Robotic colorectal cancer surgery in the elderly - A monocentric analysis of short-term postoperative outcomes in patients ≥ 75 years versus <75 years
Article Information
Mazin Hamed1*, Melanie Holzgang1, Yining Chen2, Wanda Ward1, Dolly Dowsett1, Irshad Shaikh1,3, Ahmed El-Hadi1
1Sir Thomas Brown Colorectal Unit, Norfolk and Norwich University Hospital, UK
2Department of Statistics, London School of Economics and Political Science, London, UK
3Professor of Surgery, University of East Anglia, Norwich, UK
*Corresponding Author: Mazin Hamed, Sir Thomas Brown Colorectal Unit, Norfolk and Norwich University Hospital, UK
Received: 14 November 2023; Accepted: 20 November 2023; Published: 04 December 2023
Citation: Mazin Hamed, Melanie Holzgang, Yining Chen, Wanda Ward, Dolly Dowsett, Irshad Shaikh, Ahmed El-Hadi. Robotic colorectal cancer surgery in the elderly - A monocentric analysis of short-term postoperative outcomes in patients ≥ 75 years versus <75 years. Journal of Surgery and Research. 6 (2023): 391-400.
View / Download Pdf Share at FacebookAbstract
Introduction: Colorectal cancer is becoming an increasingly common health issue, especially among the elderly population. We aimed to assess the shortterm postoperative outcomes of robotic colorectal cancer surgery in elderly (≥ 75 years) and non-elderly (<75 years) patient groups.
Materials and Methods: Patients who underwent robotic colorectal cancer resections in our tertiary colorectal referral center between October 2017 and May 2022 with the Da Vinci X system were included in this retrospective study. Patients were divided into two groups: the “elderly group” including patients ≥75 years, and the “non-elderly” group including patients <75 years. The short-term postoperative outcomes between these two groups were then compared using the Chi-squared/Fisher’s exact or Wilcoxon test. Differences were considered statistically significant at P< 0.05.
Results: A total of 228 patients were included in our study; 61 patients ≥ 75 years old (elderly group) and 167 patients < 75 years old (non-elderly group).
Although there were no statistically significant differences observed between the elderly and non-elderly patient groups regarding length of hospital stay, anastomotic leak, re-admission and re-operation rates, the elderly group had a significantly shorter operative time (mean time 275.35 minutes vs. 315.14 minutes; p < 0.001) compared to the non-elderly group. The results for left and right robotic colonic cancer resections were analyzed separately and there were no statistical differences observed in any of the outcomes that were included in our study.
Conclusion: Our study results on robotic colorectal cancer surgery in elderly patients suggest that it is a safe and feasible surgical approach. The operative times and short-term postoperative outcomes of elderly patients were comparable to those of the non-elderly group. This indicates that robotic colorectal cancer surgery is a viable option for elderly patients.
Keywords
Robotic surgery, Colorectal cancer, Elderly patients, Robotic outcomes
Article Details
Introduction
The world’s population is getting older every decade. This phenomenon, so-called “population ageing”, resulting in a growing proportion of older people within world populations. This trend can already be seen in many parts of the world, as shown by population projections which indicate that the world's elderly will constitute more than 15% of the world’s population by 2030 [1,2]. As the elderly population continues to grow, the incidence of colorectal cancer in this demographic is projected to increase significantly. Currently, 60% of patients diagnosed with colorectal cancer are over 70 years old at the time of diagnosis, with 43% being over 75 years old [3].
Despite the laparoscopic approach being widely accepted as the standard of care for colorectal surgeries, initial concerns about its safety and tolerance in elderly populations were raised. However, multiple studies conducted over the past decades have confirmed laparoscopic colorectal surgery to be a safe procedure even in the elderly group [4-9].
Robotic colorectal surgery has become increasingly popular and is seen as a breakthrough in the field of minimal-invasive surgery. Compared to traditional laparoscopic surgery, robotic colorectal surgery offers three-dimensional views, good access to the pelvis due to more flexible instrument mobility and a stable camera platform. There is increasing evidence that robotic abdominal surgery might offer advantages such as less postoperative pain and faster recovery compared to laparoscopy, with similar complication rates and oncological adequacy [10,11].
