Risk factors associated with dehiscence of intestinal anastomosis in patients of the University Hospital of Puebla: Retrospective, Nonexperimental Analytical study
Article Information
Marín Pardo EI, Méndez Sánchez A*, Vazquez Medina MU, Diaz Barrientos CZ, Navarro Tovar F, González González G, Linares Melo S
Department of General surgery of the University Hospital of Puebla, Benemérita Universidad Autónoma de Puebla, Mexico
*Corresponding Author: Méndez Sánchez A, Department of general surgery of the University Hospital of Puebla, Benemérita Universidad Autónoma de Puebla, Mexico.
Received: 26 March 2024; Accepted: 03 April 2023; Published: 29 April 2024
Citation: Marín Pardo EI, Méndez Sánchez A, Vazquez Medina MU, Diaz Barrientos CZ, Navarro Tovar F, González González G, Linares Melo S. Risk factors associated with dehiscence of intestinal anastomosis in patients of the University Hospital of Puebla: Retrospective, nonexperimental analytical study. Journal of Surgery and Research. 7 (2024): 159-164.
View / Download Pdf Share at FacebookAbstract
Introduction: Intestinal anastomosis is a procedure commonly used in elective and emergency surgery, the technique for its performance is subject to various factors such as: place of anastomosis, probability of anastomosis leakage, anastomose loop diameter and patient comorbidities [1]. AD represents an indicator of the quality of the surgery performed and has been the subject of multiple studies on the factors associated with said complication, especially in colorectal anastomosis.3 Since there have been very few studies carried out in our country on this subject, we decided to carry out this border study.
Objectives: To identify risk factors associated with anastomosis dehiscence in the case series.
Materials and methods: An experimental retrospective analytical study was performed on 52 patients, who underwent intestinal anastomosis, those who presented with anastomosis dehiscence and those who did not present anastomosis dehiscence, regardless of whether the procedure was urgent or was elective over 18 years, in the period from January 2016 to December 2021.
Results: 52 patients were evaluated, 16 (31%) women and 36 (69% men), of which a total of 8 people (15%) had anastomosis dehiscence, 25 (48%) were emergency surgeries, 6 (11%) had sepsis criteria (p<0.01), 6 (75%) had comorbidities (p<0.01). The ileum was the segment that presented mostly anastomosis dehiscence.
Conclusion: Our study shows that sepsis and the presence of comorbidities are the factors most associated with anastomosis dehiscence.
Keywords
Palabras Clave intestinal ischemia, Complications of arterial diseases, Abdominal sepsis, Intestinal resection, Intestinal anastomosis, Anemia, Ileum, Emergency surgery
Palabras Clave intestinal ischemia articles; complications of arterial diseases articles, abdominal sepsis articles; intestinal resection articles; intestinal anastomosis articles; anemia articles; ileum articles; emergency surgery articles.
Article Details
Introduction
Intestinal anastomosis is a procedure commonly used in elective and emergency surgery, the technique for its realization is subject to various factors such as: place of anastomosis, probability of anastomosis leakage, diameter of the loop to anastomosar and comorbidities presented by the patient [1]. As in all procedures, there is a risk of presenting complications, where anastomosis dehiscence (AD) is a feared complication that exponentially increases morbidity, mortality, hospital stay and cost of medical care [2]. AD represents an indicator of the quality of the surgery performed and has been the subject of multiple studies on the factors associated with said complication, especially in colorectal anastomosis [3]. The frequency and severity of complications may vary in relation to the site at which it occurs [4].
Nastomotic failure, or gastrointestinal fistula, was defined by Berry and Fisher in 1996 as "any communication between two epithelial intestinal surfaces (sic) after an intestinal anastomosis that causes characteristic clinical manifestations after the exposure of the peritoneal cavity to intestinal material".
Determining the risk factors that favor the presence of anastomosis dehiscence is a controversial issue, as demonstrated by the development of multiple studies with inconclusive and contradictory results. Among the factors studied are: male sex, smoking, ASA classification (American Society of Anesthesiologist), nutritional status, prolonged surgical time, intraoperative bleeding and the ability of the surgeon [5].
