habit was normal. There was no history of hematemesis, melaena, red color urine, sense of burning micturition, depression, unconsciousness, palpitation, weight loss, cough, fever, joint pain, rash, gall stone disease or head injury. Patient was non-alcoholic but ex-smoker with 20 sticks of cigarette/day. He belongs to a family of middle socioeconomic condition. There was no significant family history or any contributing drug history related to this illness. On examination; patient was ill looking, moderately dehydrated and felt comfort on leaning forward position. His pulse rate was 88 beats per minute, blood pressure was 100/60 mm of Hg, respiratory rate was 16 breaths per minute and temperature was recorded 98.8° F (at the time of examination). Anaemia, jaundice, cyanosis, bony tenderness, ascites were absent. His abdomen was tender over epigastric region. Upper border of liver dullness present over 5th intercostal space along right mid-clavicular line. Bed side dipstick test of urine was negative for glucose and albumin. Biochemical assays revealed no abnormal findings in complete blood count (CBC) and urine routine microscopic examination (R/M/E) along with normal physiological level of serum electrolytes. serum alanine transaminase (ALT) and serum phosphate. Patient’s serum creatinine was initially rising (highest recorded level was 2.74 mg/dl) which was gradually decrease to normal limit after conservative management; indicated that it was acute kidney injury (AKI). Ultrasonography (USG) of whole abdomen revealed features of acute pancreatitis, mild fatty change in liver, relatively larger and swollen kidney with mild acute renal parenchymal disease. Initial urinary amylase was 626 U/L (normal level up to 500 U/L) and serum lipase was 1323 U/L (normal level: 23-300 U/L); consisting with acute pancreatitis. Serum calcium level was initially 12.8 mg/dl (normal limit is 8.5-10.5 mg/dl) which was increasing gradually and highest recorded value was 19.68 mg/dl. Serum intact parathyroid hormone (iPTH) level was 2014.70 pg/ml (normal value is 9-80 pg/ml), which indicated primary hyperparathyroidism. A twelve lead electrocardiogram (ECG) tracing showed cardiac arrhythmia, while endoscopy of upper gastrointestinal tract (GIT), plain X-ray abdomen A/P view in erect posture and X-ray skull A/P view were normal. USG of neck region and parathyroid scintigraphy showed features of left lower parathyroid adenoma (Figure 1 and Figure 2).
The patient was finally diagnosed as a case of acute kidney injury, acute pancreatitis due to hypercalcaemia a consequence of primary hyperparathyroidism (PHPT) as a result of left lower parathyroid adenoma (Parathyroid crisis). The patient was transferred to the coronary care unit (CCU) for observation of cardiac arrhythmia and symptomatic treatment. To decrease the serum calcium concentration the patient received; Inj. Salmon Calcitonin (200 IU/ml) 6 IU/kg - 8 hourly, given by subcutaneous route; Inj. Zoledronic Acid (4 mg/5 ml) mixed with 100 ml Normal Saline infused intravenously over 1 hour; Inj. Hydrocortisone (20 mg) 1 amp was given through intravenously every 6 hourly. In addition; intravenous normal saline was infused accordingly for correcting dehydration.
The initial treatment was successful and follow up on 4th day of hospitalization showed general well-being like- nausea, anorexia, weakness, and lethargy were improved; dehydration and polyuria were corrected; serum calcium level became normal. Surgical exploration of the neck was carried out on 7th day of hospitalization and thereafter the serum parathyroid hormone (PTH) level had been reduced to 60.8 mg/dl (4 days after surgery). A parathyroid adenoma of 12 × 10 × 10 mm, with a weight of 4.8 g was found and removed. The remaining parathyroid glands were found normal in size and left untouched. Histological examination revealed the parathyroid adenoma (Figure 3). Serum calcium and the intact parathyroid hormone (iPTH) levels were normalized. The patient was discharged 6 days after surgery with advice and has so far been followed up for a 12-month period without any sign symptoms of recurrence or other endocrine disorders.