The study by Zhang et al. provided valuable insight into the comparative outcomes of robotic-colorectal resections and laparoscopic colorectal resections. It showed that robotic surgery could provide an advantage in terms of lower conversion rates, shorter length of stay and lower intraoperative blood loss, with oncological outcomes and postoperative morbidity being comparable between the two groups [12]. The study conducted by Hettiarachi et al. demonstrated that robotic colorectal resections had several advantages over laparoscopic colorectal resections, including but not limited to shorter length of stay, lower conversion rates, shorter median operative time and lower complication rate [13].
Recent evidence suggests that robotic surgery is an effective and safe option for elderly patients, who are often at greater risk of perioperative complications. Buchs et al. found that elderly patients undergoing diverse abdominal robotic procedures experienced low mortality, short hospital stays, and acceptable morbidity [14]. Moreover, several studies investigating gynecological robotic procedures in elderly patients found no higher complication rates than those seen in younger women [15,16].
Several papers have compared robotic and laparoscopic outcomes in colorectal surgery in the elderly population. De'Angelis et al. found that robotic colorectal resection was associated with a longer operative time, but similar operative and oncological outcomes as the laparoscopic group in the elderly population [17]. The study by Srinath et al. further suggested that robotic right hemicolectomies could be a feasible option for octogenarians (patients >80 years), with similar oncological outcomes and a shorter length of stay compared to the laparoscopic group [7]. The results of Palomba et al.’s study found similiar outcomes between robotic and laparoscopic colonic resections for elderly patients. No significant differences were found between the two surgical techniques in terms of conversion rate, postoperative complications or oncological results [18].
Recent research has begun to investigate the comparative outcomes of robotic colorectal surgery between elderly and non-elderly patients. The study by Weih-Chi et al. showed that elderly patients have comparable outcomes to younger patients in robotic colorectal surgery. They found that the length of hospital stay, as well as disease-free and overall survival were similar in both groups. Additionally, postoperative complications were lower in the elderly group [19]. The study by Hannan E et al. [20] concluded that there were no significant differences in postoperative complications, reoperation, wound infection, anastomotic leak or mortality between the two surgical procedures. The findings of the study by Cuellar-Gomez et al. add to mounting evidence that robotic surgery is a safe and viable treatment option for elderly colorectal cancer patients. The study found that robotic surgery provided an acceptable postoperative morbidity rate and a favorable cancer-specific survival outcome [21].
On this background, this paper aims to investigate and analyze our monocentric outcomes of robotic colorectal cancer surgery in a retrospective study involving patients aged 75 years or older compared to those below the age of 75.
Material and Methods
This is a retrospective study including patients who underwent robotic colorectal cancer resections in our tertiary colorectal referral center between October 2017 and May 2022. Patients were divided into two groups, the “elderly group” including patients ≥75 years and the “non-elderly” group, including patients <75 years. All robotic resections were performed by two colorectal consultants and one international fellow with the Da Vinci X surgical system (Intuitive Surgical, Sunnyvale, CA, USA).
The procedures included in our study were right hemicolectomies with or without complete mesocolic excision (CME) and with/without intracorporeal anastomosis, high anterior resections (tumor above the peritoneal reflection), low anterior resections (tumor below the peritoneal reflection) with/without ileostomy, Hartmann procedures as well as segmental resections for splenic flexure tumors (limited colonic resection ligating the left ascending colonic artery and the left middle colic artery selectively). Our study excluded robotic exenterations and robotic operations for benign conditions such as robotic rectopexy for rectal prolapse.
Data were analyzed from a prospectively maintained operative database starting October 2017. Patient data included demographics such as age at time of surgery, gender, American Society of Anesthesiology (ASA) grading and body mass index (BMI). Furthermore, data collected from the procedure included type and length of procedure, conversion to open, length of stay, perioperative morbidity using the Clavien-Dindo score, re-operations, 90-day re-admission and 90 -day mortality rates. In addition to the above-mentioned data, other factors such as tumor staging (TNM), use of neo-adjuvant and adjuvant chemotherapy (CT) and/or radiotherapy (RT) and height of the tumor from the anal verge in left colorectal resections were also included. All patients were discussed in the multidisciplinary tumor board meeting, both pre- and postoperatively. This discussion encompassed all clinical aspects related to the patient's disease, such as prognosis and treatment planning. Following the meeting, all patients were included in a nurse-led colorectal cancer follow-up programme according to their tumor stage. The authors limited patient inclusion to May 2022 to ensure a 90-day follow-up period was available for the analysis of short-term postoperative outcomes.
