Sacral Chordoma: Don’t throw away the Scalpel
Article Information
Aadit Shah*, Ryan P Tantone, Matthew Berchuck
Department of Orthopaedic Surgery, Renaissance School of Medicine, Stony Brook University, Stony Brook, USA
*Corresponding Author: Aadit Shah, Department of Orthopaedic Surgery, Renaissance School of Medicine, Stony Brook University, 101 Nicolls Rd, HSC T-18 – 089, Stony Brook 11794, USA
Received: 20 April 2021; Accepted: 30 April 2021; Published: 03 May 2021
Citation:
Aadit Shah, Ryan P Tantone, Matthew Berchuck. Sacral Chordoma: Don’t throw away the Scalpel. Journal of Spine Research and Surgery 3 (2021): 017-023.
View / Download Pdf Share at FacebookAbstract
Sacral chordomas pose a difficult challenge for physicians due to the close proximity of neural, vascular, and visceral structures. Patients and physicians must weigh the risks and benefits of operative versus non operative management when deciding on treatment of these lesions. We report a complication of single dose intent to treat SBRT for a sacral chordoma that should serve to remind oncologists that radiation therapy, like surgery, is not without serious potential complications and that surgical resection may still be the best option for patients whose tumor can be treated with en bloc resection.
Keywords
Chordoma, Stereotactic Body Radiation Therapy, Sacroiliac Septic Arthritis
Chordoma articles Chordoma Research articles Chordoma review articles Chordoma PubMed articles Chordoma PubMed Central articles Chordoma 2023 articles Chordoma 2024 articles Chordoma Scopus articles Chordoma impact factor journals Chordoma Scopus journals Chordoma PubMed journals Chordoma medical journals Chordoma free journals Chordoma best journals Chordoma top journals Chordoma free medical journals Chordoma famous journals Chordoma Google Scholar indexed journals Stereotactic Body Radiation Therapy articles Stereotactic Body Radiation Therapy Research articles Stereotactic Body Radiation Therapy review articles Stereotactic Body Radiation Therapy PubMed articles Stereotactic Body Radiation Therapy PubMed Central articles Stereotactic Body Radiation Therapy 2023 articles Stereotactic Body Radiation Therapy 2024 articles Stereotactic Body Radiation Therapy Scopus articles Stereotactic Body Radiation Therapy impact factor journals Stereotactic Body Radiation Therapy Scopus journals Stereotactic Body Radiation Therapy PubMed journals Stereotactic Body Radiation Therapy medical journals Stereotactic Body Radiation Therapy free journals Stereotactic Body Radiation Therapy best journals Stereotactic Body Radiation Therapy top journals Stereotactic Body Radiation Therapy free medical journals Stereotactic Body Radiation Therapy famous journals Stereotactic Body Radiation Therapy Google Scholar indexed journals Sacroiliac Septic Arthritis articles Sacroiliac Septic Arthritis Research articles Sacroiliac Septic Arthritis review articles Sacroiliac Septic Arthritis PubMed articles Sacroiliac Septic Arthritis PubMed Central articles Sacroiliac Septic Arthritis 2023 articles Sacroiliac Septic Arthritis 2024 articles Sacroiliac Septic Arthritis Scopus articles Sacroiliac Septic Arthritis impact factor journals Sacroiliac Septic Arthritis Scopus journals Sacroiliac Septic Arthritis PubMed journals Sacroiliac Septic Arthritis medical journals Sacroiliac Septic Arthritis free journals Sacroiliac Septic Arthritis best journals Sacroiliac Septic Arthritis top journals Sacroiliac Septic Arthritis free medical journals Sacroiliac Septic Arthritis famous journals Sacroiliac Septic Arthritis Google Scholar indexed journals spine tumor articles spine tumor Research articles spine tumor review articles spine tumor PubMed articles spine tumor PubMed Central articles spine tumor 2023 articles spine tumor 2024 articles spine tumor Scopus articles spine tumor impact factor journals spine tumor Scopus journals spine tumor PubMed journals spine tumor medical journals spine tumor free journals spine tumor best journals spine tumor top journals spine tumor free medical journals spine tumor famous journals spine tumor Google Scholar indexed journals sacral chordoma articles sacral chordoma Research articles sacral chordoma review articles sacral chordoma PubMed articles sacral