Safety Comparison of Conventional Versus Extended Infusion of Pulse Methylprednisolone in Multiple Sclerosis Exacerbation
Article Information
Haider Alabd1*, Lolwa Barakat1, Bhagya Sree2, Prem Chandra3, Mohamed Khalil4, Mohamed Elshafei1
1Clinical Pharmacy Department, Hamad General Hospital, Hamad Medical Corporation, Doha, Qatar
2Clinical Pharmacy Department, Women’s wellness and research center, Hamad Medical Corporation Doha, Qatar
3Biostatstics section, Medical Research center, Hamad Medical Corporation, Doha, national
4Internal Medicine Department, Hamad General Hospital, Hamad Medical Corporation, Doha, Qatar
*Corresponding Author: Mohamed Nabil Elshafei, Clinical Pharmacy Department, Hamad General Hospital, Hamad Medical Corporation, Doha, Qatar.
Received: 10 November 2022; Accepted: 17 November 2022; Published: 28 December 2023
Citation: Haider Alabd, Lolwa Barakat, Bhagya Sree, Prem Chandra, Mohamed Khalil, Mohamed Elshafei. Safety Comparison of Conventional Versus Extended Infusion of Pulse Methylprednisolone in Multiple Sclerosis Exacerbation. Fortune Journal of Rheumatology 5 (2023): 22-30.
View / Download Pdf Share at FacebookAbstract
Objective: To determine the impact of Intravenous Methylprednisolone (IVMP) administration on the changes in vital signs (Heart Rate (HR), Systolic (SBP), Diastolic Blood Pressure (DBP), and serum potassium level in multiple sclerosis flare.
Design: retrospective review study conducted at Hamad General Hospital (HGH). All patients admitted in 2019-2020 with MS flare without any comorbidities were categorized into two groups depending on infusion rate. One group received a conventional IVMP dose over 30 minutes to one hour, while the second group received IVMP over an extended period) (four to six hours). After that, we assessed multiple readings of vital signs and potassium levels through steroid administration time to determine if there was an infusion-related significant difference in adverse events between both groups.
Methods: 74 adult patients with MS relapse admitted to Hamad General Hospital (HGH) and satisfied pre-specified inclusion criteria were invited to participate in the study.
Results: 74 patients with MS were included in the study; 61 patients (83.6%) received a methylprednisolone dose of 500 mg -1000 mg in a conventional infusion rate, while 12 patients (16.4%) received pulse steroids in an extended duration. Both groups had no significant difference in mean blood pressure before and after IVMP. There was a small but statistically significant increase in mean heart rate in the conventional group immediately after the first and second but not 3rd dose of IVMP compared to baseline 3.5± 8.9 and 4.85± 13.9 P < 0.003. There was a minimal non-significant increase in potassium level in the conventional group (P = 0.17), while there was a non-significant decrease in potassium level in the extended group (P=0.72).
Conclusion: IVMP is considered safe and effective in treating MS exacerbation regardless of intravenous infusion duration. There was no significant difference in vital signs among different infusion rates. However, there was a small but statistically significant increase in mean heart rate in the conventional group immediately after the first and second but not 3rd dose of IVMP compared to baseline. No significant difference was observed in potassium levels before and after IVMP. We, therefore, recommend restricting potassium level monitoring to patients with other risk factors of hypokalemia.