The statistical analysis was conducted using the Chi-squared or Fisher’s exact test for categorical data and the Wilcoxon test for continuous data.
Results
Patient demographics
A total of 228 patients were included in our study. 61 of these patients were ≥ 75 years old (elderly group), while 167 were < 75 years old (non-elderly group). The mean age of the elderly group was 78.8 (standard deviation 3.24), and that of the non-elderly group was 62.6 (standard deviation 9.27). No significant differences were observed among the two groups in terms of gender distribution, body mass index (BMI), number of patients who had previous abdominal operations, TNM stage, and the percentage of patients who had undergone neoadjuvant/adjuvant radiotherapy and/or chemotherapy (Table 1).
Analysis of patient characteristics revealed notable significant differences between the elderly and non-elderly age groups. Specifically, 41.7% of patients in the elderly group had an American Society of Anesthesiologists (ASA) score of 3 or higher, while only 19.6% of patients in the non-elderly group had an ASA score of 3 or higher (p < 0.001). In addition, 81.4% of operations in the non-elderly group were left-sided, compared to only 50% of operations in the elderly group (p < 0.001) (Table 1).
|
Characteristics |
≥ 75 years (n = 61) |
< 75 years (n = 167) |
p values |
|
Age, mean (SD) |
78.80 (3.24) |
62.61 (9.27) |
< 0.001 |
|
Gender, n (%) |
0.105 |
||
|
Male |
27 (44.3%) |
96 (57.5%) |
|
|
Female |
34 (55.7%) |
71 (42.5%) |
|
|
BMI, n (%) |
0.329 |
||
|
Normal weight (< 25.0) |
16 (26.7%) |
38 (22.9%) |
|
|
Overweight (25.0–29.9) |
32 (53.3%) |
73 (44.0%) |
|
|
Obesity class I (30.0–34.9) |
8 (13.3%) |
41 (24.7%) |
|
|
Obesity class II (35.0–39.9) |
4 (6.7%) |
11 (6.6%) |
|
|
Obesity class III (40.0+) |
0 (0.0%) |
3 (1.8%) |
|
|
ASA, n (%) |
<0.001 |
||
|
1 |
0 (0.0%) |
13 (8.0%) |
|
|
2 |
35 (58.3%) |
118 (72.4%) |
|
|
3 |
25 (41.7%) |
32 (19.6%) |
|
|
T, n (%) |
0.133 |
||
|
0 |