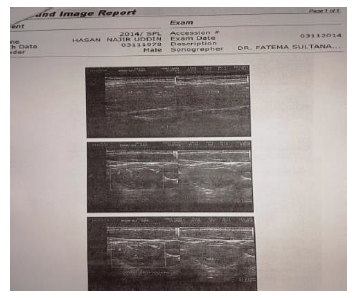
Figure 1: Ultrasound image demonstrates a hypoechoic mass, 12 × 10 × 1 0 mm, inferior and posterior to the left lobe of the thyroid, consistent an enlarged left inferior parathyroid gland.
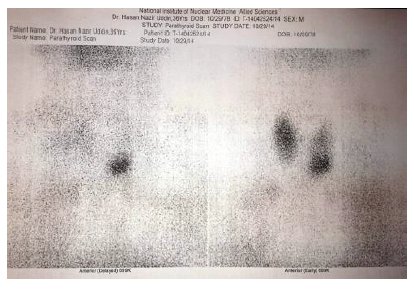
Figure 2: Parathyroid scintigraphy reported positive for parathyroid adenoma (Left lower).
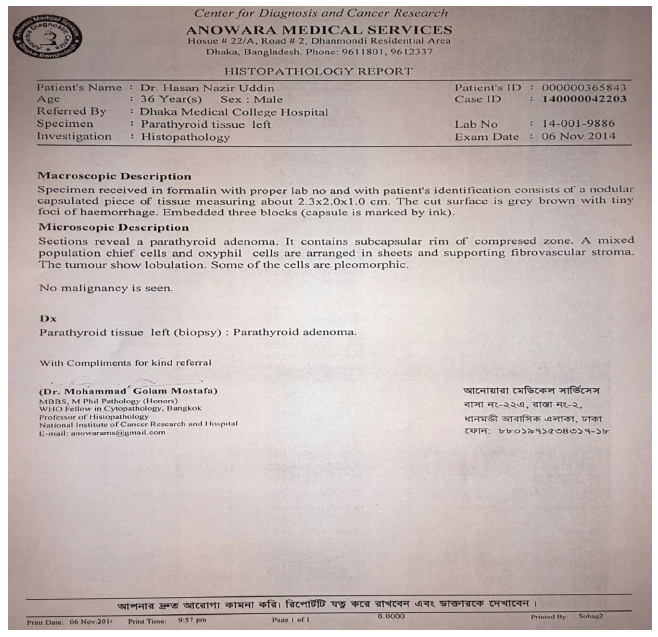
Figure 3: Histopathology report of parathyroid tissue reveals parathyroid adenoma.
3. Discussion
In this report, we portrayed an instance of a youngster with serious hypercalcaemia with intact parathyroid hormone (iPTH) level was over abundance of 2014.70 pg/ml. Diagnostic evaluation confirmed the presence of an huge (4.8 g) parathyroid adenoma. Hypercalcaemia and hyperparathyroidism were settled quickly following initial medical management and finally adenoma resection. We believe that our patient's findings reflect the most severe clinical manifestations of primary hyperparathyroidism (PHPT). While, PHPT brought about by parathyroid adenoma is normal, this case is novel for a few reasons. To begin with; severe hypercalcaemia is uncommon in PHPT. In this case level of serum calcium was 19.68 mg/dl. This degree of hypercalcaemia results only when PHPT is exceptionally severe (as in this case) or when tertiary hyperparathyroidism develops (like- autonomous hyperparathyroidism, hypersecretion after long-standing renal insufficiency etc). Vasoconstriction initiated by severe hypercalcaemia is a significant contributing reason for the acute renal failure as saw in this understanding. The resultant decrease in glomerular filtration rate (GFR) probably represented his normal serum phosphate level, which are commonly low to normal, typical in PHPT. In this setting of hypercalcaemia where primary or tertiary hyperparathyroidism is suspected, doctors ought to search other etiologies (for example malignancy, thiazide or lithium use, milk-antacid disorder, hypervitaminosis D and granulomatous infection). Secondly, the especially raised iPTH (>2000 pg/ml) usually observed in secondary or tertiary hyperparathyroidism. In a new arrangement of 80 patients with primary hyperparathyroidism from parathyroid adenoma, the most elevated announced PTH concentration was 2578 pg/ml [7].