Keywords
Methylprednisolone; Multiple sclerosis; Hypokalemia; Blood pressure
Methylprednisolone articles; Multiple sclerosis articles; Hypokalemia articles; Blood pressure articles
Methylprednisolone articles Methylprednisolone Research articles Methylprednisolone review articles Methylprednisolone PubMed articles Methylprednisolone PubMed Central articles Methylprednisolone 2023 articles Methylprednisolone 2024 articles Methylprednisolone Scopus articles Methylprednisolone impact factor journals Methylprednisolone Scopus journals Methylprednisolone PubMed journals Methylprednisolone medical journals Methylprednisolone free journals Methylprednisolone best journals Methylprednisolone top journals Methylprednisolone free medical journals Methylprednisolone famous journals Methylprednisolone Google Scholar indexed journals Multiple sclerosis articles Multiple sclerosis Research articles Multiple sclerosis review articles Multiple sclerosis PubMed articles Multiple sclerosis PubMed Central articles Multiple sclerosis 2023 articles Multiple sclerosis 2024 articles Multiple sclerosis Scopus articles Multiple sclerosis impact factor journals Multiple sclerosis Scopus journals Multiple sclerosis PubMed journals Multiple sclerosis medical journals Multiple sclerosis free journals Multiple sclerosis best journals Multiple sclerosis top journals Multiple sclerosis free medical journals Multiple sclerosis famous journals Multiple sclerosis Google Scholar indexed journals Hypokalemia articles Hypokalemia Research articles Hypokalemia review articles Hypokalemia PubMed articles Hypokalemia PubMed Central articles Hypokalemia 2023 articles Hypokalemia 2024 articles Hypokalemia Scopus articles Hypokalemia impact factor journals Hypokalemia Scopus journals Hypokalemia PubMed journals Hypokalemia medical journals Hypokalemia free journals Hypokalemia best journals Hypokalemia top journals Hypokalemia free medical journals Hypokalemia famous journals Hypokalemia Google Scholar indexed journals Blood pressure articles Blood pressure Research articles Blood pressure review articles Blood pressure PubMed articles Blood pressure PubMed Central articles Blood pressure 2023 articles Blood pressure 2024 articles Blood pressure Scopus articles Blood pressure impact factor journals Blood pressure Scopus journals Blood pressure PubMed journals Blood pressure medical journals Blood pressure free journals Blood pressure best journals Blood pressure top journals Blood pressure free medical journals Blood pressure famous journals Blood pressure Google Scholar indexed journals cardiac arrhythmias articles cardiac arrhythmias Research articles cardiac arrhythmias review articles cardiac arrhythmias PubMed articles cardiac arrhythmias PubMed Central articles cardiac arrhythmias 2023 articles cardiac arrhythmias 2024 articles cardiac arrhythmias Scopus articles cardiac arrhythmias impact factor journals cardiac arrhythmias Scopus journals cardiac arrhythmias PubMed journals cardiac arrhythmias medical journals cardiac arrhythmias free journals cardiac arrhythmias best journals cardiac arrhythmias top journals cardiac arrhythmias free medical journals cardiac arrhythmias famous journals cardiac arrhythmias Google Scholar indexed journals hypokalemia articles hypokalemia Research articles hypokalemia review articles hypokalemia PubMed articles hypokalemia PubMed Central articles hypokalemia 2023 articles hypokalemia 2024 articles hypokalemia Scopus articles hypokalemia impact factor journals hypokalemia Scopus journals hypokalemia PubMed journals hypokalemia medical journals hypokalemia free journals hypokalemia best journals hypokalemia top journals hypokalemia free medical journals hypokalemia famous journals hypokalemia Google Scholar indexed journals intravenous infusion articles intravenous infusion Research articles intravenous infusion review articles intravenous infusion PubMed articles intravenous infusion PubMed Central articles intravenous infusion 2023 articles intravenous infusion 2024 articles intravenous infusion Scopus articles intravenous infusion impact factor journals intravenous infusion Scopus journals intravenous infusion PubMed journals intravenous infusion medical journals intravenous infusion free journals intravenous infusion best journals intravenous infusion top journals intravenous infusion free medical journals intravenous infusion famous journals intravenous infusion Google Scholar indexed journals cytokines articles cytokines Research articles cytokines review articles cytokines PubMed articles cytokines PubMed Central articles cytokines 2023 articles cytokines 2024 articles cytokines Scopus articles cytokines impact factor journals cytokines Scopus journals cytokines PubMed journals cytokines medical journals cytokines free journals cytokines best journals cytokines top journals cytokines free medical journals cytokines famous journals cytokines Google Scholar indexed journals Joint pain articles Joint pain Research articles Joint pain review articles Joint pain PubMed articles Joint pain PubMed Central articles Joint pain 2023 articles Joint pain 2024 articles Joint pain Scopus articles Joint pain impact factor journals Joint pain Scopus journals Joint pain PubMed journals Joint pain medical journals Joint pain free journals Joint pain best journals Joint pain top journals Joint pain free medical journals Joint pain famous journals Joint pain Google Scholar indexed journals neck pain articles neck pain Research articles neck pain review articles neck pain PubMed articles neck pain PubMed Central articles neck pain 2023 articles neck pain 2024 articles neck pain Scopus articles neck pain impact factor journals neck pain Scopus journals neck pain PubMed journals neck pain medical journals neck pain free journals neck pain best journals neck pain top journals neck pain free medical journals neck pain famous journals neck pain Google Scholar indexed journals
Article Details
Learning points
- Multiple Sclerosis (MS) relapses are typically defined as a new or worsening neurological deficit lasting 24 hours or more in the absence of fever or infection.
- High-dose short-term parenteral steroids are the standard of care for treating MS relapse.
- IVMP is relatively safe and effective in treating MS exacerbation regardless of intravenous infusion duration.
- There was no difference in vital signs fluctuation and potassium level between different infusion rates.