1 (3.7%) |
8 (4.8%) |
|
|
1 |
4 (6.9%) |
23 (13.9%) |
|
|
2 |
9 (15.5%) |
32 (19.3%) |
|
|
3 |
34 (58.6%) |
91 (54.8%) |
|
|
4 |
10 (17.2%) |
12 (7.2%) |
|
|
N, n (%) |
0.507 |
||
|
0 |
43 (74.1%) |
110 (66.3%) |
|
|
1 |
10 (17.2%) |
41 (24.7%) |
|
|
2 |
5 (8.6%) |
15 (9.0%) |
|
|
M, n (%) |
0.293 |
||
|
0 |
59 (96.7%) |
164 (98.8%) |
|
|
1 |
2 (3.3%) |
2 (1.2%) |
|
|
CT/RT, n (%) |
1 |
||
|
Yes |
3 (4.9%) |
9 (5.4%) |
|
|
No |
58 (95.1%) |
158 (95.2%) |
|
|
Operation type, n (%) |
< 0.001 |
||
|
Left |
30 (50.0%) |
136 (81.4%) |
|
|
Right |
30 (50.0%) |
31 (18.6%) |
|
|
Stoma, n (%) |
0.313 |
||
|
Yes |
17 (27.9%) |
60 (36.1%) |
|
|
No |
44 (72.1%) |
106 (63.9%) |
|
|
Previous abdominal surgery, n (%) |
0.258 |
||
|
Yes |
23 (37.7%) |
48 (28.7%) |
|
|
No |
38 (62.3%) |
119 (71.3%) |
Table 1: Patient demographics
Overall operative outcomes
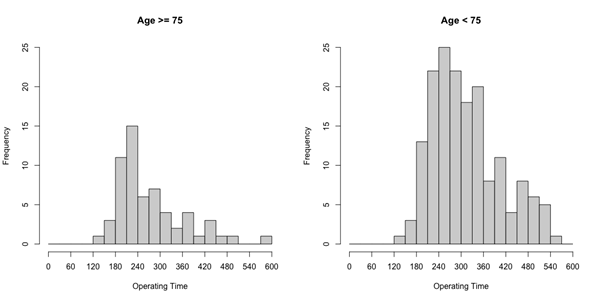
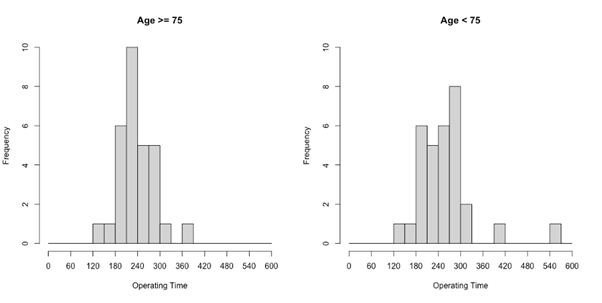
Our study revealed that there was no statistically significant difference between the two age groups regarding their overall operative outcomes, except for the duration of the operation. The duration of the operation was significantly lower in the elderly group (mean time 275.35 minutes vs. 315.14 minutes; p < 0.001) (Table 2) (Figure 1).
In addition, the results of our study showed that there were no statistically significant differences between the two groups when it came to conversion rates, postoperative morbidity and mortality, and 90-day re-admission or re-operation rates.
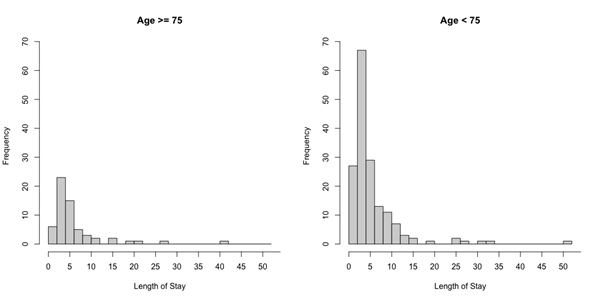
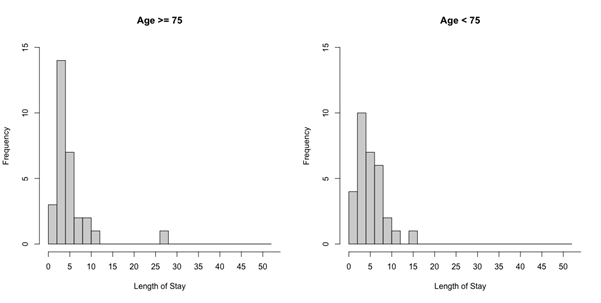
In terms of length of hospital stay, the mean for the elderly group was 6.82 days compared to 5.98 days in the non-elderly group, though the difference did not reach statistical significance (Figure 2). Similarly, the anastomotic leak rate was 1.5% in the elderly group (1/61) versus 9.0% in the non-elderly group (15/167), but the difference was not statistically significant (p = 0.076).
