Safety and Efficacy of Oral and Parenteral Ibuprofen for Closure of Patent Ductus Arteriosus in Very Low Birth weight Asian Neonates - A retrospective Audit
Article Information
Badillo MC1,6 , Abdul Alim AA2,4,5,6 , Chandran S2,4,5,6*, Saffari SE3, Rajadurai VS2,4,5,6
1Staff Registrar, Department of Neonatology, KK Women's and Children's Hospital, Singapore
2Senior Consultant, Department of Neonatology, KK Women's and Children's Hospital, Singapore
3Center for Quantitative Medicine, Duke NUS Medical School, Singapore
4Duke-NUS Medical School, Singapore
5NUS Yong Loo Lin School of Medicine, Singapore
6NTU Lee Kong Chian School of Medicine, Singapore
*Corresponding Author: Suresh Chandran, Senior Consultant, Department of Neonatology, KK Women’s and Children’s Hospital, 100 Bukit Timah Road, Singapore, DID: 65 63941985; HP: 65 91799244;
Received: 02 January 2021; Accepted: 19 January 2021; Published: 29 January 2021
Citation: Badillo MC, Abdul Haium AA, Chandran S, Saffari SE, Rajadurai VS. Safety and Efficacy of Oral and Parenteral Ibuprofen for Closure of Patent Ductus Arteriosus in Very Low Birth weight Asian Neonates - A retrospective Audit. Archives of Clinical and Medical Case Reports 5 (2021): 182-192.
View / Download Pdf Share at FacebookAbstract
Introduction: Patent ductus arteriosus (PDA) is common in preterm neonates. Indomethacin and ibuprofen are commonly used for medical closure of patent ductus arteriosus. This study aims to evaluate the safety and efficacy of ibuprofen for treatment of PDA in very low birth weight (VLBW) infants.
Methods: A retrospective audit of VLBW infants who received ibuprofen for treatment of PDA in a single centre between March 2010 and December 2014 was conducted. Infants with hemodynamically significant PDA were treated with intravenous or oral ibuprofen after echocardiographic evaluation. Response to treatment was documented with follow up echocardiography. The baseline patient characteristics, the ductal closure rate, adverse effects and need for PDA ligation were analysed.
Results: Total of 138 VLBW infants received ibuprofen. 108 infants with birth weight ranging from 430-1500g received intravenous ibuprofen (group 1) and 30 infants with birth weight ranging from 661-1483g received oral ibuprofen (group 2). The closure rate of PDA was 50.9% (55/108) in-group 1 and 43.3% (13/30) in-group 2. Necrotizing enterocolitis or spontaneous intestinal perforation was observed in 11.1% (12/108) of group 1 and 10% (3/30) of group 2 infants. PDA ligation rate was 20.4% (22/108) in-group 1 and 6.7% (2/30) in-group 2.
Conclusion: The closure rate of PDA following intravenous ibuprofen was 50.9% in VLBW infants. Serious gastrointestinal adverse effects occurred in 10-11% of infants treated with ibuprofen. Relatively lower closure rates and serious gastrointestinal adverse effects should be considered when treatment decisions are made for closure of PDA with ibuprofen.