Introduction
Multiple Sclerosis (MS) relapses are defined as a new or worsening neurological deficit lasting 24 hours or more in the absence of fever or infection [1]. High-dose short-term parenteral steroids are the standard of care for treating MS relapse. The most common regimen used is 500mg-1000mg of IV methylprednisolone (MP) for 3- 5 days [1]. The common practice at Hamad General Hospital (HGH) is to administer MP infusion once daily. Still, there is always an inconsistent practice between physicians regarding infusion rate and duration due to a lack of guidelines or standards regarding infusion duration. Some prefer administering over 30 minutes to one hour; in contrast, others prefer extended infusion over 4-6 hours due to the conception of more adverse events such as cardiac arrhythmias and hypokalemia associated with the short infusion. However, extended infusion time will increase the length of hospital stay. Additionally, it increases the possibility of steroid infusion interruption due to the patient's mobility. Methylprednisolone manufacturing company mentioned that there are reports of cardiac arrhythmias and cardiac arrest following the rapid administration of large intravenous doses (greater than 0.5 grams administered over less than 10 minutes). In addition, Bradycardia has been reported during or after administering large doses of IVMP and may be unrelated to the speed or duration of infusion. Therefore, when a high steroid dose is wanted, the recommended dose must be administered over 30 minutes [2,7].
Adult case reports described unexpected cardiac arrest and death following high-dose IVMP infusions [6]. Most of these patients had a multisystem disease, but several had no evidence of a pre-existing cardiac condition. One adult and one pediatric case report developed severe Bradycardia associated with the infusion [3]. There is no established consensus on monitoring patients during and after IVMP administration.
One retrospective study analyzed the changes in vital signs, including heart rate (HR), systolic (SBP), and diastolic blood pressure (DBP)) after IVMP infusion in Thyroid eye disease, which showed that IVMP is safe and associated with mild and non-cumulative effects on vital signs when administered over 60 minutes. This study attributed the occurrence of hypertension or bradycardia to individual factors such as underlying hypertension, uncontrolled thyroid dysfunction, or medication usage, e.g., Beta-blockers [5]. For the above reasons, this retrospective comparative study is conducted to investigate the impact of IVMP infusion duration on vital signs and serum potassium levels in MS patients. Seventy-four patients with MS relapse with no other comorbidities were reviewed and classified into two groups; one group received pulse IVMP at a conventional rate over 1 or 2 hours, whereas the other group received extended infusion; both groups were monitored frequently during steroid infusion. Potassium level, blood pressure, and heart rate readings were recorded during hospitalization. These readings were analyzed to determine the effect of infusion duration of steroids on potassium level, HR, and BP among the two groups. This study protocol was approved by the Institutional Review Board (IRB) of Hamad Medical Corporation (MRC number: 01-18-024).
Method
We performed a retrospective review of seventy-four electronic medical records of MS patients administered methylprednisolone pulse therapy for MS flare through 2019 at Hamad General Hospital (HGH). Inpatients aged 18 years or older with MS flare without other comorbidities were categorized into two groups. Group 1 received intravenous methylprednisolone pulse therapy (500 -1000 mg) for 2-5 days over 1 – 2 hours, while group 2 received it over an extended period (3-6 hours). Blood pressure, heart rate, and potassium level were measured according to study protocol before, during, and after infusion of IVMP during the hospital stay, which varied from 2-to 5 days. Subsequently, data were analyzed to determine the effect of infusion duration on blood pressure, Heart rate, and potassium level variation between both groups. This study was approved by the Medical Research Center (MRC) of Hamad Medical Corporation (MRC number: 01-18-024). The mean value of the three measurements of systolic blood pressure, diastolic blood pressure, and pulse rate were included in the analysis. All subjects had their daily vital signs (HR, SBP, and DBP) recorded before infusion (baseline), after infusion immediately (post-infusion), and at a later point during the day (1st reading). Serum potassium was measured on admission before pulse MP and after infusion before discharge. Patients with hypertension, diabetes mellitus, chronic renal disease, cardiac disease, hyperthyroidism, and pregnant women were excluded from the study. Statistical analyses were performed using statistical software and the package SPSS 27.0 (IBM SPSS Inc. NY). We used Descriptive statistics to summarize and determine the sample characteristics, data distribution, and results. The normally distributed data and results were reported with mean and standard deviation (SD); the remaining results were reported with median and Inter-Quartile Range (IQR). Quantitative outcomes measured on each specific day between the two groups (conventional infusion rate vs. extended infusion rate) were compared using unpaired t or Mann-Whitney U tests as appropriate. Repeated measure analysis of variance (ANOVA) was performed to determine and assess differences in quantitative outcomes measured across different time points. All P values presented were two-tailed, and P values <0.05 were considered statistically significant.