chordoma PubMed Central articles sacral chordoma 2023 articles sacral chordoma 2024 articles sacral chordoma Scopus articles sacral chordoma impact factor journals sacral chordoma Scopus journals sacral chordoma PubMed journals sacral chordoma medical journals sacral chordoma free journals sacral chordoma best journals sacral chordoma top journals sacral chordoma free medical journals sacral chordoma famous journals sacral chordoma Google Scholar indexed journals coronary artery disease articles coronary artery disease Research articles coronary artery disease review articles coronary artery disease PubMed articles coronary artery disease PubMed Central articles coronary artery disease 2023 articles coronary artery disease 2024 articles coronary artery disease Scopus articles coronary artery disease impact factor journals coronary artery disease Scopus journals coronary artery disease PubMed journals coronary artery disease medical journals coronary artery disease free journals coronary artery disease best journals coronary artery disease top journals coronary artery disease free medical journals coronary artery disease famous journals coronary artery disease Google Scholar indexed journals erythema articles erythema Research articles erythema review articles erythema PubMed articles erythema PubMed Central articles erythema 2023 articles erythema 2024 articles erythema Scopus articles erythema impact factor journals erythema Scopus journals erythema PubMed journals erythema medical journals erythema free journals erythema best journals erythema top journals erythema free medical journals erythema famous journals erythema Google Scholar indexed journals iliac joint articles iliac joint Research articles iliac joint review articles iliac joint PubMed articles iliac joint PubMed Central articles iliac joint 2023 articles iliac joint 2024 articles iliac joint Scopus articles iliac joint impact factor journals iliac joint Scopus journals iliac joint PubMed journals iliac joint medical journals iliac joint free journals iliac joint best journals iliac joint top journals iliac joint free medical journals iliac joint famous journals iliac joint Google Scholar indexed journals lumbar spine articles lumbar spine Research articles lumbar spine review articles lumbar spine PubMed articles lumbar spine PubMed Central articles lumbar spine 2023 articles lumbar spine 2024 articles lumbar spine Scopus articles lumbar spine impact factor journals lumbar spine Scopus journals lumbar spine PubMed journals lumbar spine medical journals lumbar spine free journals lumbar spine best journals lumbar spine top journals lumbar spine free medical journals lumbar spine famous journals lumbar spine Google Scholar indexed journals SI pseudoarthrosis articles SI pseudoarthrosis Research articles SI pseudoarthrosis review articles SI pseudoarthrosis PubMed articles SI pseudoarthrosis PubMed Central articles SI pseudoarthrosis 2023 articles SI pseudoarthrosis 2024 articles SI pseudoarthrosis Scopus articles SI pseudoarthrosis impact factor journals SI pseudoarthrosis Scopus journals SI pseudoarthrosis PubMed journals SI pseudoarthrosis medical journals SI pseudoarthrosis free journals SI pseudoarthrosis best journals SI pseudoarthrosis top journals SI pseudoarthrosis free medical journals SI pseudoarthrosis famous journals SI pseudoarthrosis Google Scholar indexed journals
Article Details
1. Introduction
Treatment of spine tumors typically requires a team
approach including orthopedic/neurosurgeons, medical and radiation oncologists. As new treatment modalities emerge the treatment strategy for spine tumor continues to evolve. Chordomas and chondrosarcoma constitute the majority of malignant sacral tumors in adulthood. Histologically, these tumors are low to intermediate grade, however, they are locally invasive and have a high propensity to recur following surgery. They often present with advanced local disease, making them challenging to treat. When possible, en bloc surgical resection has been the recommended treatment for these tumors. Current literature clearly demonstrates that wide en bloc resection with negative surgical margins is the single most important predictor of tumor recurrence and long term survival [1, 2].