Despite the human and financial costs generated by the anastomosis leak, and the efforts made to reduce its incidence, the presence of leakage has not evolved in recent years. In addition, its preoperative prediction and the identification of patients at risk are not sufficiently accurate, as it is often diagnosed too late in the postoperative period [6]. Due to the few studies carried out in the Mexican population that serve as a measure of impact, it is decided to carry out this study looking for associated factors and if these are consistent with what was reported in the literature.
Objectives
General objective
To identify risk factors associated with dehiscence of intestinal anastomosis in patients of the University Hospital of Puebla.
Specific objective
- Determine the demographic characteristics of the population (patients admitted to the University Hospital of Puebla) who present dehiscence of intestinal anastomosis.
- Determine the relationship between anastomosis dehiscence and body mass index, emergency or elective surgery, abdominal sepsis, hemoglobin levels, ASA, comorbidities and gender.
- Describe whether anastomosis dehiscence is more common in manual anastomosis versus mechanical anastomosis.
- Determine which type of anastomosis has the highest dehiscence index, classifying them in: mechanical, manual, term-terminal, term-lateral, latero-terminal and lateral latero.
Material and methods
The present research was carried out in patients of the general surgery service of the University Hospital of Puebla, who underwent intestinal anastomosis during the period from January 2016 to December 2021 giving a total of 52 patients. All patients undergoing intestinal anastomosis are listed. Data were obtained using the hospital platform (Assist). A review of the medical records was carried out identifying those patients who presented with anastomosis dehiscence, and the database was filled in, separating the associated risk factors.
Inclusion criteria: eligible patients from the University Hospital of Puebla, patients in agreement with the hospital, and private patients treated in the hospital, aged between 18 and 85 years, underwent intestinal anastomosis were included, manual or mechanical, ASA rated between I and IV, and patients with documented anastomosis dehiscence.
Exclusion criteria: Patients under 18 years of age, patients undergoing intestinal anastomosis whose follow-up has not been performed at the University Hospital of Puebla, patients undergoing intestinal anastomosis in another unit, patients with incomplete records, patients with ASA V to VI classification, patients with hostile abdomen.
Elimination criteria: Patients who have died in postoperative due to cause other than intestinal anastomosis.
Statistical analysis
Sociodemographic data are presented using numbers (percentages) or medians (interquartile range [IQR]), as appropriate.
The clinical records of those subjects subjected to an intestinal anastomosis were collected, demographic variables were collected, as well as medical of the population as it is a border study in the case of the significance of the effects this will be evaluated later and assuming the sample normality when treating a population greater than N=30.
We present a table describing the sociodemographic characteristics of the population, the continuous variables as normal distributions are presented as mean (standard deviation) and in case of qualitative variables as frequency (percentage); Variables are described: table 1
|
Variables |
|
|
Sexo Sex |
• Man |
|
• Woman |
|
|
Type of surgery |
• Urgency |
|
• Elective |
|
|
ASA assessment |
• I |
|
• II |
|
|
• III |
|
|
• IV |
|
|
Comorbidities |
• Diabetes Mellitus Type 2 |
|
• Systemic Arterial Hypertension |
|
|
Type of anastomosis |
• Mechanics |
|
• Manual |
|
|
Anastomosed segment |
• Gastric |
|
• Jejunum |
|
|
• ileum |
|
|
• Colon |
|
|
Type |
• Latero-lateral |
|
• Latero-terminal |
|
|
• Lateral-term |
|
|
Age |
Years old |
|
The BMI kg/m2 |
|
|
Hemoglobin level (mg/dl) |
|
|
Surgical time |
Minutes |
Table 1: Variables.
Data were divided into two groups based on the presence or absence of anastomosis dehiscence and a bivariate analysis was performed to obtain the statistical significance of the presence of variables in the result of anastomosis dehiscence, in case of qualitative variables the statistical test of the Fisher Exact Test at 2 tails was used in case of quantitative variables, the normality of the distribution was evaluated by means of the curtosis test, and the homogeneity of the variances by means of the Barlett test in the case of those who met these assumptions, the significance of the Student T-test for unpatched samples was evaluated. The significance level was established for an alpha level of 95% with a P <0.05.