Keywords
Very low birth weight infant; Patent ductus arteriosus; Ibuprofen; Spontaneous intestinal perforation; Necrotizing enterocolitis
Very low birth weight infant articles; Patent ductus arteriosus articles; Ibuprofen articles; Spontaneous intestinal perforation articles; Necrotizing enterocolitis articles
Very low birth weight infant articles Very low birth weight infant Research articles Very low birth weight infant review articles Very low birth weight infant PubMed articles Very low birth weight infant PubMed Central articles Very low birth weight infant 2023 articles Very low birth weight infant 2024 articles Very low birth weight infant Scopus articles Very low birth weight infant impact factor journals Very low birth weight infant Scopus journals Very low birth weight infant PubMed journals Very low birth weight infant medical journals Very low birth weight infant free journals Very low birth weight infant best journals Very low birth weight infant top journals Very low birth weight infant free medical journals Very low birth weight infant famous journals Very low birth weight infant Google Scholar indexed journals Patent ductus arteriosus articles Patent ductus arteriosus Research articles Patent ductus arteriosus review articles Patent ductus arteriosus PubMed articles Patent ductus arteriosus PubMed Central articles Patent ductus arteriosus 2023 articles Patent ductus arteriosus 2024 articles Patent ductus arteriosus Scopus articles Patent ductus arteriosus impact factor journals Patent ductus arteriosus Scopus journals Patent ductus arteriosus PubMed journals Patent ductus arteriosus medical journals Patent ductus arteriosus free journals Patent ductus arteriosus best journals Patent ductus arteriosus top journals Patent ductus arteriosus free medical journals Patent ductus arteriosus famous journals Patent ductus arteriosus Google Scholar indexed journals Ibuprofen articles Ibuprofen Research articles Ibuprofen review articles Ibuprofen PubMed articles Ibuprofen PubMed Central articles Ibuprofen 2023 articles Ibuprofen 2024 articles Ibuprofen Scopus articles Ibuprofen impact factor journals Ibuprofen Scopus journals Ibuprofen PubMed journals Ibuprofen medical journals Ibuprofen free journals Ibuprofen best journals Ibuprofen top journals Ibuprofen free medical journals Ibuprofen famous journals Ibuprofen Google Scholar indexed journals Spontaneous intestinal perforation articles Spontaneous intestinal perforation Research articles Spontaneous intestinal perforation review articles Spontaneous intestinal perforation PubMed articles Spontaneous intestinal perforation PubMed Central articles Spontaneous intestinal perforation 2023 articles Spontaneous intestinal perforation 2024 articles Spontaneous intestinal perforation Scopus articles Spontaneous intestinal perforation impact factor journals Spontaneous intestinal perforation Scopus journals Spontaneous intestinal perforation PubMed journals Spontaneous intestinal perforation medical journals Spontaneous intestinal perforation free journals Spontaneous intestinal perforation best journals Spontaneous intestinal perforation top journals Spontaneous intestinal perforation free medical journals Spontaneous intestinal perforation famous journals Spontaneous intestinal perforation Google Scholar indexed journals Case report articles Case report Research articles Case report review articles Case report PubMed articles Case report PubMed Central articles Case report 2023 articles Case report 2024 articles Case report Scopus articles Case report impact factor journals Case report Scopus journals Case report PubMed journals Case report medical journals Case report free journals Case report best journals Case report top journals Case report free medical journals Case report famous journals Case report Google Scholar indexed journals treatment articles treatment Research articles treatment review articles treatment PubMed articles treatment PubMed Central articles treatment 2023 articles treatment 2024 articles treatment Scopus articles treatment impact factor journals treatment Scopus journals treatment PubMed journals treatment medical journals treatment free journals treatment best journals treatment top journals treatment free medical journals treatment famous journals treatment Google Scholar indexed journals CT articles CT Research articles CT review articles CT PubMed articles CT PubMed Central articles CT 2023 articles CT 2024 articles CT Scopus articles CT impact factor journals CT Scopus journals CT PubMed journals CT medical journals CT free journals CT best journals CT top journals CT free medical journals CT famous journals CT Google Scholar indexed journals surgery articles surgery Research articles surgery review articles surgery PubMed articles surgery PubMed Central articles surgery 2023 articles surgery 2024 articles surgery Scopus articles surgery impact factor journals surgery Scopus journals surgery PubMed journals surgery medical journals surgery free journals surgery best journals surgery top journals surgery free medical journals surgery famous journals surgery Google Scholar indexed journals Pathogenesis articles Pathogenesis Research articles Pathogenesis review articles Pathogenesis PubMed articles Pathogenesis PubMed Central articles Pathogenesis 2023 articles Pathogenesis 2024 articles Pathogenesis Scopus articles Pathogenesis impact factor journals Pathogenesis Scopus journals Pathogenesis PubMed journals Pathogenesis medical journals Pathogenesis free journals Pathogenesis best journals Pathogenesis top journals Pathogenesis free medical journals Pathogenesis famous journals Pathogenesis Google Scholar indexed journals Necrotizing enterocolitis articles Necrotizing enterocolitis Research articles Necrotizing enterocolitis review articles Necrotizing enterocolitis PubMed articles Necrotizing enterocolitis PubMed Central articles Necrotizing enterocolitis 2023 articles Necrotizing enterocolitis 2024 articles Necrotizing enterocolitis Scopus articles Necrotizing enterocolitis impact factor journals Necrotizing enterocolitis Scopus journals Necrotizing enterocolitis PubMed journals Necrotizing enterocolitis medical journals Necrotizing enterocolitis free journals Necrotizing enterocolitis best journals Necrotizing enterocolitis top journals Necrotizing enterocolitis free medical journals Necrotizing enterocolitis famous journals Necrotizing enterocolitis Google Scholar indexed journals
Article Details
1. Introduction
Patent ductus arteriosus (PDA) is a common cardiovascular condition in preterm infants. Ductus arteriosus (DA) remains patent in 70% of infants born <28 weeks’ gestation and 80% of infants born at 24-25 weeks’ gestation [1-3]. Haemodynamically significant PDA (hsPDA) in preterm neonates has been shown to be associated with several neonatal morbidities such as bronchopulmonary dysplasia (BPD), necrotizing enterocolitis (NEC), intraventricular haemorrhage (IVH) and mortality. However routine treatment of PDA neither failed to show significant reduction in these morbidities nor offer any long-term benefits [2, 4]. Treatment options for hsPDA in preterm infants include conservative management with expectant spontaneous closure, pharmacologic treatment aiming at ductal constriction/closure and surgical ligation. Targeted early treatment of symptomatic PDA is still being practiced by many clinicians, as studies have shown that this offers short term benefits such as reduction in pulmonary haemorrhage, improvement in respiratory status and weight gain [5] Indomethacin and ibuprofen are the only licenced medications for PDA closure in preterm infants. In recent times, paracetamol has also been used for ductal closure with variable success rate [6].
