Severe Generalized Sweet Syndrome with good outcome: A Case Report
Article Information
Migena Vargu1, Petrit Vargu2, Sabina Dedej1, Eriselda Kurushi1, Samuele Vargu1, Alecia Anyim 3, Elsie Tachie Mensah 3 Ibrahim Gowaily 4, Jaclyn Tan-Wohlers 5, Grace Lin 5 Gurparneet Kaur Sohi 6 , Abdelrahman Awad 7 , Henri Fero 8 Yousra Abdalla 9, Alma Lamo10 ,Juna Musa11*
1Department of Dermatology, University Hospital Center “Mother Teresa”, University of Medicine of Tirana, Rruga e Dibrës, Tiranë, Albania
2Department of Emergency, University Hospital Center “Mother Teresa”, University of Medicine of Tirana, Rruga e Dibrës, Tiranë, Albania
3Department of Internal Medicine, Mayo Clinic, Rochester, USA
4Faculty of Medicine Tanta University, Qism 2, Second Tanta, Gharbia Governorate, Egypt
5Department of Laboratory Medicine and Pathology, Mayo Clinic Rochester, Rochester, USA
6Department of Nephrology and Hypertension ,Mayo Clinic , MN, USA
7Department of Internal Medicine, Mansoura ,Egypt
8German Hospital International Department of Internal Medicine, Tirana Albania
9Department of Neurology, Mayo Clinic, Rochester, Minnesota, USA
10Department of Pharmacy American Hospital ,Tirane,Albania
11Department of Endocrinology Diabetes and Nutrition Mayo Clinic, Rochester, Minnesota, USA
*Corresponding author: Juna Musa, Department of Endocrinology Diabetes and Nutrition, Mayo Clinic, Rochester, Minnesota, USA.
Received: 05 February 2025; Accepted: 11 February 2025; Published: 15 March 2025
Citation:
Migena Vargu, Petrit Vargu, Sabina Dedej, Eriselda Kurushi, Samuele Vargu, Alecia Anyim, Elsie Tachie Mensah, Ibrahim Gowaily, Jaclyn Tan-Wohlers, Grace Lin, Gurparneet Kaur Sohi, Abdelrahman Awad, Henri Fero, Yousra Abdalla, Alma Lamo, Juna Musa. Severe Generalized Sweet Syndrome with good outcome: A Case Report. Archives of Clinical and Biomedical Research. 9 (2025): 88-91.
View / Download Pdf Share at FacebookAbstract
Sweet syndrome (SS), also known as acute febrile neutrophilic dermatosis, is characterized by fever, elevated white blood cell counts predominantly composed of neutrophils, painful red plaques on the skin, and dermal neutrophilic infiltration without vasculitis. SS can be triggered by various factors and is diagnosed based on clinical, laboratory, and histopathological criteria. SS is classified into three types: classical (or idiopathic), malignancy-associated, and drug-induced. Classical Sweet syndrome is the most common form, often linked to infectious diseases, inflammatory disorders, or pregnancy. This case report describes a patient with an aggravated and generalized form of Sweet syndrome who had a favorable outcome following appropriate treatment.
Keywords
Sweet syndrome; Pregnancy; Fever; Vasculitis; Infectious diseases; Inflammatory disorders; Neutrophils
Sweet syndrome articles; Pregnancy articles; Fever articles; Vasculitis articles; Infectious diseases articles; Inflammatory disorders articles; Neutrophils articles
Article Details
1. Introduction
Sweet syndrome (SS), also known as acute febrile neutrophilic dermatosis, was first described by Dr. Robert Sweet in 1964 [1]. This condition is characterized by a set of distinct clinical and histological features, including fever, elevated white blood cell count with a predominance of neutrophils, painful red plaques on the skin, and dermal infiltration by neutrophils without evidence of vasculitis [2,3]. Sweet syndrome can be triggered by various factors and is diagnosed based on specific clinical, laboratory, and histopathological criteria. Sweet syndrome can be categorized into three main types: classical (or idiopathic), malignancy-associated, and drug-induced. Classical Sweet syndrome is the most common form and is linked to infectious diseases, inflammatory disorders, or pregnancy [3-5]. Here, we present a patient suffering from an aggravated and generalized form of Sweet syndrome with a good outcome.