Once the variables with statistical significance were established, based on the presence of perfect concordance of results or not, medians of impact were obtained in case of perfect concordance, it was modeled in Tau-statisticsKendall B as nonparametric association strength statistic considering values >75 as very strongly associated. In the case of not perfect agreement, logistic regression was used as a method to obtain the mummy ratio of the significant variables in the bivariate analysis, in order to know the weights in a multivariate model and to know the predicted probability with respect to the change of variable; taking into account that this is neither a causality model nor a frontier study to calculate the totality of variables involved in a phenomenon, but as a methodology to obtain a result with possible medical use. The significance of the model was evaluated by the chi-square test with respect to the probability predicted by the likelihood logarithm and the goodness of fit by the Hosmer test.
Ethical considerations: This study is conducted along the lines of the Declaration of Helsinki adopted by the World Medical Assembly in 1964, the last update of which was held in Fortaleza, Brazil in October 2013; as well as the general health law enacted in 1984.
Results
A total of 52 patients were included in the final analysis, of which 8 (15%) presented anastomosis dehiscence, with a higher prevalence in males 6 (75%), 25 (48%) were emergency surgery, in 4 (50%) In 6 (75%) patients presented diabetes and systemic arterial hypertension and sepsis, the other demographic variables are presented in table 2.
|
Variable |
Population N=52 |
|
Sex |
|
|
Women |
16(31%) |
|
Men |
36 (69%) |
|
Type of surgery |
|
|
Urgency |
|
|
Elective |
25 (48%) |
|
Sepsis |
27 (52%) |
|
ASA |
6 (11%) |
|
I |
|
|
II |
2 (3.8%) |
|
III |
23 (44.3%) |
|
IV |
25 (48%) |
|
Comorbidity |
2 (3.8%) |
|
DM2 |
|
|
HAS |
15 (28%) |
|
Type of anastomosis |
25 (48%) |
|
Mechanics |
|
|
Manual |
25 (48%) |
|
Segment |
27 (51%) |
|
Gastric |
|
|
Jejunum |
3 (5.7%) |
|
Ileum |
5 (9.6%) |
|
Colon |
26 (50%) |
|
Guy |
18 (34.6%) |
|
Latero-lateral |
|
|
Latero-Terminal |
12 (23.8%) |
|
Lateral-term |
7 (13.46%) |
|
Age (years) |
33 (63.4%) |
|
BMI (kg/M2) |
58.9 (±13.4) |
|
Hemoglobin (mg/dl) |
27.2 (±4.3) |
|
Surgical time (min.) |
14.2 (±2.09 DS) |
|
166.5 (±56 min) |
Table 2: Variables and percentages found in study subjects.
In the bivariate analysis there was only statistical significance in the presence of sepsis, the presence of type 2 diabetes mellitus and hemoglobin levels. Sepsis previously occurred in 75% of cases of abdominal sepsis (p=0.0001). Type 2 diabetes mellitus occurred in 75% of patients with abdominal sepsis compared to 20% of those who did not present it (p=0.005). Hemoglobin was significantly lower in those patients with wound dehiscence (14.4 versus 13.0) (p=0.03). The difference observed in the rest of the variables was not statistically significant. These results are expressed in table 3.