Indomethacin and ibuprofen both inhibit prostaglandin synthesis. Indomethacin is the most studied pharmacologic agent for the treatment of PDA and has been shown to be effective in up to 70% of the cases [7, 8]. Ibuprofen has been shown to be as effective as indomethacin with similar closure rates and fewer renal side effects [9]. The choice of pharmacologic agent varies across units and is guided by the local experience, availability of the drug and cost of treatment. In our unit, we were using intravenous indomethacin as the first line drug for ductal closure. We switched to ibuprofen in the year 2010 due to non-availability of indomethacin. While on ibuprofen, we noticed an increased incidence of gastrointestinal (GI) side effects such as GI bleed and necrotising enterocolitis temporally associated with ibuprofen therapy. This prompted us to undertake this audit to determine the safety and efficacy and the incidence of adverse effects of ibuprofen for treatment of PDA in VLBW infants.
2. Material and Methods
This retrospective audit was conducted in a single centre tertiary neonatal unit at KK Women’s and Children’s Hospital, Singapore. VLBW infants born at 23 - 33 weeks’ gestation and birth weight of 430 - 1500g who received any form of ibuprofen, either intravenous or oral during the study period (March 2010 to December 2014) were included in this audit. Infants with pre-existing renal failure (creatinine >100µmol/L), significant thrombocytopenia (platelet count <100,000/µL), complex congenital cardiac defects and grade IV intraventricular haemorrhage (IVH) did not receive ibuprofen and hence were not included in this audit. All infants who received ibuprofen had hsPDA based on clinical evaluation and echocardiographic assessment. The criteria used to define hsPDA during the study period were pragmatic. Requirement for mechanical ventilation, hypotension, blood stained endotracheal aspirate and cardiomegaly/pulmonary congestion on chest x-ray are considered as significant clinical features of hsPDA. The echocardiographic features of hsPDA considered include ductal diameter of >1.5mm and left atrial and/or left ventricular dilatation [10]. The echocardiographic assessments were performed by trained paediatric echocardiographers and reported by paediatric cardiologists. During the study period unit’s fluid management and feeding practice remain unchanged.
During the study period, Ibuprofen was the only medication used for medical treatment of PDA. The choice of intravenous or oral route of administration was made mainly based on infant’s birth weight, clinical status and feed tolerance. Intravenous ibuprofen (Ibuprofen THAM, Pedea 5mg/ml, Orphan Europe, Paris, France) was preferred for smaller infants with birth weight <1000g and those infants with birth weight >1000 g but on minimal or no enteral feeds. Oral Ibuprofen (Ibuprofen 100 mg/5ml, Bifen, Drug House of Australia) was preferred for infants with birth weight more than 1000 g; however some infants with birth weight <1000 g, who are tolerating at least 60 ml/kg/day of enteral feeds were also given oral ibuprofen based on attending neonatologist’s discretion. The dose of intravenous and oral ibuprofen was the same for all infants: Initial dose of 10 mg/kg followed by 2 doses of 5 mg/kg, given 24 hours apart (total of 3 doses).