2. Case Presentation
A 59-year-old female presented to the emergency department with a three-week history of high fever, cough, and painful red lesions on her face, trunk, and extremities. Her medical history included long-term use of Clozapine since 2008 for schizoaffective disorder, and she was under regular psychiatric follow-up. Due to her medical history, a psychiatric consultation was requested, raising suspicion of Clozapine-induced Stevens-Johnson syndrome (SJS)/toxic epidermal necrolysis (TEN) [6,7]. Consequently, Clozapine was discontinued, and Risperidone was initiated. A thorough dermatological examination revealed erythematous, edematous, and painful plaques of varying sizes and target-like lesions on her head, trunk, upper, and lower extremities, with sparing of the palmar and plantar regions as well as the mucous membranes. Nikolsky's sign was negative, and her overall condition was stable. Hospitalization followed, and comprehensive diagnostic workup including laboratory tests, imaging, and histopathological examinations was performed [8-10]. Laboratory findings indicated elevated white blood cell count and neutrophilia. Chest X-ray and abdominal ultrasound were normal. A skin biopsy showed subcorneal pustules with eosinophils and neutrophils, spongiosis in the epidermis, and dense papillary edema with mixed inflammatory infiltrates, confirming Sweet syndrome. Evaluating the criteria for drug-induced Sweet syndrome, the patient did not meet the temporal relationship criterion between the onset of medication and symptom appearance. Additionally, investigations for infectious, autoimmune, and malignant diseases were negative, leading to a final diagnosis of classic Sweet syndrome [11]. Treatment with intravenous Prednisolone 100 mg was initiated and gradually tapered, resulting in significant clinical improvement without relapse or complications. Despite the generalized nature of the lesions, covering approximately 90% of the body surface area, the disease was successfully managed without the need for additional immunosuppressive therapy [12].
3. Discussion
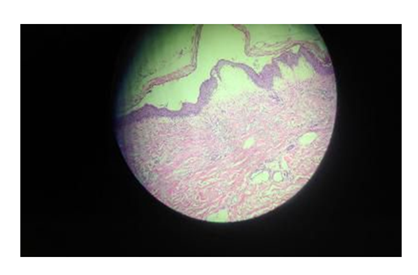
Sweet syndrome (SS) is a rare condition that predominantly affects women, with a female-to-male ratio o 4 to 1. It typically occurs in individuals aged 30 to 60 years, but cases have also been documented in both children and older adults. There is no known racial predilection for this condition (Figure 1).
The diagnosis of SS is based on fulfilling two major criteria: the abrupt onset of painful erythematous plaques or nodules and histopathological evidence of a dense neutrophilic infiltrate without vasculitis. Additionally, at least two of the following minor criteria should be met: fever, association with an underlying condition (such as malignancy, inflammatory disease, or pregnancy), excellent response to systemic corticosteroids, and abnormal laboratory values (elevated erythrocyte sedimentation rate, positive C-reactive protein, leukocytosis, and neutrophilia) [13,14]. In our case, the patient had been taking Clozapine for 16 years without previous manifestations of SS (Figure 2 and 3).
Drug-induced Sweet syndrome must fulfill all five criteria proposed by Walker and Cohen: abrupt onset of painful erythematous plaques or nodules, pyrexia >38°C, temporal relationship between drug ingestion and clinical presentation, temporally related recurrence after oral challenge, and temporally related resolution of lesions after drug withdrawal or treatment with systemic corticosteroids [15]. Since the fourth criterion was not established, we excluded drug etiology as the trigger for the disease. However, Clozapine has been reported to induce SS in three studies. Our patient met the major and minor criteria for classical SS, likely due to a respiratory tract infection, as she had a persistent cough for several days (Figure 4).
The skin lesions in SS are typically painful and erythematous, most commonly found on the face, neck, and upper extremities. Other relatively new dermatological manifestations include bullous, cellulitis-like, necrotizing, neutrophilic dermatosis of the dorsal hands, and generalized pustular variants. These lesions are usually localized to specific body sites [16]. In our case, multiple plaques were spread almost all over the body, posing diagnostic and management challenges. Painful, target-like, and generalized lesions in a febrile patient taking antipsychotics should primarily raise suspicion of SJS/TEN, which was excluded by a careful clinical approach and confirmed by biopsy revealing a dense neutrophilic infiltrate.
The exact pathogenesis of Sweet syndrome remains unclear, but several mechanisms have been proposed, involving infections, immune reactions, cytokines, and potentially genetic causes. The condition often presents with fever and elevated white blood cell counts, indicating a possible infectious origin. Sweet syndrome may also be driven by a hypersensitivity reaction to bacterial, viral, or tumor antigens, as suggested by the syndrome's rapid response to corticosteroids. Potentially involved cytokines in SS include granulocyte-colony stimulating factor (G-CSF), granulocyte-macrophage colony-stimulating factor, interferon-gamma, and several interleukins. Cases of SS have been reported following G-CSF treatment or in patients with tumors producing G-CSF [17,18]. Studies have shown elevated serum values of cytokines like G-CSF and interleukin-6 in tumor tissues. Increased levels of helper T-cell type 1 cytokines and normal levels of helper T-cell type 2 cytokines have been found in patients' serum. A possible genetic link with HLA-B54 has been observed in two Japanese brothers who developed SS in the neonatal period (Figure 5 and 6).
