Reverse V Osteotomy of the Distal Humerus for the Correction of Cubitus Varus
Article Information
Mohammad Shahin Akter1*, Mst. Maksuda Khatun2, Abul Hasan1, Shahidul Islam3, Mohammed Salim Miah1, Md. Azizur Rahman4
1Department of Orthopedics, Bangabandhu Sheikh Mujib Medical College (BSMMC), Faridpur, Bangladesh
2Department of Radiology and imaging, Bangabandhu Sheikh Mujib Medical College (BSMMC), Faridpur, Bangladesh
3Department of Orthopedics and Spine Surgery, Addin Women’s Medical College Hospital, Dhaka, Bangladesh
4Ortho-Surgery, Kaliganj Upazila Health Complex, Kaliganj, Jhenaidah, Bangladesh
*Corresponding Author: Mohammad Shahin Akter, Department of Orthopedics, Bangabandhu Sheikh Mujib Medical College (BSMMC), Faridpur, Bangladesh.
Received: 06 February 2023; Accepted: 21 February 2023; Published: 28 February 2023
Citation:
Mohammad Shahin Akter, Mst. Maksuda Khatun, Abul Hasan, Shahidul Islam, Mohammed Salim Miah, Md. Azizur Rahman. Reverse V Osteotomy of the Distal Humerus for the Correction of Cubitus Varus. Journal of Orthopedics and Sports Medicine 5 (2023): 72-78.
View / Download Pdf Share at FacebookAbstract
Introduction: Cubitus varus deformity is triplanar, consisting of sagittal, coronal, and rotational components. There are numerous osteotomy techniques proposed in the past to address the correction of this deformity. Most osteotomies are aimed at correcting varus components only and are labelled as uniplanar osteotomies. The goal of the osteotomy is to correct the alignment of the elbow joint to a normal range of 5 to 15 degrees and create a stable joint. Cubitus varus deformity in children is a late complication of supracondylar humerus fracture.
Aim: The study aimed to correct the elbow so that it was anatomically and functionally identical to the opposite normal side. Methods: It is an observational study; 14 children were treated for cubitus varus using a reverse V osteotomy. The study children were treated from January 2021 to December 2021 at Faridpur Medical College and Hospital, Faridpur, Bangladesh. A total of 14 patients had sustained a supracondylar humeral fracture, two lateral condylar fractures, two medial condylar fractures, and one trans-physical separation. All 14 children were treated for cubitus varus using a reverse V osteotomy.
Result: Among the majority, about sixty percent of children were from the age range of 1-2 years. We used Oppenheim’s (1989) grading system to grade our results. This grading system has four labelled (Excellent, Good, Fair, and Poo) which are based on carrying angle (Degree) and range of movement (Degree) Table 1. Table 2 shows the assessment of the results according to modified Oppenheim’s grading system. According to our study, 11(78.57%) children had an excellent outcome without complications, and 3(21.43%) children had a good result without complications.
Conclusion: We recommend this technique as a safe, reliable, reproducible, and technically easy procedure for the correction of cubitus varus deformity.