Results
In the study, 61 (83.6%) out of 74 MS patients received a methylprednisolone dose of 500 mg-1000 mg through a conventional infusion rate (group 1). Conversely, 12 patients (16.4%) received pulse steroids for an extended duration (group 2), 688 blood pressure readings and 685 heart rate readings were collected. The mean baseline blood pressure before pulse steroid administration was (systolic 118.93+/-16.04 mmHg, diastolic 70.42+/- 9.44 mmHg), and baseline heart rate 76.66 +/- 11.2 beat per minute (BPM), The majority of patients underwent pulse infusion of methylprednisolone at a dosage of 1000 mg over 1hour [Table 1]. Throughout the five days of intravenous methylprednisolone (IVMP) administration, there weren't any notable variations in systolic or diastolic blood pressure changes between the conventional and extended groups (Tables 2-6 illustrate the daily mean blood pressure and heart rate readings throughout the five days of pulse steroids administration).
Methylprednisolone pulse administration had led to fluctuation in heart rate through either increasing or decreasing compared to the patient's initial or baseline measurements. [Figures 1, 2]. Our study’s results showed that there was a change in the mean heart rate across three specific time points over the span of five days: at baseline, immediately following the infusion, and at an additional reading taken later in the day. The mean heart rate was not significantly different between both groups [Tables 2-6]. A limited number of patients whose vital signs readings were measured and documented across all five days of the study period. Therefore, we conducted additional analysis focusing on the mean heart rate at two specific time points: baseline and immediately after IVMP administration. Our findings indicated a statistically significant increase in the mean heart rate in the conventional group immediately after the first and second but not the third dose of IVMP compared to baseline [Table 9, 10].
On the contrary, our analysis revealed no statistically significant difference in the mean heart rate following IVMP administration compared to the baseline within the extended group after the first, second, and third doses. The maximum and lowest patient’s heart rate obtained following IVMP administration were 102 BPM and 45 BPM, respectively. Even though methylprednisolone was administered over a one-hour period in both cases, only one patient exhibited tachycardia. However, this increase in heart rate was not attributable to the steroid infusion itself, suggesting an unrelated cause for the observed tachycardia in that patient. Six patients developed bradycardia (< 60 BPM); five out of six were in a conventional group on days 1,3,4, and 5, while one patient experienced bradycardia at day one in the extended group. For all patients, bradycardia resolved spontaneously. We collected 46 out of 74 participants' blood potassium levels before and after Methylprednisolone pulse administration [Table 8]. The mean baseline potassium level in the conventional and extended group was (4.05+/- 0.26), and (4.16 +/-0.35) mmol/L, respectively. Following Methylprednisolone administration, the potassium levels observed in the conventional group, averaging at 4.1+/-0.3 mmol/L, did not demonstrate any statistically significant difference compared to the potassium levels noted in the extended group, which averaged at 4.07+/-0.3 mmol/L (P= 0.72). There was a minimal increase in potassium level in the conventional group but not statistically significant p-value (P= 0.17). There was a non-statistically significant decrease in potassium level in the extended group p-value (P= 0.72). [Table 8]. No incidence of hypokalemia/hyperkalemia in both groups.
Table 1: Baseline characteristics of the patients along with HR and BP readings before and after IVMP administration.