The treatment of Sweet syndrome primarily involves corticosteroids, which are highly effective in controlling symptoms. The typical initial dose is 1 mg/kg/day, tapered over 4-6 weeks. For patients intolerant to corticosteroids, alternative first-line treatments include colchicine and potassium iodide. Second-line therapies include indomethacin, clofazimine, dapsone, and cyclosporine. Supportive care and treating any underlying conditions are crucial for managing the disease. Our patient was initially administered 100 mg of Prednisolone, with the dosage gradually tapered based on the progression of her lesions. During the three-week hospitalization period, she exhibited an excellent therapeutic response. No complications or involvement of other organs were observed.
4. Conclusions
Sweet syndrome is a rare but significant condition characterized by acute febrile neutrophilic dermatosis. Accurate diagnosis requires a combination of clinical, laboratory, and histopathological findings, guided by established diagnostic criteria. Early recognition and appropriate therapeutic intervention can lead to rapid symptom resolution and improve patient outcomes, especially in aggravated and widespread lesions.
References
- Sweet rd. An acute febrile neutrophilic dermatosis. Br J Dermatol 76 (1964): 349-356.
- Su WP, Liu HN. Diagnostic criteria for Sweet's syndrome. Cutis 37 (1986): 167-174.
- Cohen PR. Sweet's syndrome--a comprehensive review of an acute febrile neutrophilic dermatosis. Orphanet J Rare Dis (2007): 34.
- Jung EH, Park JH, Hwan Kim K, et al. Characteristics of Sweet syndrome in patients with or without malignancy. Ann Hematol 101 (2022): 1499-1508.
- Sáez M, García-Bustínduy M, Noda A, et al. Drug-induced Sweet's syndrome. J Eur Acad Dermatol Venereol 18 (2004): 233.
- Joshi TP, Friske SK, Hsiou DA, et al. New Practical Aspects of Sweet Syndrome. Am J Clin Dermatol 23 (2022): 301-318.
- Walker DC, Cohen PR. Trimethoprim-sulfamethoxazole-associated acute febrile neutrophilic dermatosis: case report and review of drug-induced Sweet's syndrome. J Am Acad Dermatol 34 (1996): 918-923.
- Bunting A, Silman D, Karia M, et al. Clozapine and Sweet's syndrome: case report. BJPsych Open 9 (2023): e166.
- Schonfeldt-Lecuona C, Connemann BJ. Sweet's syndrome and polyserositis with clozapine [published correction appears in Am J Psychiatry 160 (2003): 204.
- Kleinen JM, Bouckaert F, Peuskens J. Clozapinegeïnduceerde agranulocytose en het syndroom van Sweet bij een 74-jarige patiënte [Clozapine-induced agranulocytosis and Sweet's syndrome in a 74-year-old female patient. A case study]. Tijdschr Psychiatr 50 (2008): 119-123.
- Chen O, Partarrieu-Mejías F, Alarcón-Cabrera R. Erythema and bullae on the face and hands of a farm worker. Clin Exp Dermatol 44 (2019): 99-101.
- Surovy AM, Pelivani N, Hegyi I, et al. Giant cellulitis-like Sweet Syndrome, a new variant of neutrophilic dermatosis. JAMA Dermatol 149 (2013): 79-83.
- Hresko AM, Pickrell BB, Harper CM. Necrotizing Sweet Syndrome of the Hand and Forearm in the Immediate Postoperative Period: Case Report. Hand (N Y) (2023).
- Galaria NA, Junkins-Hopkins JM, Kligman D, et al. Neutrophilic dermatosis of the dorsal hands: pustular vasculitis revisited. J Am Acad Dermatol 43 ( 2000): 870-874.
- Heath MS, Ortega-Loayza AG. Insights Into the Pathogenesis of Sweet's Syndrome. Front Immunol 10 (2019): 414.
- Reuss-Borst MA, Müller CA, Waller HD. The possible role of G-CSF in the pathogenesis of Sweet's syndrome. Leuk Lymphoma 15 (1994): 261-264.
- Parsapour K, Reep MD, Gohar K, et al. Familial Sweet's syndrome in 2 brothers, both seen in the first 2 weeks of life. J Am Acad Dermatol 49 (2003): 132-138.
- Villarreal-Villarreal CD, Ocampo-Candiani J, Villarreal-Martínez A. Sweet Syndrome: A Review and Update. Actas Dermosifiliogr 107 (2016): 369-378.