|
Outcome |
≥ 75 years (n = 61) |
< 75 years (n = 167) |
p values |
|
Duration of the Operation (in mins) |
275.35 (90.90) |
315.14 (92.59) |
<0.001 |
|
mean (SD) |
|||
|
Length of Hospital Stay (in days) |
6.82 (6.67) |
5.98 (6.25) |
0.054 |
|
mean (SD) |
|||
|
Conversion to Open |
1 |
||
|
Yes |
0 (0.0%) |
1 (0.6%) |
|
|
No |
60 (100.0%) |
166 (99.4%) |
|
|
Morbidity |
0.668 |
||
|
0 |
30 (50.0%) |
97 (58.1%) |
|
|
1 |
8 (13.3%) |
17 (10.2%) |
|
|
2 |
18 (30.0%) |
40 (24.0%) |
|
|
3 |
4 (6.7%) |
10 (6.0%) |
|
|
4 |
0 (0.0%) |
3 (1.8%) |
|
|
Leak |
0.076 |
||
|
Yes |
1 (1.6%) |
15 (9.0%) |
|
|
No |
60 (98.4%) |
152 (91.0%) |
|
|
Mortality (within 90 days) |
0.268 |
||
|
Yes |
1 (1.6%) |
0 (0.0%) |
|
|
No |
60 (98.4%) |
167 (100.0%) |
|
|
Readmission |
0.764 |
||
|
Yes |
3 (5.0%) |
12 (7.2%) |
|
|
No |
57 (95.0%) |
155 (92.8%) |
|
|
Reoperation |
1 |
||
|
Yes |
1 (1.7%) |
5 (3.0%) |
|
|
No |
59 (98.3%) |
162 (97.0%) |
Table 2: Univariate analysis of the operative outcomes in robotic colorectal cancer surgery between the elderly and non-elderly groups
Operative outcomes in robotic left segmental colectomies
The results of left and right robotic colonic cancer resections for elderly and non-elderly patients were analysed separately and summarized in tables 3 and 4. For the left-sided resections, 30 elderly patients and 136 non-elderly patients underwent high/low anterior resection, segmental colectomy for splenic flexure cancers or abdominoperineal resection.
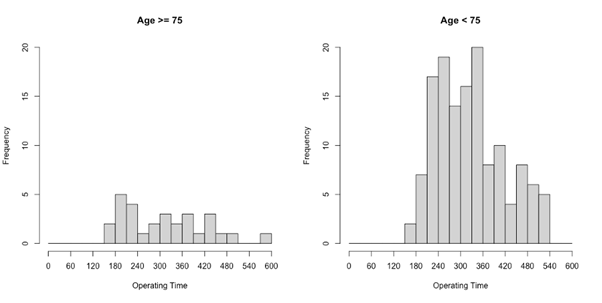
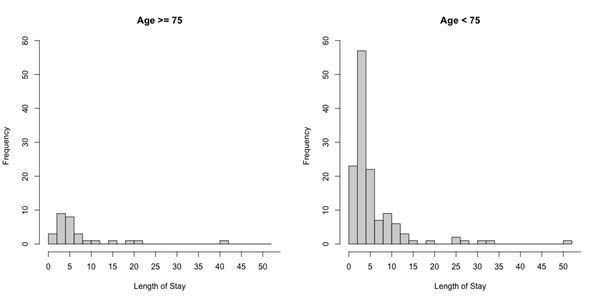
The results for left robotic colorectal cancer resections show that there were no significant differences between elderly and non-elderly patients in any of the outcomes that were analyzed. Operating time, length of hospital stay, conversion to open surgery, postoperative morbidity and anastomotic leak rate were comparable between the two groups. The 90-day mortality/re-admission and re-operation rates were also similar for the elderly and non-elderly patients (Table 3) (Figures 3,4).
Of note, the operative time was shorter in the elderly group compared to the non-elderly group (314.66 minutes vs. 327.76 minutes), but this did not reach statistical significance (p = 0.347). Similarly, the length of hospital stay was over a day longer in the elderly group (7.72 vs. 6.08), however, this was also not statistically significant (p = 0.054). The absolute rate of anastomotic leaks was higher in the non-elderly group (11% vs. 0%), yet again no statistically significant difference was found (p = 0.075). Moreover, the rate of re-admission and re-operation were both higher in the non-elderly group than in the elderly group, but the difference did not reach statistical significance (Table 3).