|
Characteristics |
Conventional infusion rate n= 62 (83.6%) |
Extended infusion rate n= 12 (16.4%) |
|
Sex Male n=33 (44.6%) Female n=41 (55.4%) |
Male n=29 (39.2%) Female n= 33 (44.6%) |
Male n= 4 (5.4%) Female n=8 (10.8%) |
|
Methylprednisolone dose 500 mg N= 4 1000 mg N=70 |
500 mg N= 2 1000 mg N=60 |
500 mg N=2 1000 mg N= 10 |
|
Infusion time rate |
1hr n=37 2hr n=25 |
3hr n=1 4hr n=9 6hr n=2 |
|
DAY 1 |
||
|
BP baseline |
61 |
12 |
|
BP post-infusion immediately |
61 |
12 |
|
BP first reading post-infusion |
42 |
11 |
|
Heart rate baseline before infusion |
60 |
12 |
|
Heart rate post-infusion immediately |
60 |
12 |
|
Heart rate first reading post-infusion |
48 |
10 |
|
DAY 2 |
||
|
BP baseline |
56 |
10 |
|
BP post-infusion immediately |
56 |
11 |
|
BP first reading post-infusion |
41 |
8 |
|
Heart rate baseline before infusion |
55 |
11 |
|
Heart rate post-infusion immediately |
55 |
11 |
|
Heart rate first reading post-infusion |
44 |
6 |
|
DAY 3 |
||
|
BP baseline |
49 |
10 |
|
BP post-infusion immediately |
47 |
10 |
|
BP first reading post-infusion |
29 |
8 |
|
Heart rate baseline before infusion |
48 |
9 |
|
Heart rate post-infusion immediately |
48 |
9 |
|
Heart rate first reading post-infusion |
29 |
7 |
|
DAY 4 |
||
|
BP baseline |
32 |
4 |
|
BP post-infusion immediately |
32 |
4 |
|
BP first reading post-infusion |
19 |
3 |
|
Heart rate baseline before infusion |
31 |
4 |
|
Heart rate post-infusion immediately |
32 |
4 |
|
Heart rate first reading post-infusion |
20 |
3 |
|
DAY 5 |
||
|
BP baseline |
22 |
2 |
|
BP post-infusion immediately |
22 |
2 |
|
BP first reading post-infusion |
11 |
1 |
|
Heart rate baseline before infusion |
21 |
2 |
|
Heart rate post-infusion immediately |
21 |
2 |
|
Heart rate first reading post-infusion |
13 |
1 |
|
Total BP and HR readings in 5 days |
||
|
BP readings HR readings |
580 585 |
108 103 |
|
Baseline potassium level (Number of readings) |
39 |
7 |
|
Post pulse steroid potassium level (Number of readings) |
39 |
7 |
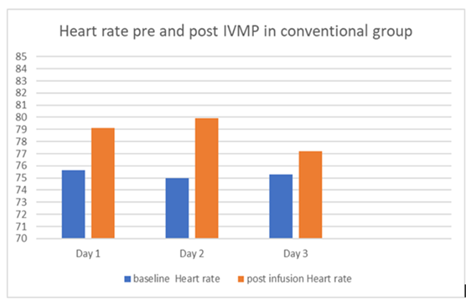
Figure 1: The comparison of heart rates before and after IVMP administration in the conventional group was conducted from day 1 to day 3.
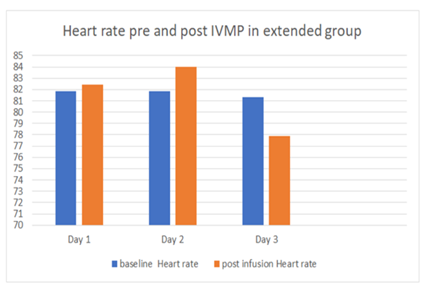
Figure 2: The comparison of heart rates before and after IVMP administration in the extended group was conducted from day 1 to day 3.
Table 2: The differences in blood pressure and heart rate on day 1 between the two groups.
|
Day 1 |
Conventional infusion rate |
Extended infusion rate |
P-value |
|
Systolic BP baseline (mmHg) Diastolic BP baseline (mmHg) |
118.3+/- 15.7 70.3+/- 9.8 |
122.9+/-18.3 70.5+/- 7.914 |
0.372 0.942 |
|
Systolic post infusion (mmHg) Diastolic post infusion (mmHg) |
120.2+/-14.3 70.95+/- 8.4 |
117.08+/-10.31 69.58+/-6.571 |
0.478 0.598 |
|
Systolic first reading (mmHg) Diastolic first reading (mmHg) |
118.7+/- 12.1 69.6+/- 8.2 |
116.3+/-7.7 68.5+/-5.7 |
0.537 0.661 |
|
Baseline Heart rate (BPM) |
75.6+/- 10.1 |
81.8+/- 15.3 |
0.081 |
|
Heart rate post-infusion (BPM) |
79.1+/-10 |
82.4+/-14.0 |
0.335 |
|
Heart rate first reading (BPM) |
78.6+/- 11.2 |
81.00+/-15.7 |
0.563 |
Table 3: The differences in blood pressure and heart rate on day 2 between the two groups.
|
Day 2 |
Conventional infusion rate |
Extended infusion rate |
P-value |
|
Systolic BP baseline (mmHg) Diastolic BP baseline (mmHg) |
118.7+/- 11.8 70.3+/- 6.8 |
121.1+/-10.5 70.0+/- 7.6 |
0.541 0.914 |
|
Systolic post infusion (mmHg) Diastolic post infusion (mmHg) |
118.7+/-18.7 70.91+/- 10.7 |
118.18+/-12.1 66.73+/-8.0 |
0.933 0.224 |
|
Systolic 1st reading (mmHg) Diastolic 1st reading (mmHg) |
119.17+/- 10.7 69.73+/- 8.0 |
122.88+/- 11.2 68.75+/-8.0 |
0.378 0.753 |
|
Baseline Heart rate (BPM) |
79.64+/- 11.2 |
83.82+/- 11.2 |
0.264 |
|
Heart rate post infusion (BPM) |
80.07+/-10.3 |
84.00+/-12.0 |
0.266 |
|
Heart rate 1st reading (BPM) |
79.18+/- 11.0 |
84.50+/-9.2 |
0.268 |
Table 4: The differences in blood pressure and heart rate on day 3 between the two groups.