Unfortunately, the proximity of these tumors to neural, vascular, and visceral structures creates significant challenges to achieving the desired level of resection. Most of these tumors have an insidious onset and can be quite large at presentation. Advances in radiation oncology, specifically stereotactic body radiation (SBRT), which allows delivery of high dose radiation to the tumor while limiting exposure to normal adjacent structures, has recently led some oncologists to use this as definitive treatment for certain tumors. In addition to eliminating operative morbidity, SBRT offers a treatment option that spares neural structures that control important functions (i.e. bowel, bladder, sexual, extremity). SBRT is not without significant risks and associated morbidities. In this report we present a case of a gentleman with a sacral chordoma who was offered en bloc resection but elected to proceed with SBRT. We report a complication of single dose intent to treat SBRT for a sacral chordoma that should serve to remind oncologists that radiation therapy, like surgery, is not without serious potential complications and that surgical resection may still be the best option for patients whose tumor can be treated with en bloc resection.
2. Case Report
The patient is a 77-year-old male who five years ago had been treated for a sacral chordoma with SBRT presented to the ED with lumbosacral pain. The original tumor involved the S1, S2 segments as well as the ilium adjacent to the right sacroiliac joint. He also reported bilateral lower extremity weakness. He denied paresthesia, fevers, or chills. The patient previously ambulated with a cane, but now required a walker and wheelchair. The patient’s medical history is significant for diabetes, coronary artery disease, hypertension, and gout. At the time of diagnosis, the patient was offered en bloc resection; however, he declined surgical treatment due to his desire to avoid nerve sacrificing surgery and a difficult sacral reconstruction. He was treated with single fraction SBRT. Following radiosurgery, the patient experienced significant skin breakdown over the sacrum as well as osteomyelitis which took two years to manage with antibiotics, multiple wound debridements and soft tissue coverage procedures.
On exam, he had well healed flaps over the sacral area (Figure 1) with no warmth, erythema, or fluctuance. He was tender at the left sacroiliac joint. There was a positive Patrick’s test on the left. Neurologic evaluation of the lower extremities revealed 5/5 motor strength in all muscle groups. He had diminished sensation in both legs due to diabetic neuropathy. He was able to stand with great difficulty and could not ambulate without severe pain. Diagnostic imaging revealed extensive osseous erosion involving bilateral sacroiliac joints and left sacroiliac joint septic arthritis (Figure 2). He had been previously treated with several 6 week courses of IV antibiotics. Due to the patient's worsening pain and decreased ambulatory status, he was indicated for sacroiliac joint debridement and fusion. We performed a dual approach involving initial anterior left SI joint debridement/ fusion followed by posterior lumbopelvic fixation (Figure 3). Post-operatively, the patient received a 6 week course of IV vancomycin. Initially, he demonstrated significant improvement in his pain and mobility. At six months post-op the patient noted increasing pain and deteriorating bowel and bladder function. Over time his functional status continued to decline; however, he remains alive 7 years after his diagnosis. Surgical pathology did not show any evidence of recurrent chordoma or new malignancy. The biopsy was consistent with radiation induced osteonecrosis. CT scan 14 month post op shows the hardware to be intact with pseudoarthrosis of the left SI joint (Figure 4).

Figure 1: Well healed flap without erythema or fluctuance on initial presentation physical exam.
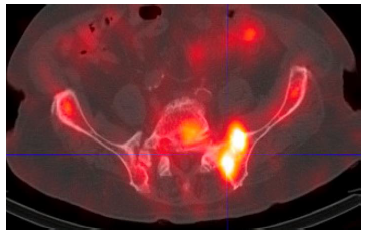
Figure 2: Spect CT scan showing Intense gallium uptake within the left sacral wing and left sacral iliac joint.