|
Outcome |
≥ 75 years (n = 30) |
< 75 years (n = 136) |
p values |
|
Duration of the Operation (in mins) |
314.66 (110.14) |
327.76 (91.59) |
0.347 |
|
mean (SD) |
|||
|
Length of Hospital Stay (in days) |
7.72 (8.15) |
6.08 (6.76) |
0.054 |
|
mean (SD) |
|||
|
Conversion to Open |
1 |
||
|
Yes |
0 (0.0%) |
1 (0.7%) |
|
|
No |
29 (100.0%) |
135 (99.3%) |
|
|
Morbidity |
0.254 |
||
|
0 |
13 (44.8%) |
82 (60.3%) |
|
|
1 |
3 (10.3%) |
13 (9.6%) |
|
|
2 |
12 (41.4%) |
29 (21.3%) |
|
|
3 |
1 (3.4%) |
9 (6.6%) |
|
|
4 |
0 (0.0%) |
3 (2.2%) |
|
|
Leak |
0.075 |
||
|
Yes |
0 (0.0%) |
15 (11.0%) |
|
|
No |
30 (100.0%) |
121 (89.0%) |
|
|
Mortality (within 90 days) |
1 |
||
|
Yes |
0 (0.0%) |
0 (0.0%) |
|
|
No |
30 (100.0%) |
136 (100.0%) |
|
|
Readmission |
0.694 |
||
|
Yes |
1 (3.4%) |
11 (8.1%) |
|
|
No |
28 (96.6%) |
125 (91.9%) |
|
|
Reoperation |
0.588 |
||
|
Yes |
0 (0.0%) |
5 (3.7%) |
|
|
No |
29 (100.0%) |
131 (96.3%) |
Table 3: Univariate analysis of the operative outcomes in robotic left segmental colectomies between the elderly and the non-elderly groups
Operative outcomes in robotic right segmental colectomies
The results of our study showed no significant difference in postoperative outcomes between the elderly and non-elderly patients in those who underwent robotic right colonic cancer resection (Table 4). Absolute operative times for elderly patients were shorter, though not statistically significant (239.13 minutes compared to 259.81 minutes in the non-elderly group; p=0.363). Length of hospital stay, re-admission and re-operation rates, postoperative morbidity and mortality were also comparable between groups (Table 4, Figures 5,6).
|
Outcome |
≥ 75 years (n = 30) |
< 75 years (n = 31) |
p values |
|
Duration of the Operation (in mins) mean (SD) |
239.13 (45.81) |
259.81 (76.20) |
0.363 |
|
Length of Hospital Stay (in days) mean (SD) |
5.63 (4.59) |
5.52 (3.22) |
0.867 |
|
Conversion to Open |
1 |
||
|
Yes |
0 (0.0%) |
0 (0.0%) |
|
|
No |
30 (100.0%) |
31 (100.0%) |
|
|
Morbidity |
0.557 |
||
|
0 |
17 (56.7%) |
15 (48.4%) |
|
|
1 |
5 (16.7%) |
4 (12.9%) |
|
|
2 |
6 (20.0%) |
11 (35.5%) |
|
|
3 |
2 (6.7%) |
1 (3.2%) |
|
|
4 |
0 (0.0%) |
0 (0.0%) |
|
|
Leak |
0.492 |
||
|
Yes |
1 (3.3%) |
0 (0.0%) |
|
|
No |
29 (96.7%) |
31 (100.0%) |
|
|
Mortality (within 90 days) |
0.492 |
||
|
Yes |
1 (3.3%) |
0 (0.0%) |
|
|
No |
29 (96.7%) |
31 (100.0%) |
|
|
Readmission |
0.612 |
||
|
Yes |
2 (6.7%) |
1 (3.2%) |
|
|
No |
28 (93.3%) |
30 (92.8%) |
|
|
Reoperation |
0.492 |
||
|
Yes |
1 (3.3%) |
0 (0.0%) |
|
|
No |
29 (96.7%) |
31 (100.0%) |
Table 4: Univariate analysis of the operative outcomes in robotic right segmental colectomies between the elderly and the non-elderly groups
Discussion
Colorectal cancer is one of the most common forms of cancer in Europe, affecting both men and women. According to data from 2020, it is the second most common cancer in women (12.4%) and third most common cancer in men (13.2%). It is most prevalent among the elderly population, and with the trend of “population ageing” set to continue in the coming decades, it is likely that this age group will be increasingly affected by colorectal cancer [22].