|
Day 3 |
Conventional infusion rate |
Extended infusion rate |
P-value |
|
Systolic BP baseline (mmHg) Diastolic BP baseline (mmHg) |
118.55+/- 11.96 68.65+/- 8.243 |
116.10+/-8.13 69.60+/- 10.844 |
0.540 0.755 |
|
Systolic post infusion (mmHg) Diastolic post infusion (mmHg) |
121.51+/-11.84 70.15+/- 7.46 |
117.00+/-12.7 71.90+/-10.6 |
0.285 0.536 |
|
Systolic 1st reading (mmHg) Diastolic 1st reading (mmHg) |
124.66+/- 12.060 71.59+/- 9.0 |
119.63+/- 9.5 73.00+/-7.2 |
0.285 0.686 |
|
Baseline Heart rate (BPM) |
79.10+/- 10.3 |
75.22+/- 11.0 |
0.309 |
|
Heart rate post infusion (BPM) |
77.38+/-9.3 |
77.89+/-11.2 |
0.883 |
|
Heart rate 1st reading (BPM) |
75.41+/- 11.4 |
81.29+/-13.9 |
0.249 |
Table 5: The differences in blood pressure and heart rate on day 4 between the two groups.
|
Day 4 |
Conventional infusion rate |
Extended infusion rate |
P-value |
|
Systolic BP baseline (mmHg) Diastolic BP baseline (mmHg) |
121.13+/- 12.5 69.69+/- 7.9 |
121.50+/-2.4 67.25+/- 7.2 |
0.953 0.563 |
|
Systolic post-infusion (mmHg) Diastolic post infusion (mmHg) |
119.75+/-11.019 70.44+/- 7.264 |
126.75+/-2.9 72.25+/-6.7 |
0.220 0.639 |
|
Systolic 1st reading (mmHg) Diastolic 1st reading (mmHg) |
126.05+/- 9.8 73.95+/- 9.2 |
126.00+/- 7.0 72.00+/- 4.6 |
0.993 0.727 |
|
Baseline Heart rate (BPM) |
76.45+/- 11.2 |
78.25+/- 14.9 |
0.772 |
|
Heart rate post infusion (BPM) |
75.16+/-8.3 |
82.00+/-12.6 |
0.151 |
|
Heart rate 1st reading (BPM) |
73.05+/- 9.5 |
68.33+/-1.5 |
0.410 |
Table 6: The differences in blood pressure and heart rate on day 5 between the two groups.
|
Day 5 |
Conventional infusion rate |
Extended infusion rate |
P-value |
|
Systolic BP baseline (mmHg) |
121.45+/- 11.7 |
111.00+/-1.4 |
0.23 |
|
Diastolic BP baseline (mmHg) |
69.55+/- 8.6 |
64.50+/- 9.2 |
0.438 |
|
Systolic post infusion (mmHg) |
124.14+/-13.7 |
116.00+/-1.4 |
0.419 |
|
Diastolic post infusion (mmHg) |
73.36+/- 7.4 |
70.00+/-2.8 |
0.537 |
|
Systolic 1st reading (mmHg) |
128.27+/- 12.5 |
112 |
0.241 |
|
Diastolic 1st reading (mmHg) |
70.73+/- 6.9 |
74 |
0.66 |
|
Baseline Heart rate (BPM) |
74.90+/- 9.8 |
67.50+/- 6.4 |
0.314 |
|
Heart rate post-infusion (BPM) |
74.71+/-11.6 |
62.50+/-7.8 |
0.165 |
|
Heart rate 1st reading (BPM) |
75.54+/- 11.2 |
63 |
0.302 |
Table 7: The comparison of arrhythmia occurrences between the conventional and extended infusion methods.
|
Conventional |
extended |
|
|
Lowest HR post-infusion |
45 BPM |
49 BPM (baseline 52 BPM) |
|
Maximum HR post-infusion |
102 BPM |
100 BPM |
|
Maximum increasing HR |
71 BPM increased 97 (+26) |
74 BPM increased 98 (+24) |
|
Maximum decreasing HR |
82 BPM decreased 62 (-20) |
78 BPM decreased 54 (-24) |
|
Incidents of bradycardia |
5 patients 8% |
1 patient 8.3% |
Table 8: Potassium level before and after steroid pulse infusion.