Figure 3: Anteroposterior pelvis and lateral lumbar spine image showing post-operative spinopelvic fixation.
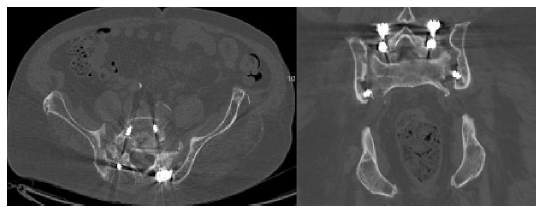
Figure 4: Left SI pseudoarthrosis.
3. Discussion
Chordomas are rare slow-growing malignant tumors compromising 1-4 % of all primary bone tumors [3]. They arise from the remnants of the notochord and present in the 5th-7th decade of life, occurring three times more often in men than women [4]. Population-based studies suggest an incidence of chordoma of 0·08 per 100 000, with predominance in men and peak incidence between 50–60 years of age. There is a very low incidence in patients younger than 40 years, and rarely in children and adolescents (<5% of all chordoma cases) [5]. Histologically considered to be a low-grade neoplasm, they often recur and rarely metastasize. Chordomas were believed to most commonly occur in the sacrum; however, recent evidence suggests an almost equal distribution in the skull base (32%), mobile spine (32·8%), and sacrum (29·2%) [6]. Chordomas are typically not sensitive to chemotherapy or external beam radiation, and therefore surgical resection has been the primary form of treatment.
The most important factor for disease-free survival is achieving an en bloc resection with negative margins. Their proximity to the spinal cord, cauda equina, bowel and other vital structures can make en bloc resection difficult to achieve. Confounding management is that often these tumors have grown considerably before diagnosis and so can be quite large on presentation. While sacral chordomas that are from S3-S5 can be resected through a posterior only approach, the presence of anterior soft tissue mass that extends as high as S1, S2 will require a more extensive resection and reconstruction. In tumors that involve the proximal sacrum en bloc resection requires resection of sacral roots, which sacrifice bowel, bladder, and sexual function. Because of that risk, SBRT would appear to be an attractive option of managing these tumors, however SBRT is not without significant risks and associated morbidities. Our patient was initially offered surgical resection; however, he opted for SBRT as primary treatment and had a prolonged and difficult disease course. He developed bone and soft tissue necrosis requiring multiple surgical procedures and chronic suppressive antibiotics to achieve soft tissue coverage. His course was further complicated by osteonecrosis of sacrum followed by sacroiliac septic arthritis/ osteomyelitis. His quality of life was significantly affected.
The incidence of sacroiliac septic arthritis is rare, ranging from 1-2% [7, 8]. The diagnosis is often delayed, with 75% of cases presenting with vague symptoms [9]. MRI and CT can demonstrate fluid in the SI joint and bony involvement, but are often not obtained in the acute setting [10, 11]. While surgical resection has been considered the mainstay of treatment for sacral chordoma, surgery alone has been associated with suboptimal local control when en bloc resection is not achieved. A 43% local recurrence at median 6 year follow up was found in a meta-analysis of published sacral chordoma series from 1980-2016 that included 1235 patients (80% R 0/1 resections and 37% RT adjuvant) [12]. Surgery, especially for high sacral tumors has also been associated with significant morbidity. Memorial Sloan Kettering published a series of 42 sacral chordoma patients undergoing surgery (89% R0/1 resection and 12 % adjuvant radiation) with reported complication including 74% self-catheterization, 67% sexual dysfunction, and 29% permanent colostomy [13]. Advances in radiation oncology have dramatically affected the management of spinal tumors. Conventional doses of external beam radiation therapy are constrained by spinal cord and cauda equina tolerance, usually at 45 Gy and 60 Gy respectively [14].