A follow-up echocardiogram was performed within 3 days of completion of treatment. A second course of ibuprofen was given to a subset of symptomatic infants with persistent hsPDA after the first course, confirmed by echocardiography. Repeat course of ibuprofen was not given for infants who had GI/renal adverse events following the first course. PDA ligation was performed for selected cases of symptomatic hsPDA following failure of medical closure or in infants who have contraindication for medical therapy. Antenatal, perinatal risk factors and demographic features of infants who received ibuprofen were obtained from the neonatal database. Time of treatment, post treatment echocardiographic findings and complications of medical therapy were obtained from hospital electronic medical records. Post treatment GI complications including NEC (Bell’s Stage ≥II), spontaneous intestinal perforation (SIP), and significant gastric aspirates (bile or blood, fresh and altered) were documented. Biochemical and haematological changes including hyponatraemia (<130 mmol/L), raised blood urea nitrogen (BUN) (>10 mmol/L), raised creatinine (>100 µmol/L) and new onset of thrombocytopenia (<150,000/µL) up to 3 days post treatment were collected. Approval for this study was obtained from the Centralized Institutional Review Board (CIRB 2016/2106), Singapore.
2.1 Statistical methods
Infant and maternal characteristics, gastrointestinal effects, biochemical, hematologic and drug-related complications were reported using mean ± standard deviation and frequency as percentage for continuous and categorical variables, respectively. Complications were presented as frequency and percentage. Statistical analysis was performed using SAS version 9.4 for Windows (SAS Institute Inc., Cary, NC, USA).
3. Results
Out of 981 VLBW infants born during the study period, 138 (14%) infants with hsPDA received treatment with ibuprofen. 108 (78%) infants received intravenous and 30 (22%) infants received oral ibuprofen. The infants who received intravenous ibuprofen were of lower birth weight and lower gestation due to treatment selection criteria. Majority of the infants (n=101, 94%) who received intravenous ibuprofen are of birth weight <1000g, however there were 7 (6%) infants with birth weight 1000-1500g in the intravenous group. Out of 30 infants who received oral ibuprofen, 11 (37%) were in birth weight <1000g and 19 (63%) in birth weight 1000-1500g groups. A second course of ibuprofen was given to 14 infants in intravenous group and 4 infants in the oral group (Figure 1). The baseline characteristics of the infants who received ibuprofen are given in Table 1. Marginally higher number of infants in the intravenous ibuprofen group (n = 93, 86.1%) required surfactant, which could related to lower gestation and birth weight in this group. Mode of maximum ventilatory support required was not different between the groups (Table 1).
The closure rate of PDA following intravenous ibuprofen was 50.9% (39.8% after first course and additional 11.1% after second course). The closure rate of PDA following oral ibuprofen was 43.3% (30% after first course and additional 13.3% after second course) (Figure 1). PDA ligation rate showed an increasing trend in the smaller infants, 20.3% in birth weight <1000g compared to 6.7% in infants of birth weight 1000-1500g. The commonly observed adverse effects were listed in Table 2. Renal and electrolyte abnormalities were observed both with intravenous and oral treatment. There was a tendency for higher rates of hyponatraemia (36.7% vs. 25%) in the oral ibuprofen group compared to the intravenous group. Raised BUN and raised creatinine was more commonly observed in the smaller infants treated with intravenous ibuprofen. Thrombocytopenia was observed in 59.3% of the infants treated with intravenous ibuprofen (Table 2).
The commonly observed GI adverse effects include GI bleeding indicated by blood stained or brownish aspirates, bile stained aspirates and NEC/SIP. GI bleeding was observed in 18.5% of infants in intravenous group and 10% of infants in the oral group. NEC (Bell’s stage ≥II) occurred in 9 (8.3%) infants in the intravenous and 3 (10%) infants in the oral ibuprofen group. Spontaneous intestinal perforation was noted in 3 (2.8%) infants in the intravenous group. The median time interval between the last dose of ibuprofen and onset of NEC symptoms were 3 days in the intravenous and 7 days in the oral ibuprofen groups. Three infants who developed NEC in intravenous ibuprofen group (33.3%) and 1 infant in oral ibuprofen group (33.3%) have died. All infants who had SIP had recovered following surgical treatment (Table 3).