Third, the size of this patient's parathyroid adenoma was quite large [12 × 10 × 10 mm (Figure 1)]. In primary hyperparathyroidism, adenoma size is an important determinant of disease severity, but the reason for such large variation (100-fold) in size is unknown. Two recent studies reported normal parathyroid glands weights from 62.4 ± 31.6 mg [8] and from 42.6 ± 20.3 mg [9], respectively. It was reported that, the mean parathyroid adenoma weight was 553.7 ± 520.5 mg [10]. This patient's parathyroid adenoma weighed 4.8 g, making it significantly larger than most reported parathyroid adenomas. Adenomas weighing more than 60 g have been rarely reported [10, 11]. Fourth, this patient endured acute kidney injury, doubtlessly because of severe hypercalcaemia (19.68 mg/dl). Serum calcium concentrations from 12.0 to 15.0 mg/dl have been appeared to diminish GFR by direct vasoconstriction and natriuresis prompting volume exhaustion and pre-renal azotemia [12]. Additionally, aquaporin-2 downregulation along with tubulointerstitial injury resulting in impaired osmotic gradient formation may preclude effective urine concentrating mechanisms [13]. Rather than an exceptional case of primary hyperparathyroidism, most of this patient's clinical features are more consistent with parathyroid carcinoma. Parathyroid carcinoma accounted for only 0.74% of more than 22000 cases of ‘primary hyperparathyroidism’ in a large retrospective study.7 Total serum calcium concentrations were >14 mg/dl in more than 66% of carcinoma cases [8]. Nephrolithiasis, nephrocalcinosis and impaired kidney function were found in 32-80% of patients with parathyroid carcinoma compared with 4-18% in benign primary hyperparathyroidism [14]. In this case, there was no evidence of malignancy.
Hypercalcemic emergency is described by severe hypercalcaemia, generally with a serum calcium >3.5 mmol/l (>14 mg/dl), with related sign and symptoms involving different organ systems and patients frequently show metabolic encephalopathy, renal insuficiency, gastrointestinal manifestations, cardiovascular dysrhythmia and a normochromic normocytic anaemia [15-21]. Malignancy is the most widely recognized reason for hypercalcemic emergency, which results from hypersecretion of PTH related polypeptide or from bone resorption identified with osseous metastasis [16].
Severe hypercalcaemia is a medical emergency and underlying therapy depends to the etiology. Therapy is aimed at increasing renal excretion of calcium and decreasing bone resorption [15-17]. Patients with hypercalcaemic crisis are volume depleted and initial therapy should be intravenous hydration with isotonic saline. The conventional use of loop diuretics to promote calciuresis is currently under scrutiny as this may exacerbate extracellular volume depletion through concomitant sodium diuresis [16, 17]. Bisphosphonates, which directly inhibit osteoclast activity, are the most effective of the pharmacological agents that decrease bone resorption. Pamidronate has gained acceptance as the drug of choice since it is the most potent bisphosphonate and has the fewest side effects [16].
For patients with parathyroid crisis, surgical procedure should be implemented, after preliminary medical management. Recent studies involving urgent parathyroidectomy has suggested excellent results with perioperative mortality of less than 5% [18-21]. As for all patients with PHPT, around 85-90% of patients with parathyroid crisis have a solitary adenoma [18-21]. It was reported that, serum parathyroid hormone (PTH) levels decrease quickly after parathyroidectomy, while serum calcium level normalized within a few days [17-18]. The adjustment of serum calcium and PTH is complemented by improvement of bone-pain, renal insufficiency, cardiac dysrhythmias and mental status changes. Complete resolution of the metabolic derangements including improvement of bone, renal and hematological abnormalities may take six to twelve months [17-18].
4. Conclusion
Hyperparathyroidism must be considered at the top among the differential diagnosis for severe hypercalcaemia in all age groups. These patients may present with a wide range of clinical symptoms related to metabolic derangements of multiple organ systems. Initial medical management should aim to lowering serum calcium by increasing renal excretion of calcium and reducing bone resorption. Patients should undergo urgent parathyroidectomy. Surgical resection results in prompt correction of serum calcium and parathyroid hormone level along with gradual resolution of the metabolic consequences of severe hypercalcaemia.