Robotic platforms are becoming increasingly popular in colorectal surgery departments all over the world, as evidence suggests that they may offer a shorter hospital stay and faster return to bowel function than laparoscopic surgery [10, 11,14]. Moreover, with the increasing use of robotic platforms in the elderly population, studies have shown that robotic procedures are generally well-tolerated by the elderly [14-16]. While the assumption may be that robotic colorectal surgery in elderly patients results in poor postoperative outcomes due to longer operating times and longer static Trendelenburg positioning; evidence suggests otherwise. Studies have shown that elderly patients are well-tolerated in robotic surgeries, with equal morbidity rates compared to other groups, lower conversion rates and shorter hospital stays [7,17,18]. These results demonstrate the efficacy of robotic surgery in elderly patients and highlight its potential in this population.
Our study, which analyzed the outcomes of 61 elderly patients (aged ≥75) and 166 non-elderly patients (aged <75) in robotic colorectal cancer operations, supports the existing literature with no significant differences found. Length of hospital stay, postoperative morbidity/mortality, anastomotic leaks and conversion rates did not differ between the two groups, indicating that robotic colorectal cancer surgery is feasible and safe in elderly patients. This data provides further evidence that age should not be a deterrent when considering robotic colorectal cancer surgery for elderly patients.
The results of our study demonstrated that elderly individuals had a trend towards shorter operative times when compared to non-elderly individuals. We initially interpreted this as selection bias as a relatively higher number of right-sided operations were done in the elderly group which usually takes less time. However, when looking specifically at the analysis of left and right colectomies, there was still a slight reduction in operative times for the elderly individuals for both types of operations, although this was not statistically significant. These results challenge the notion that robotic procedures in elderly individuals are often longer and more technically challenging.
A closer look at the absolute numbers revealed a lack of statistical significance difference in hospital stay between the two groups. However, the elderly group stayed over a day longer after left robotic colorectal resections compared to the non-elderly group, which is clinically significant. This phenomenon is likely because the elderly group had significantly higher comorbidities than the non-elderly group. These comorbidities may impede the postoperative recovery process and thus, delay the length of hospital stay. The findings from this study demonstrate that comorbidities should be considered when considering the care of elderly patients undergoing left robotic colorectal resections.
Our study showed that there was no statistically significant difference between the elderly and non-elderly groups when it came to postoperative morbidity, notably anastomotic leaks. However, the absolute number of anastomotic leaks in the non-elderly group was higher than that of the elderly group, and similarly, re-admission and re-operation rates were higher in the non-elderly group. One explanation for this could be that the non-elderly group had more left-sided colectomies performed than the elderly group. To back up this hypothesis, it was found that operative time, re-admission and re-operative rates were nearly equivalent between the two groups in the right-sided colectomies.
This study has several limitations. It was a non-randomized, retrospective and monocentric study. In addition, the sample size in the elderly population group is relatively small. Although it is larger than Wei-Chi et al.'s group study and comparable numbers to Hannan E et al. and Cuellar-Gomez et al.'s studies [19-21] which showed very similar results with no differences in the outcomes. Due to the small sample size definitive conclusions cannot be drawn. In order to definitively confirm these results, a larger multicenter or randomized controlled study would have to be conducted. Such a study could provide more insight into the potential benefits and limitations of the studied intervention. Thus, any conclusions must be interpreted with caution. Despite these limitations, the findings of this study are very promising and could potentially lead to improved outcomes for elderly patients.
Conclusion
Our study results on robotic colorectal cancer surgery in elderly patients suggest that it is a safe and feasible surgical approach. The operative times and short-term postoperative outcomes of elderly patients were comparable to those of the non-elderly group. This indicates that robotic colorectal cancer surgery is a viable option for elderly patients.
Conflict interest
The authors have no relevant financial or non-financial interests to declare.
Funding
None.
Acknowledgement
Not applicable.