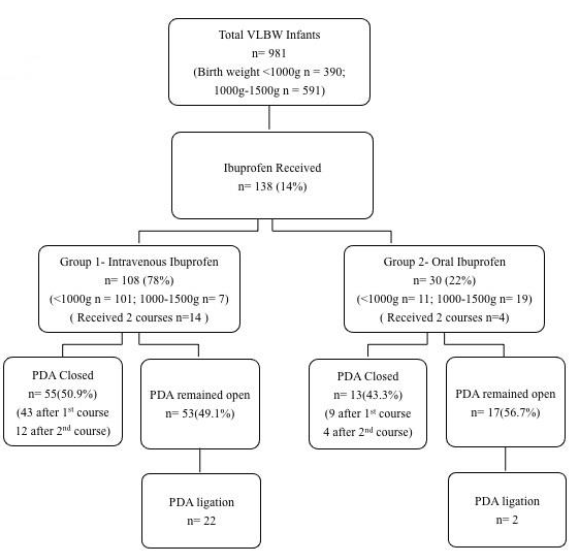
Figure 1: Flow diagram of eligible very low birth weight (VLBW) infants included in the study. Closure rate of patent ductus arteriosus (PDA) between oral and intravenous ibuprofen groups among VLBW Infants.
|
Parameters |
Intravenous N = 108 |
Oral N = 30 |
|
Gestational age, week (mean ± SD) |
26.1 ± 1.8 |
27.9 ± 2.2 |
|
Birth weight in grams, median (range) |
818 (430-1500) |
1074 (661-1483) |
|
Male sex, frequency (%) |
47 (43.5) |
12 (40) |
|
Ethnicity, frequency (%) |
||
|
Chinese |
66 (61.1) |
24 (80) |
|
Malay |
21 (19.4) |
4 (13.3) |
|
Indian |
7 (6.5) |
0 (0) |
|
Others |
14 (13) |
2 (6.7) |
|
Caesarean Delivery, frequency (%) |
71 (65.7) |
19 (63.3) |
|
Received Surfactant, frequency (%) |
93 (86.1) |
21 (70) |
|
Maximum Ventilatory support, frequency (%) |
||
|
CPAP |
6 (5.6) |
4 (13.3) |
|
IPPV |
71 (65.7) |
23 (76.7) |
|
HFOV |
31 (28.7) |
3 (10) |
|
Maternal Diabetes, frequency (%) |
5 (4.6) |
7 (23.3) |
|
Maternal PIH, frequency (%) |
23 (16.7) |
7 (23.3) |
|
Maternal Chorioamnionitis, frequency (%) |
45 (32.6) |
9 (30) |
|
Antenatal dexamethasone, frequency (%) |
||
|
1 dose |
15 (13.9) |
4 (13.3) |
|
2 doses |
77 (71.3) |
20 (66.7) |
|
None |
16 (14.8) |
6 (20) |
CPAP=Continuous positive pressure ventilation; IPPV=Itermittent positive pressure ventilation; HFOV=High frequency oscillatory ventilation; PIH=Pregnancy induced hypertension
Table 1: Infant perinatal characteristics.
|
Adverse Effects |
Intravenous n = 108 (%) |
Oral n = 30 (%) |
|
NEC Stage II and above or SIP |
12 (11.1) |
3 (10) |
|
NEC Stage II |
9 (8.3) |
3 (10) |
|
SIP |
3 (2.8) |
0 (0) |
|
GI Bleed |
20 (18.5) |
3 (10) |
|
Bilious aspirates |
3 (2.8) |
1 (3.3) |
|
Hyponatremia |
27 (25) |
11 (36.7) |
|
Raised BUN |
19 (17.6) |
4 (13.3) |
|
Raised Creatinine |
5 (4.6) |
0 (0) |
|
Thrombocytopenia |
64 (59.3) |
3 (10) |
NEC = Necrotizing enterocolitis; SIP = Spontaneous intestinal perforation; GI = Gastrointestinal; BUN = Blood urea nitrogen
Table 2: Complications of oral and intravenous ibuprofen treatment.