Conflicts of Interest
The authors declare no conflicts of interest regarding the publication of this case report.
Ethical Approval
Our institutions do not require ethical approval for reporting individual cases or case series.
References
- Walsh J, Gittoes N, Selby P, Society for Endocrinology Clinical Committee. Society for Endocrinology Endocrine Emergency Guidance: Emergency management of acute hypercalcaemia in adult patients. Endocrine connections 5 (2016): G9.
- Ariyan CE, Sosa JA. Assessment and management of patients with abnormal calcium. Critical care medicine. 32 (2004): S146-S154.
- Dent DM, Miller JL, Klaff L, et al. The incidence and causes of hypercalcaemia. Postgraduate medical journal 63 (1987): 745-750.
- Edelson GW, Kleerekoper M. Hypercalcemic crisis. The Medical clinics of North America 79 (1995): 79-92.
- Chan AK, Duh QY, Katz MH, et al. Clinical manifestations of primary hyperparathyroidism before and after parathyroidectomy. A case-control study. Annals of surgery 222 (1995): 402.
- Walker MD, Fleischer J, Rundek T, et al. Carotid vascular abnormalities in primary hyperparathyroidism. The Journal of Clinical Endocrinology & Metabolism 94 (2009): 3849-3856.
- Erbil Y, Ademoglu E, Ozbey N, et al. Reply-Correlations between Vitamin D Status and Biochemical/Clinical and Pathological Parameters in Primary Hyperparathyroidism. World Journal of Surgery 30 (2006): 2299-2300.
- Yao K, Singer FR, Roth SI, et al. Weight of normal parathyroid glands in patients with parathyroid adenomas. The Journal of Clinical Endocrinology & Metabolism 89 (2004): 3208-3213.
- Ghandur-Mnaymneh LA, Cassady J, Hajianpour MA, et al. The parathyroid gland in health and disease. The American journal of pathology 125 (1986): 292.
- Power C, Kavanagh D, Hill AD, et al. Unusual presentation of a giant parathyroid adenoma: report of a case. Surgery today 35 (2005): 235-237.
- Tsuchiya A, Endo S, Abe R. Giant adenoma of the parathyroid: report of a case. Surgery today 23 (1993): 465-467.
- Lins LE. Reversible renal failure caused by hypercalcaemia: a retrospective study. Acta Medica Scandinavica 203 (1978): 309-314.
- Rosen S, Greenfeld Z, Bernheim J, et al. Hypercalcemic nephropathy: chronic disease with predominant medullary inner stripe injury. Kidney international 37 (1990): 1067-1075.
- Shane E. Parathyroid carcinoma. The Journal of Clinical Endocrinology & Metabolism 86 (2001): 485-493.
- Kebebew E, Clark OH. Parathyroid adenoma, hyperplasia, and carcinoma: localization, technical details of primary neck exploration, and treatment of hypercalcemic crisis. Surgical oncology clinics of North America 7 (1998): 721-748.
- Edelson GW, Kleerekoper M. Hypercalcemic crisis. The Medical clinics of North America 79 (1995): 79-92.
- Clark JH, Schrader WT, O'Malley BW. Textbook of endocrinology. by Wilson JD, Foster DW, Saunders, Philadelphia. (1992): 35-90.
- Wang CA, Guyton SW. Hyperparathyroid crisis: clinical and pathologic studies of 14 patients. Annals of surgery 190 (1979): 782.
- Fitzpatrick LA, Bilezikian JP. Acute primary hyperparathyroidism. The American journal of medicine 82 (1987): 275-282.
- Maselly MJ, Lawrence AM, Brooks M, et al. Hyperparathyroid crisis. Successful treatment of ten comatose patients. Surgery 90 (1981): 741-746.
- Schweitzer VG, Thompson NW, Harness JK, et al. Management of severe hypercalcaemia caused by primary hyperparathyroidism. Archives of Surgery 113 (1978): 373-381.