Author contributions
All authors contributed to the study conception and design. Material preparation and data collection were performed by Melanie Holzgang, Mazin Hamed, Wanda Ward, Dolly Dowsett, Irshad Shaikh and Ahmed El-Hadi. Data analysis was performed by Yining Chen. The first draft of the manuscript was written by Melanie Holzgang, Mazin Hamed and Yining Chen and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
References
- https://ec.europa.eu/eurostat/web/main/data/database
- World Health Organization. Ageing and health (2021).
- Millan M. Treatment of colorectal cancer in the elderly, World Journal of Gastroenerology 15 7 (2015): 204-220.
- Hashida H. Laparoscopic Surgery for Colorectal Cancer in Super-Elderly patients: A single-center analysis, Surg Laparosc Endosc Percutan Tech 31 (2020): 337-341.
- Devoto L. Colorectal Cancer Surgery in the Very Elderly patient: a systematic review of laparoscopic versus open colorectal resection, Int J Colorectal Disease 32 (2017): 1237-1242.
- Li Y. Laparoscopic Colorectal Resection versus Open Colorectal Resection in octogenerians: a systematic review and meta-analysis of safety and efficacy, Techniques in Coloproctology 20 (2013): 153-162.
- Srinath H. Robot-Assisted vs Laparoscopic Right Hemicolectomy in Octogenerians. JAMDA 23 (2022) 690-694.
- Van der Pas MH. Laparoscopic versus open surgery for rectal cancer (COLOR II): short term outcomes of a randomized 3 trial, Lancet Oncol 14 (2013): 210-218.
- Evaluation of laparoscopic versus open colorectal surgery in elderly patients more than 70 years old: an evaluation of 727 patients. Int J Colorectal Dis 11 (2012): 36-41.
- Oldani A. Colorectal surgery in elderly patients: Our experience with Da Vinci Xi system. Age Clin Exp Res 11 (2016): 27-35.
- Papanikolaou G. Robotic surgery for colorectal cancer: systematic review of the literature. Surg Laparosc Endosc Percutan Tech 24 (2014): 478-483
- Zhang X. Robot-assisted versus laparoscopic-assisted surgery for colorectal cancer: a meta-analysis. Surg Endosc 12 (2015): 365-372.
- Hettiarachchi TS. Comparison of robotic vs laparoscopic left-sided colorectal cancer resections. Journal of Robotic Surgery,doi.org/10.1007/s11701-022-01414-9
- Buchs N et al, Safety of robotic general surgery in elderly patients, J Robot Surg, 2010 Aug;4(2):91-8.
- Krause A et al, Robotic-Assisted Gynecologic Surgery and Perioperative Morbidity in Elderly Women, J Minim Invasive Gynecol 23 (2016): 949-953.
- Lindfors A. Robotic vs Open Surgery for Endometrial Cancer in Elderly patients: Surgical Outcome, Survival and Cost Analysis, Int J Gynecol Cancer 28 (2018): 692-699
- De’Angelis N. Robotic Versus laparoscopic Colorectal Cancer Surgery in Elderly Patients: A Propensity Score Match Analysis. Journal of Laparoendoscopic & Advanced Surgical Techniques 28 (2018): 1334-1345.
- Palomba G, Marianna C, Pietro A, Marco M et al, Robotic versus laparoscopic colorectal surgery in elderly patients in terms of recovery time: a monocentric experience. Journal of Robotic Surgery 16 (2022): 981-987.
- Wei-Chi S, Po-Jung C, Hsiang-Lin T, Tsung-Kun C, et al. Feasibility of robot-assisted rectal surgery in elderly patients with rectal cancer. J Minim Access Surg 17 (2021): 165-174.
- Hannan E, Gerard F, Mohammad FU, Eoghan C et al, Robotic colorectal surgery in elderly patients: A single-centre experience. Int J Med Robot 18 (2022): e2431.
- Cuellar-Gomez H, Guglielmo Niccolò P, Seon-Hahn K, Cruz Vargas-DL et al, Operative and Survival Outcomes of Robotic-Assisted Surgery for Colorectal Cancer in Elderly and Very Elderly Patients: A Study in a Tertiary Hospital in South Korea. J Oncol 30 (2022): 63-71.
- https://ecis.jrc.ec.europa.eu/