Advances in radiation oncology have allowed safe delivery of significantly higher doses. Three major techniques have been used to deliver this higher doses: photon based SBRT, proton therapy and carbon ion therapy [15]. Particle therapy (proton and carbon ion) uses the physical properties of charged particles to increase tumor dose while sparing normal tissue whereas SBRT uses superior localization and conformality of the photons.
Radiation effects on the skeleton range from osteopenia to necrosis and vary based on the location, dose and fractionation of the beam. The effects of high dose radiation on adjacent soft tissues are also significant in the development of osteoradionecrosis [16]. Radiotherapy causes a hypo vascular, hypoxic and hypocellular environment in which the basic metabolic demands for cellular survival cannot be met. Under these conditions bone becomes devitalized and adjacent soft tissues break down. Exposure of bone to radiation primarily damages osteoblasts, resulting in reduced production of bone matrix [17]. This, in turn, leads to osteopenia due to unopposed osteoclast function making the bone prone to fractures [18]. Osteoradionecrosis is most commonly described in the head and neck literature after treatment of head and neck cancer with reports suggesting that it affects the mandible and maxilla in up to 22% and 11% of patients, respectively [19]. Osteoradionecrosis of the spine is a well recognized complication of SBRT. Memorial sloan Kettering was the first institution to report on SBRT induced vertebral compression fracture (VCF) with VCF in 27(39%) of 71 sites treated with SBRT and the median reported time was 25 months post treatment [20]. In their reports MD Anderson Cancer Center (MDACC) and University of Toronto (UofT) suggested that the risk may be closer to 11% to 20%, with a median time to VCF of 2 to 3 months [21, 22].
Our patient developed osteonecrosis from SBRT affecting the sacrum which led to osteomyelitis and sacroiliac septic arthritis. The RTOG is a widely used grading scheme to describe the complications of radiation therapy. The grading scheme varies from 0 (no symptoms) to 5 (death), which directly relates to radiation dose [23]. Our patient experienced grade 4 radiation toxicity involving skin (ulceration), subcutaneous (necrosis), bone (necrosis/ spontaneous fracture) and joint (necrosis). The typical single fraction SRBT dose for a chordomas is 16 Gy [24]. Toxicity can be seen with doses as low as 9.2 Gy, with risks of radiation myelopathy beginning at 12.4 Gy [25, 26]. There is no well-defined dose at which skin and subcutaneous tissue toxicity begins, but skin toxicity has been reported with single doses of 15 Gy [27]. Our case illustrates the significant morbidity that can occur with intent to treat SBRT for a sacral chordoma. Patients should be aware of these potential complications of SBRT when deciding between surgery and radiation as the primary treatment of sacral chordoma.
References
- Sciubba DM, Chi JH, Rhines LD, Gokaslan ZL. Chordoma of the spinal column. Neurosurg Clin N Am 19 (2008): 5-15.
- Fourney DR, Gokaslan ZL. Current management of sacral chordoma. Neurosurg Focus 15 (2003): E9.
- Hsieh PC, Xu R, Sciubba DM, et al. Long-term clinical outcomes following en bloc resections for sacral chordomas and chondrosarcomas: a series of twenty consecutive patients. Spine (Phila Pa 1976) 34 (2009): 2233-2239.
- Samson IR, Springfield DS, Suit HD, et al. Operative treatment of sacrococcygeal chordoma. A review of twenty-one cases. J Bone Joint Surg Am 75 (1993): 1476-1484.
- Walcott BP, Nahed BV, Mohyeldin A, et al. Chordoma: current concepts, management, and future directions. Lancet Oncol 13 (2012): e69-e76.
- McMaster ML, Goldstein AM, Bromley CM, et al. Chordoma: incidence and survival patterns in the United States, 1973-1995. Cancer Causes Control 12 (2001): 1-11.
- Woytala PJ, Sebastian A, Blach K, et al. Septic arthritis of the sacroiliac joint. Reumatologia 56 (2018): 55-58.