|
Variable |
Dehiscence |
Value of P |
|
|
No (n=44) |
Si (n=8) |
||
|
Sex |
|||
|
Men |
30 (68%) |
6 (75%) |
1 |
|
Type of surgery |
|||
|
Urgency |
19 (43%) |
6 (75%) |
0.1 |
|
Sepsis |
0 (0%) |
6 (75%) |
<0.001 |
|
ASA |
|||
|
I |
2 (4.5%) |
0 (0%) |
0.8 |
|
II |
20 (45%) |
3 (37%) |
|
|
III |
20 (45%) |
5 (62.5%) |
|
|
IV |
2 (4.5%) |
0 (0%) |
|
|
Comorbidity |
|||
|
DM2 |
9 (20.4%) |
6 (75%) |
0.005 |
|
HAS |
19 (43%) |
6 (75%) |
0.1 |
|
Type of anastomosis |
|||
|
Mechanics |
|||
|
Manual |
21 (47%) |
4 (50%) |
0.6 |
|
Segment |
23 (52.2%) |
4 (50%) |
0.6 |
|
Gastric |
|||
|
Jejunum |
2 (4.5%) |
1 (12.5%) |
0.6 |
|
Ileum |
5 (11.3%) |
0 (0%) |
|
|
Colon |
22 (50%) |
4 (50%) |
|
|
Guy |
15 (34%) |
3 (37.5%) |
|
|
Latero-lateral |
|||
|
Latero-Terminal |
9 (20.4%) |
3 (37.5%) |
0.2 |
|
Terminus-lateral |
5 (11.3%) |
2 (25%) |
|
|
Age (years) |
30 (68%) |
3 (37.5%) |
|
|
BMI (kg/M2) |
58.7 (13.6%) |
60.2 (13.01%) |
0.7 |
|
Hemoglobin (mg/dl) |
26.8 (4.4%) |
29.2 (3.09%) |
0.1 |
|
Surgical time (min.) |
14.4 (2.08 %) |
13 (1.78%) |
0.03 |
|
164 (59.96%) |
175 (31.62%) |
0.6 |
|
Since in the sample perfect agreement of sepsis was presented in the result was obtained the statistical analysis of Tau-b of Kendall as a measure of impact which was 84%, of this it is known that 84% can be explained only by the presence of sepsis, that is, with a very strong association (Table 4).
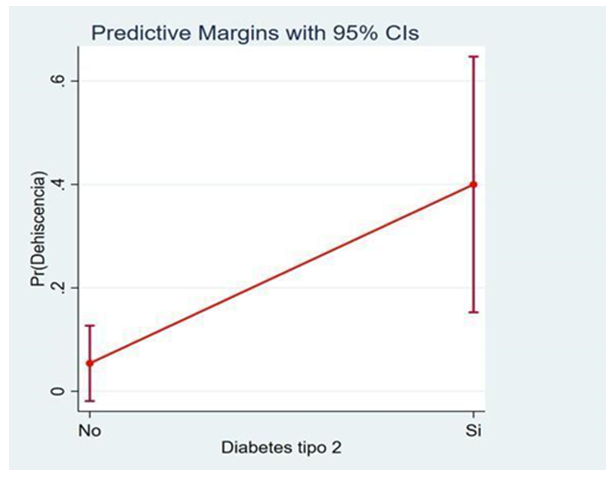
In the case of multivariate regression, it was found that in relative weights, (in this model), hemoglobin lost statistical significance, in the case of impact measurement the presence of diabetes was associated with a relative risk of 2.69 for risk of presenting dehiscence of anastomosis (95% CI 0.39-5) with a value of p=0.02, having an adequate goodness of fit of Hosmer (p=0.04). (Table 5)
In the marginal probability calculation the presence of anastomosis dehiscence when having diabetes mellitus would be in the range 10-65% with a mean of 40%. (Figure 1).
|
Sepsis |
Dehiscence |
|
|
Not |
yes |
|
|
Not |
44 (100%) |
2 (25%) |
|
Yes |
0 |
6 (75%) |
|
Fisher exact test= <0.001 |
||
|
Kendall Tau-B= 0.84 |
||
|
Asymptotic error= 0.098 |
||
Table 4: Evidence of statistical significance.
|
Variable |
OR |
IC 95% |
P |
|
Hemoglobin |
0.07 |
0.39-0.55 |
0.7 |
|
Type 2 diabetes mellitus |
2.69 |
0.39-5 |
|
|
LR Chi2 (2) = 9 P=0.01 |
|||
|
Pseudo R2= 0.2 |
|||
|
Hosmer-Lemeshow: p=0.04 |
|||
Table 5: Statistical significance of variables.