|
Infusion group |
Initial potassium level |
Post infusion potassium level |
P-value |
|
Conventional group N=39 |
4.03+/- 0.26 |
4.1+/-0.3 |
0.17 |
|
Extended group N=7 |
4.16+/- 0.35 |
4.07+/-0.3 |
0.72 |
Table 9: Heart rate changing in the conventional group from day 1-3.
|
Days |
Baseline heart rate |
Post infusion heart rate |
P-value |
|
Day 1 n=60 |
75.62 ± 10.1 |
79.1±10 |
0.003 |
|
Day 2 n=54 |
75±10.3 |
79.9±10.3 |
0.013 |
|
Day 3 n=47 |
75.3±10.4 |
77.2±9.3 |
0.294 |
Table 10: Heart rate changing in the extended group from day 1-3.
|
Days |
Baseline heart rate |
Post infusion heart rate |
P-value |
|
Day 1 n=12 |
81.83± 15.314 |
82.42± 14.016 |
0.808 |
|
Day 2 n=11 |
81.82± 16.061 |
84.00± 12.058 |
0.563 |
|
Day 3 n= 9 |
81.33± 17.664 |
77.89± 11.230 |
0.322 |
Discussion
We found Pulse methylprednisolone infusion relatively safe when given over 1 hour or extended up to 6 hours. Our data showed no significant difference in vital signs readings before and after infusion among different infusion rates. At the same time, there was a change in blood pressure and heart rate readings before and after the administration of IVMP. However, this variation remains within the normal range and does not stray significantly from the baseline. Additionally, this variation has not been affected by the infusion rate. The variation in heart rate might be related to individual factors such as stress, the timing of vital sign measuring, and patient activity during the hospital stay. Eight patients out of 74 patients developed bradycardia (defined as heart rate below 60 beats per minute [9]. Among these, two patients had a baseline heart rate below 60 BPM, which increased after IVMP, while the remaining six patients developed bradycardia after receiving IVMP. Five patients (8%) were from the conventional group, and one patient (8.3%) was from the extended group. Despite this, there was no significant difference in the incidents of bradycardia between different infusion rates of IVMP. On the other hand, tachycardia (defined as heart rate above 100 BPM [8]) was documented in 8 patients (7 patients in the conventional group and one patient in the extended group) out of 74 patients. Seven out of those eight patients developed tachycardia at baseline before administration of IVMP on days 1 and 2. Only one patient in the conventional group experienced mild tachycardia following the administration of IVMP. Therefore, we believe the tachycardia occurred due to individual factors as patients were initially and persistently tachycardiac even before IVMP administration. As this is a retrospective study, only a limited number of patients completed all vital signs readings during the five days; while most patients received only three doses of IVMP during their hospital stay and completed the rest of the steroid course in outpatient settings. Hence, we conducted an additional analysis comparing the average heart rate at two time points (baseline and immediately after IVMP) from day 1 to day 3. [Table 9, 10].
Interestingly, additional analysis showed a statistically significant increase in the average heart rates among the conventional group immediately after 1st and 2nd doses despite these rates remaining within the normal range. This increase in heart rate was not accompanied by any clinical symptoms. On the other hand, there was a non-statistically significant increase in heart rate before and after IVMP in the extended infusion group which could potentially be attributed to the prolonged duration of the infusion. Yong, Kai-Ling, et al.'s study showed a significant decrease in HR at the 60 minutes following IVMP administration [4] which contradicts our additional analysis results. This might be explained by the impact of comorbidities and medications on the included subjects, in contrast to our research which focused solely on healthy individuals without underlying health conditions or medications. Generally, we found a mild increase in the mean BP after receiving IVMP, but without hypertension; the potential mechanism of such finding is sodium retention, volume expansion, and potential interference with the nitric oxide system [6]. In addition, steroids increase the sensitivity of blood vessels to vasoconstrictor hormones like catecholamines and other vasoconstrictive systems [4]. Hypokalemia is a possible side effect of IVMP, defined as a serum potassium level of less than 3.5 mEq/l. The usual range of serum potassium is 3.5 to 5 mEq/l. Out of 46 patients who underwent potassium level assessments before and 24-72 hours post IVMP administration, only one patient developed mild hypokalemia (3.4 mEq/l). In comparison with baseline, 23 patients (50%) experienced an increase in potassium levels within the normal range following IVMP administration; however, it was not statistically significant in either the conventional or extended group, with p-values of 0.17 and 0.72, respectively [Table 8]. Our study findings support the recommendation of Kai-Ling Yong El, who discouraged regular potassium checking after IVMP administration in relatively healthy patients with normal baseline potassium levels. Instead, restricting its measurement for those patients with other risk factors., such as renal failure or utilizing medications such as diuretics [4,10].