|
No |
Gestation (weeks), Birth weight (gm) |
Ibuprofen Route |
Diagnosis |
Time interval of ibuprofen completion and symptoms (days) |
Outcome |
|
1 |
26+0, 998 |
IV |
SIP |
4 |
A |
|
2 |
25+4, 810 |
IV |
SIP |
1 |
A |
|
3 |
28+3, 1115 |
IV |
SIP |
3 |
A |
|
4 |
24+6, 736 |
IV |
NEC, Stage 3 |
40 |
A |
|
5 |
24+6, 893 |
IV |
NEC, Stage 2B |
4 |
A |
|
6 |
25+0, 652 |
IV |
NEC, Stage 3 |
35 |
D |
|
7 |
25+0, 810 |
IV |
NEC, Stage 3 |
2 |
A |
|
8 |
26+1, 998 |
IV |
NEC, Stage 3 |
1 |
A |
|
9 |
26+0, 835 |
IV |
NEC, Stage 3 |
7 |
D |
|
10 |
26+4, 1116 |
IV |
NEC, Stage 2A |
3 |
D |
|
11 |
23+6, 624 |
IV |
NEC, Stage 3 |
2 |
A |
|
12 |
23+6, 634 |
IV |
NEC, Stage 3 |
3 |
A |
|
13 |
29+5, 1440 |
Oral |
NEC, Stage 3 |
6 |
A |
|
14 |
27+0, 956 |
Oral |
NEC, Stage 3 |
7 |
D |
|
15 |
30+4, 1289 |
Oral |
NEC, Stage 2B |
26 |
A |
NEC= Necrotizing enterocolitis; SIP=Spontaneous intestinal perforation; IV=Intravenous; A=Alive; D=Death
Table 3: Gastrointestinal adverse effects of intravenous and oral ibuprofen and outcome.
4. Discussion
In fetal life, DA shunts blood exclusively right-to-left to deliver oxygenated blood from placenta to the fetus [4]. Ductus arteriosus constricts within 24-48 hours of birth in most term infants causing a functional closure followed by anatomic remodelling. However, spontaneous closure of DA occurs only in about 34% of infants with birth weight of <1000g and 67% in infants of birth weight 1000-1500g by day 7 [11]. Spontaneous closure occurs at later gestations as well. Herman et al. has shown that all VLBW infants who had PDA at discharge from hospital had spontaneous closure at a median corrected age of 48 weeks [12]. Haemodynamically significant PDA in VLBW infants affect mortality as well as comorbidities like NEC, BPD, IVH and long-term neurodevelopmental outcome [13]. However, recent studies question the causal relationship between PDA and adverse neonatal outcomes resulting in wide variations in the management of PDA across the neonatal fraternity [1].
Recently there is a trend towards a more tolerant approach to PDA. However, many neonatologists believe that there are still a selected group of preterm infants, who will benefit from PDA closure. Consequently, targeted treatment of high- risk infants is still being practiced in many units [14]. The choice of pharmacologic agent for the treatment of PDA is also an area of research interest. Indomethacin being the most studied drug is still favoured by many neonatologists. In our unit this was the preferred medication used for medical closure of PDA. In March 2010 our unit switched from indomethacin to ibuprofen as indomethacin became unavailable. An increasing number of cases NEC and SIP were observed after introduction of intravenous ibuprofen, which prompted this audit.
Two intravenous formulations of ibuprofen are used for treatment of PDA, ibuprofen-lysine and ibuprofen-THAM. Ibuprofen-THAM showed increased closure rate of PDA, reducing the need for surgical ligation but at the cost of higher incidence of NEC [15]. Clinical studies and meta-analysis showed that ibuprofen is as effective as indomethacin in closing PDA, with lower risk of NEC and transient renal insufficiency [9, 16, 17]. With regards to the route of administration, some studies have shown better closure rates of PDA with oral ibuprofen than IV ibuprofen [18, 19]. In separate studies done by Cherif et al. and Heyman et al., oral ibuprofen was shown to be effective and well tolerated for early closure of PDA in very premature infants [20, 21]. Intravenous ibuprofen is more expensive and not readily available, hence oral preparation is used more often especially in resource-limited settings. In a study by Gokmen et al., oral ibuprofen was found to be more effective for closure of PDA with one course of treatment. The major intestinal concerns about the oral route were GI bleeding [18]. Richard et al. demonstrated that PDA closure is gestation dependent, with a cumulative closure rate of 65% [22]. The closure rates of ibuprofen have been reported to be as high as 70% in published studies [23].