Arguing
In our case series, 15% of these patients had anastomosis dehiscence and were consistent with the literature, where the incidence of anastomosis dehiscence ranged from 0.3% to 25%. Since this complication is very common and with significant morbidity and mortality, also associated with increased days of hospital stay and therefore increasing the cost of surgical treatment, it is vital to prevent and treat this complication optimally. The dehiscence of anastomosis is usually related to peritonitis and this leads to the dismantling of the anastomosis and therefore perform a digestive shunt by means of a stoma.
In our series, the most frequent surgical indication was intestinal restitution due to ileostomy/colostomy status, in which cases dehiscence was not present. The heterogeneity of the patients treated in our hospital gives the possibility to treat patients with incipient abdominal symptoms up to cases of abdominal sepsis, being precisely abdominal sepsis the risk factor with the greatest association for the presence of anastomosis dehiscence in our study, since of the 8 patients who presented anastomosis dehiscence, 75% presented abdominal sepsis, in similarity to that reported by Alvarez Villaseñor 4, who reports as significant risk factors the presence of previous intake of drugs and abdominal sepsis.
On the other hand, it is possible to have instruments for performing mechanical anastomosis, however, unlike what was reported in other series, such as the case of Naumann et al. 21 in a meta-analysis of 7 studies with a population of 1120 patients, with a total of 1205 anastomoses, referring to the situation in an emergency environment, that is, a patient with hypotension data finding that both a mechanical stapler and a manual anastomosis did not find statistical significance between the use of one technique and the other (OR 1.53; 95% CI 0.97-2.43; p=0.070) to present with anastomosis dehiscence, localized abscess or mortality.
One of the factors strongly related to anastomosis dehiscence in various series, for example, in the one reported by Morse BC7 was malnutrition, which was determined by serum albumin levels (less than 3), however, given that 48% of our sample were emergency surgery, in addition to social security (IMSS) patients, in which case it is not generally possible to request studies such as serum albumin, not all records were found with this data, so the only way to evaluate nutritional status was with the body mass index, which in our series had an average of 27.2 kg/m2, integrating overweight diagnosis, which although conditioned technical difficulty, showed no statistically significant difference.
The comorbidities that were recorded in our study were diabetes mellitus type 2 and systemic arterial hypertension, which were present in 28% and 48% respectively. Of these pathologies, both were present in 75% of patients with anastomosis dehiscence, however, only type 2 diabetes mellitus had a statistically significant difference in the development of anastomosis dehiscence, probably because in addition to having these comorbidities, they had abdominal sepsis, diabetes mellitus being a predisposing factor for immunosuppression, which in addition to altering the own mechanisms of tissue repair, decreases neutrophil response to sepsis.
The ASA score has been associated with anastomosis dehiscence, as reported by Silva Godinez JC16, however, in this analysis, no significant difference could be found between the different ASA scores. Previously, it has been shown that the duration of the operation is related to the presence of anastomosis leak [5], finding no statistical significance in the relationship of the study.
Conclusions
Anastomosis dehiscence is a complication with significant morbidity and mortality, it should be considered in all patients undergoing anastomosis, the decision on whether to perform it or not, should be individualized to the patient’s context, the severity of their pathology, the type of hospital as well as the surgeon’s experience, among others. According to our results it should be avoided in septic patients, in which cases it is suggested to opt for a stoma. Also, in situations of elective surgery and in controlled scenarios it is suggested to optimize the general conditions of the patient, with respect to the control of comorbidities especially of type 2 diabetes mellitus and to optimize hemoglobin levels.
Conflicts of interest
All authors certify that they have no affiliation or participation in any organization or entity with any financial interest, or non-financial interest in the subject or materials discussed in this article. The authors do not declare a conflict of interest related to the study presented.
References
- Morales Maza J, Clemente Gutiérrez U, Santes O. Anastomosis intestinales. Rev Mex de Cirugía del Aparato Digestivo 6 (2017): 162-168.
- Campos SF, Ureña JA, Fuentes C, et al. Dehiscencia de anastomosis gastrointestinal. Qué hacer y qué no hacer Cir Gen 41 (2019): 243-255.