Strength and limitations
Our study included 688 vital signs (BP, HR) measurements related to 277 infusions administered. The main limitation of our study was the small number of study subjects in the extended group; in addition, there was variability in the length of stay and the frequency of monitoring.
Conclusion
IVMP is relatively safe and effective in treating MS exacerbation regardless of intravenous infusion duration, whether administered over a shorter or longer period. There was no significant difference in vital signs fluctuation between different infusion rates. Moreover, there was a statistically significant increase in the mean heart rate in the conventional group immediately after the first and second but not the third dose of IVMP compared to baseline. Additionally, the absence of significant changes in potassium levels before and after IVMP administration suggests that routine potassium monitoring might not be necessary for all patients receiving this treatment.
Acknowledgments
Not applicable.
Statement of Ethics
This study protocol was approved by the Institutional Review Board (IRB) of Hamad Medical Corporation (MRC number: 01-18-024, Email: irb@hamad.qa Tel: 00974-40256410, HMC-IRB Registration: MOPH-HMC-020, IRB-MoPH Assurance: IRB-A-HMC-2019-0014), and is therefore carried out per all the relevant sections of the Rules and Regulations for Research at HMC and with the 1964 Helsinki declaration ethical standards. Furthermore, all methods were conducted in accordance with appropriate guidelines and regulations. As it is a retrospective study, the need for informed consent was waived.
Conflict of interest
The authors declare that they have no conflicts of interest.
Consent for publication
Not applicable.
Data Statement and Author Contributions
Haider Alabd conceived the research idea. Haider Alabd and Mohamed Elshafei designed the initial study protocol submitted to MRC. Prem Chandra is responsible for the statistical design and analysis. Haider Alabd and Mohamed Elshafei have done data collection. Haider Alabd, Lolwa Barakat, Bhagya Sree, and Mohamed Khalil wrote the manuscript. Haider Alabd, Lolwa Barakat, Bhagya Sree, Prem Chandra, Mohamed Khalil, and Mohamed Elshafei critically reviewed the initial draft and approved the final version for publication.
The data supporting this study's findings are available from Hamad Medical Corporation. Still, restrictions apply to the availability of these data, which are used under license for the current research and are not publicly available. However, data are available from the authors upon reasonable request and with the permission of Hamad Medical Corporation.
References
- Sevim S. Relapses in Multiple Sclerosis: Definition, Pathophysiology, Features, Imitators, and Treatment. Turkish Journal of Neurology/Turk Noroloji Dergisi 22 (2016).
- http://online.lexi.com/lco/action/doc/retrieve/docid/multinat_f/4669835?cesid=7WS8FnH6gQ3&searchUrl=%2Flco%2Faction
%2Fsearch%3Fq%3DmethylPREDNISolone%26t%3Dname%26va%3DmethylPREDNISolone# - Heidrich E, Greene G, Weberding J, et al. Effects of methylprednisolone infusions on vital signs in children with headaches. The Journal of Pediatric Pharmacology and Therapeutics 18 (2013): 39-44.
- Yong KL, Chng CL, Htoon HM, et al. Safety profile and effects of pulsed Methylprednisolone on vital signs in thyroid eye disease. International Journal of Endocrinology (2015).
- Kelly JJ, Mangos G, Williamson PM, et al. Cortisol and hypertension. Clinical and Experimental Pharmacology and Physiology 25 (1998): S51-6.
- McLuckie LA, Savage CR. Atrial fibrillation following pulse methylprednisolone therapy in an adult. Chest 104 (1993): 622-623.
- Van Den Berg JS, Hommes OV, Wuis EW, et al. Anaphylactoid reaction to intravenous Methylprednisolone in a patient with multiple sclerosis. Journal of Neurology, Neurosurgery & Psychiatry 63 (1997): 813-814.
- Page RL, Joglar JA, Caldwell MA, et al. 2015 ACC/AHA/HRS guideline for the management of adult patients with supraventricular tachycardia: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. Journal of the American College of Cardiology 67 (2016): e27-115.
- Spodick DH. Normal sinus heart rate: sinus tachycardia and sinus bradycardia redefined. American heart journal 124 (1992): 1119-1121.
- Bonnotte B, Chauffert B, Martin F, et al. Side-effects of high-dose intravenous (pulse) methylprednisolone therapy cured by potassium infusion. British journal of rheumatology 37 (1998): 109.