In our study we have found that the overall effectiveness of ibuprofen in closing the PDA is less than that published elsewhere. Only 50.9% of PDA’s in VLBW infants closed after intravenous ibuprofen and 43.3% with oral ibuprofen. The lower closure rates could be related to selective treatment of PDA and treatment criteria used and preferential treatment of symptomatic infants in the lower gestational age group. In our unit, during the study period only a selected subgroup of symptomatic infants with persistent PDA after the 1st course of ibuprofen was given the 2nd course based on clinical and echocardiographic parameters. This could be the likely reason for the additional closure rate after the second course of oral ibuprofen in our study. We have noticed significant GI complications associated with both intravenous as well as oral ibuprofen use. A randomized, double-blind, placebo-controlled study by Gournay et al. with prophylactic ibuprofen for efficacy and safety was stopped prematurely due to severe pulmonary hypertension in 3 of 65 infants born less than 28 weeks of gestation. Above all, in that study, survival was not improved with intravenous ibuprofen-THAM due to higher incidence of digestive, respiratory and renal adverse effects [15]. We also used IV ibuprofen-THAM in our cohort but the incidence of NEC was not different from the bigger babies in the oral group but SIP was noted only in infants treated with intravenous ibuprofen. Pulmonary hypertension was not observed either in our oral or intravenous ibuprofen treated infants.
Hyperosmolality of preterm milk feeds with added medications and supplements has a potential to cause feed intolerance and even NEC [21]. This has led American Academy of Pediatrics to recommend an osmolality of less than 450 mOsm/kg for enteral feeds of preterm infants at-risk of NEC [21, 22]. We have studied the neat osmolality of common oral medications and supplements used in preterm infants and found the optimal dilution ratio with diluents such as water, breast milk, breast milk with fortifier and preterm formula, to achieve an osmolality of < 450 mOsm/kg [24]. Neat osmolality of ibuprofen syrup used in our unit was >2000 mOsm/kg and since 2016 we have been using appropriate dilution ratio to optimize the osmolality with no further cases of NEC observed following oral ibuprofen therapy [25]. Kushnir et al. reported an overall similar effect on renal function with repeated courses of therapy with ibuprofen and indomethacin [26]. In our cohort, renal impairment during ibuprofen therapy showed an increasing trend with higher creatinine and raised BUN in smaller infants treated with intravenous ibuprofen than in larger infants in the oral group. In addition, we have also noticed significantly higher number of infants treated with intravenous ibuprofen developing thrombocytopenia, which has not been reported in previous studies with ibuprofen [27]. This could be due to the smaller and more immature neonates in the intravenous group and needs further evaluation in any future studies.
5. Conclusions
Intravenous ibuprofen has an overall 50.9% success rate in closing the PDA in our VLBW population, less than the 70% published in the literature [23]. Serious GI complications were observed in up to 11% of VLBW infants treated with intravenous ibuprofen in our cohort. Even though ibuprofen had been described as an effective drug in closing the PDA, the closure rate could be as low as 50% and with significant GI side effects especially in smaller infants treated with intravenous ibuprofen. Hence, the use of ibuprofen should be carefully considered if PDA treatment is contemplated in VLBW population and treatment alternatives including conservative treatment should be considered where appropriate. Parents should also be counselled regarding the possible adverse effects. We also feel that there is still justification for more randomized control trials comparing ibuprofen treatment with placebo and looking at outcome measures including ductal closure rates, adverse effects and long-term outcomes.
Acknowledgements
We would like to thank late A/Prof. M Gomez Joseph, Senior Consultant, Department of Neonatology, KK Women’s and Children’s Hospital, Singapore for initiating this research work and guiding through the preparation of proforma and collection of data and Prof. Divakaran Liginlal of Carnegie Mellon University, Pittsburgh, P.A., USA, for editing the manuscript.
Declarations
Conflict of interest: None declared.
Financial disclosures: None declared.
References
- Heuchan AM, Clyman RI. Managing the patent ductus arteriosus: current treatment options. Archives of Disease in Childhood-Fetal and Neonatal Edition 9 (2014): F431-F436.
- Rolland A, Shankar-Aguilera S, Diomandé D, et al. Natural evolution of patent ductus arteriosus in the extremely preterm infant. Archives of Disease in Childhood-Fetal and Neonatal Edition 100 (2015): F55-F58.
- Van Overmeire B, Chemtob S. The pharmacologic closure of the patent ductus arteriosus. Semin Fetal Neonatal Med 10 (2005): 177-184.
- Evans N, Archer L. Postnatal circulatory adaptation in healthy term and preterm neonates. Archives of disease in childhood 65 (1990): 24-26.
- Kluckow M, Jeffery M, Gill A, et al. A randomised placebo-controlled trial of early treatment of the patent ductus arteriosus. Archives of Disease in Childhood-Fetal and Neonatal Edition 99 (2014): F99-F104.
- Ohlsson A, Walia R, Shah SS. Ibuprofen for the treatment of patent ductus arteriosus in preterm or low birth weight (or both) infants. Cochrane Database Syst Rev 9 (2018): CD003481.