- Bannura CG, Cumsille MA, Barrera EA, et al. Factores asociados a la dehiscencia clínica de una anastomosis intestinal grapada: análisis multivariado de 610 pacientes consecutivos. Rev Chil Cir 58 (2006): 341-346.
- Álvarez AS, Prado S, Morales JI, et al. Factores asociados a dehiscencia de anastomosis intestinal. Cir Cir 89 (2021): 233-242.
- González FM, Vicente M, Gómez MJ. Factores asociados a dehiscencia en cáncer de colon. Cir Cir 87 (2019): 347-352.
- Meyer J, Naiken S, Christou N, et al. Reducing anastomotic leak in colorectal surgery: The old dogmas and the new challenges. World J Gastroenterol 25 (2019): 5017-5025.
- Golda T, Lazzara C, Zerpa C, et al. Risk factors for ileocolic anastomosis dehiscence; a cohort study. The American Journal of Surgery 12 (2004): 568
- Pacheco MA, Aldana GE, Martínez LE, et al. Incidencia de falla anastomótica en intestino delgado, colon y recto, Bogotá, Colombia. Rev Colomb Cir 32 (2017): 269-276.
- Fuentes C, Rendón J, González A. Dehiscencia de anastomosis o fístula entérica? Necesidad de definiciones precisas en la descripción de complicaciones quirúrgicas, aun en cirugía pediátrica. Gac Med Mex 151 (2015): 700- 702.
- Morse B, Simpson J, Jones Y, et al. Determination of independent predictive factors for anastomotic leak: analysis of 682 intestinal anastomoses. Am J Surg 260 (2013): 950-956.
- Leichtle SW, Mouawad NJ, Welch KB, et al. Risk factors for anastomotic leakage after colectomy. Dis Colon Rectum 55 (2012): 569-575.
- Muñoz PN, Rodríguez GM, Pérez CA, et al. Evaluación de factores de riesgo asociados a dehiscencia anastomótica en cirugía colorrectal. Análisis multivariado de 748 pacientes. Rev Chil Cir 71 (2019): 136-144.
- Gomez JM, Soto BA, Hernández M. Valoración de la cicatrización temprana en anastomosis intestinales con uso de adhesivo tisular (n-butil 2- octilcianoacrilato) versus técnica convencional. Acta Médica Grupo Ángeles 7 (2009): 137-142.
- Sciuto A, Merola G, De Palma GD, et al. Predictive factors for anastomotic leakage after laparoscopic colorectal surgery. World J Gastroenterol 24 (2018): 2247-2260.
- Gessler B, Eriksson O, Angenete E. Diagnosis, treatment, and consequences of anastomotic leakage in colorectal surgery. Int J Colorectal Dis 32 (2017): 549-556.
- Silva JC, Vásquez S, Jarquín A, et al. El estado nutricio no influye en el desarrollo de dehiscencia de anastomosis en una población mexicana. Cirujano General 35 (2017): 9-15.
- Gutiérrez A, Reyna F, Salinas R, et al. Evaluación del estado nutricional y su impacto en pacientes post operados de anastomosis intestinal. Nutrición y fuga anastomosis. Nutr Clín Diet Hosp 36 (2016): 82-88.
- Daams F, Wu Z, Lahaye MJ, et al. Prediction and diagnosis of colorectal anastomotic leakage: A systematic review of literature. World J Gastrointest Surg 6 (2014): 14-26.
- Trencheva K, Morrissey K, Wells M, et al. Identifying Important Predictors for Anastomotic Leak After Colon and Rectal Resection. Ann Surg 257 (2013): 108-111.
- Vela MA. Prevalencia, incidencia y factores asociados a dehiscencia como complicación de anastomosis colorectal en el Hospital Regional ISSSTE Puebla de enero de 2013 a diciembre de 2018. Tesis especialidad, Benemérita Universidad Autónoma de Puebla 12 (2017):1-23
- David N, Naumann MR, Annel B, et al. Stapled versus handsewintestinal anastomosis in emergency laparotomy: A systemic review and meta-analysis, surgery Apr 157 (2015): 609-618.