- Vyskocil JJ, McIlroy MA, Brennan TA, et al. Pyogenic infection of the sacroiliac joint. Case reports and review of the literature. Medicine (Baltimore) 70 (1991): 188-197.
- Zimmermann B 3rd, Mikolich DJ, Lally EV. Septic sacroiliitis. Semin Arthritis Rheum 26 (1996): 592-604.
- Klein MA, Winalski CS, Wax MR, et al. MR imaging of septic sacroiliitis. J Comput Assist Tomogr 15 (1991): 126-132.
- Hermet M, Minichiello E, Flipo RM, et al. Infectious sacroiliitis: a retrospective, multicentre study of 39 adults. BMC Infect Dis 12 (2012): 305.
- Kerekes D, Goodwin CR, Ahmed AK, et al. Local and Distant Recurrence in Resected Sacral Chordomas: A Systematic Review and Pooled Cohort Analysis. Global Spine J 9 (2019): 191-201.
- Schwab JH, Healey JH, Rose P, et al. The surgical management of sacral chordomas. Spine (Phila Pa 1976) 34 (2009): 2700-2704.
- Emami B, Lyman J, Brown A, et al. Tolerance of normal tissue to therapeutic irradiation. Int J Radiat Oncol Biol Phys 21 (1991): 109-122.
- Konieczkowski DJ, DeLaney TF, Yamada YJ. Radiation Strategies for Spine Chordoma: Proton Beam, Carbon Ions, and Stereotactic Body Radiation Therapy. Neurosurg Clin N Am 31 (2020): 263-288.
- Marx RE. Osteoradionecrosis: a new concept of its pathophysiology. J Oral Maxillofac Surg 41 (1983): 283-288.
- Ergün H, Howland WJ. Postradiation atrophy of mature bone. CRC Crit Rev Diagn Imaging 12 (1980): 225-243.
- Williams HJ, Davies AM. The effect of X-rays on bone: a pictorial review. Eur Radiol 16 (2006): 619-633.
- Støre G, Boysen M. Mandibular osteoradionecrosis: clinical behaviour and diagnostic aspects. Clin Otolaryngol Allied Sci 25 (2000): 378-384.
- Rose PS, Laufer I, Boland PJ, et al. Risk of fracture after single fraction image-guided intensity-modulated radiation therapy to spinal metastases. J Clin Oncol 27 (2009): 5075-5079.
- Cunha MV, Al-Omair A, Atenafu EG, et al. Vertebral compression fracture (VCF) after spine stereotactic body radiation therapy (SBRT): analysis of predictive factors. Int J Radiat Oncol Biol Phys 84 (2012): e343-e349.
- Boehling NS, Grosshans DR, Allen PK, et al. Vertebral compression fracture risk after stereotactic body radiotherapy for spinal metastases. J Neurosurg Spine 16 (2012): 379-386.
- Cox JD, Stetz J, Pajak TF. Toxicity criteria of the Radiation Therapy Oncology Group (RTOG) and the European Organization for Research and Treatment of Cancer (EORTC). Int J Radiat Oncol Biol Phys 31 (1995): 1341-1346.
- Jung EW, Jung DL, Balagamwala EH, et al. Single-Fraction Spine Stereotactic Body Radiation Therapy for the Treatment of Chordoma. Technol Cancer Res Treat 16 (2017): 302-309.
- Huo M, Sahgal A, Pryor D, et al. Stereotactic spine radiosurgery: Review of safety and efficacy with respect to dose and fractionation. Surg Neurol Int 8 (2017): 30.
- Sahgal A, Chang JH, Ma L, et al. Spinal Cord Dose Tolerance to Stereotactic Body Radiation Therapy [published online ahead of print, 2019 Oct 10]. Int J Radiat Oncol Biol Phys (2019).
- Milano MT, Constine LS, Okunieff P. Normal tissue toxicity after small field hypofractionated stereotactic body radiation. Radiat Oncol 3 (2008): 36.