- Gersony WM, Peckham GJ, Ellison RC, et al. Effects of indomethacin in premature infants with patent ductus arteriosus: results of a national collaborative study. The Journal of pediatrics 102 (1983): 895-906.
- Evans N. Current controversies in the diagnosis and treatment of patent ductus arteriosus in preterm infants. Advances in Neonatal Care 3 (2003): 168-177.
- Van Overmeire B, Smets K, Lecoutere D, et al. A comparison of ibuprofen and indomethacin for closure of patent ductus arteriosus. New England Journal of Medicine 343 (2000): 674-681.
- Zonnenberg I, de Waal K. The definition of a haemodynamic significant duct in randomized controlled trials: a systematic literature review. Acta paediatrica 101 (2012): 247-251.
- Clyman RI, Couto J, Murphy GM. Patent Ductus Arteriosus: Are Current Neonatal Treatment Options Better or Worse Than No Treatment at All? Seminars in perinatology 36 (2012): 123-129.
- Herrman K, Bose C, Lewis K, et al. Spontaneous closure of the patent ductus arteriosus in very low birth weight infants following discharge from the neonatal unit. Archives of Disease in Childhood-Fetal and Neonatal Edition 94 (2009): F48-F50.
- Schmidt B, Davis P, Moddemann D, et al. Long-term effects of indomethacin prophylaxis in extremely-low-birth-weight infants. New England Journal of Medicine 344 (2001): 1966-1972.
- Wyllie JP, Gupta S. Prophylactic and early targeted treatment of patent ductus arteriosus. Semin Fetal Neonatal Med 23 (2018): 250-254.
- Gournay V, Roze J, Kuster A, et al. Prophylactic ibuprofen versus placebo in very premature infants: a randomised, double-blind, placebo-controlled trial. The Lancet 364 (2004): 1939-1944.
- Gulack BC, Laughon MM, Clark RH, et al. Comparative effectiveness and safety of indomethacin versus ibuprofen for the treatment of patent ductus arteriosus. Early human development 91 (2015): 725-729.
- Ohlsson A, Walia R, Shah SS. Ibuprofen for the treatment of patent ductus arteriosus in preterm or low birth weight (or both) infants. Cochrane Database Syst Rev 2 (2020): CD003481.
- Gokmen T, Erdeve O, Altug N, et al. Efficacy and Safety of Oral Versus Intravenous Ibuprofen in Very Low Birth Weight Preterm Infants with Patent Ductus Arteriosus. J Pediatr 158 (2011): 549-U45.
- Mitra S, Florez ID, Tamayo ME, et al. Association of placebo, indomethacin, ibuprofen, and acetaminophen with closure of hemodynamically significant patent ductus arteriosus in preterm infants: a systematic review and meta-analysis. Jama 319 (2018): 1221-1238.
- Cherif A, Jabnoun S, Khrouf N. Oral ibuprofen in early curative closure of patent ductus arteriosus in very premature infants. American journal of perinatology 24 (2007): 339-345.
- Heyman E, Morag I, Batash D, et al. Closure of patent ductus arteriosus with oral ibuprofen suspension in premature newborns: a pilot study. Pediatrics 112 (2003):e354.
- Richards J, Johnson A, Fox G, et al. A second course of ibuprofen is effective in the closure of a clinically significant PDA in ELBW infants. Pediatrics 124 (2009): e287-e293.
- Aranda J, Thomas R. Systematic review: intravenous ibuprofen in preterm newborns. Semin Perinatol 30 (2006): 114-120.
- Chandran S, Chua MC, Lin W, et al. Medications that increase osmolality and compromise the safety of enteral feeding in preterm infants. Neonatology 111 (2017): 309-316.
- Chandran S, Anand AJ, Rajadurai VS, et al. Evidence-Based Practices Reduce Necrotizing Enterocolitis and Improve Nutrition Outcomes in Very Low-Birth-Weight Infants. JPEN J Parenter Enteral Nutr (2020).
- Kushnir A, Pinheiro JM. Comparison of renal effects of ibuprofen versus indomethacin during treatment of patent ductus arteriosus in contiguous historical cohorts. BMC clinical pharmacology 11 (2011): 8.
- Dani C, Bertini G, Pezzati M, et al. Prophylactic Ibuprofen for the Prevention of Intraventricular Hemorrhage Among Preterm Infants: A Multicenter, Randomized Study. Pediatrics 115 (2005): 1529-1535.