Keywords
Reverse V Osteotomy; Distal Humerus; Cubitus Varus
Orthopedics articles Orthopedics Research articles Orthopedics review articles Orthopedics PubMed articles Orthopedics PubMed Central articles Orthopedics 2023 articles Orthopedics 2024 articles Orthopedics Scopus articles Orthopedics impact factor journals Orthopedics Scopus journals Orthopedics PubMed journals Orthopedics medical journals Orthopedics free journals Orthopedics best journals Orthopedics top journals Orthopedics free medical journals Orthopedics famous journals Orthopedics Google Scholar indexed journals Spine surgery articles Spine surgery Research articles Spine surgery review articles Spine surgery PubMed articles Spine surgery PubMed Central articles Spine surgery 2023 articles Spine surgery 2024 articles Spine surgery Scopus articles Spine surgery impact factor journals Spine surgery Scopus journals Spine surgery PubMed journals Spine surgery medical journals Spine surgery free journals Spine surgery best journals Spine surgery top journals Spine surgery free medical journals Spine surgery famous journals Spine surgery Google Scholar indexed journals Cubitus varus deformity articles Cubitus varus deformity Research articles Cubitus varus deformity review articles Cubitus varus deformity PubMed articles Cubitus varus deformity PubMed Central articles Cubitus varus deformity 2023 articles Cubitus varus deformity 2024 articles Cubitus varus deformity Scopus articles Cubitus varus deformity impact factor journals Cubitus varus deformity Scopus journals Cubitus varus deformity PubMed journals Cubitus varus deformity medical journals Cubitus varus deformity free journals Cubitus varus deformity best journals Cubitus varus deformity top journals Cubitus varus deformity free medical journals Cubitus varus deformity famous journals Cubitus varus deformity Google Scholar indexed journals Osteotomy articles Osteotomy Research articles Osteotomy review articles Osteotomy PubMed articles Osteotomy PubMed Central articles Osteotomy 2023 articles Osteotomy 2024 articles Osteotomy Scopus articles Osteotomy impact factor journals Osteotomy Scopus journals Osteotomy PubMed journals Osteotomy medical journals Osteotomy free journals Osteotomy best journals Osteotomy top journals Osteotomy free medical journals Osteotomy famous journals Osteotomy Google Scholar indexed journals Elbow joint articles Elbow joint Research articles Elbow joint review articles Elbow joint PubMed articles Elbow joint PubMed Central articles Elbow joint 2023 articles Elbow joint 2024 articles Elbow joint Scopus articles Elbow joint impact factor journals Elbow joint Scopus journals Elbow joint PubMed journals Elbow joint medical journals Elbow joint free journals Elbow joint best journals Elbow joint top journals Elbow joint free medical journals Elbow joint famous journals Elbow joint Google Scholar indexed journals Ulnar nerve dislocation articles Ulnar nerve dislocation Research articles Ulnar nerve dislocation review articles Ulnar nerve dislocation PubMed articles Ulnar nerve dislocation PubMed Central articles Ulnar nerve dislocation 2023 articles Ulnar nerve dislocation 2024 articles Ulnar nerve dislocation Scopus articles Ulnar nerve dislocation impact factor journals Ulnar nerve dislocation Scopus journals Ulnar nerve dislocation PubMed journals Ulnar nerve dislocation medical journals Ulnar nerve dislocation free journals Ulnar nerve dislocation best journals Ulnar nerve dislocation top journals Ulnar nerve dislocation free medical journals Ulnar nerve dislocation famous journals Ulnar nerve dislocation Google Scholar indexed journals Triceps articles Triceps Research articles Triceps review articles Triceps PubMed articles Triceps PubMed Central articles Triceps 2023 articles Triceps 2024 articles Triceps Scopus articles Triceps impact factor journals Triceps Scopus journals Triceps PubMed journals Triceps medical journals Triceps free journals Triceps best journals Triceps top journals Triceps free medical journals Triceps famous journals Triceps Google Scholar indexed journals Avascular necrosis articles Avascular necrosis Research articles Avascular necrosis review articles Avascular necrosis PubMed articles Avascular necrosis PubMed Central articles Avascular necrosis 2023 articles Avascular necrosis 2024 articles Avascular necrosis Scopus articles Avascular necrosis impact factor journals Avascular necrosis Scopus journals Avascular necrosis PubMed journals Avascular necrosis medical journals Avascular necrosis free journals Avascular necrosis best journals Avascular necrosis top journals Avascular necrosis free medical journals Avascular necrosis famous journals Avascular necrosis Google Scholar indexed journals Distal humeral epiphysis articles Distal humeral epiphysis Research articles Distal humeral epiphysis review articles Distal humeral epiphysis PubMed articles Distal humeral epiphysis PubMed Central articles Distal humeral epiphysis 2023 articles Distal humeral epiphysis 2024 articles Distal humeral epiphysis Scopus articles Distal humeral epiphysis impact factor journals Distal humeral epiphysis Scopus journals Distal humeral epiphysis PubMed journals Distal humeral epiphysis medical journals Distal humeral epiphysis free journals Distal humeral epiphysis best journals Distal humeral epiphysis top journals Distal humeral epiphysis free medical journals Distal humeral epiphysis famous journals Distal humeral epiphysis Google Scholar indexed journals Joint ganglia articles Joint ganglia Research articles Joint ganglia review articles Joint ganglia PubMed articles Joint ganglia PubMed Central articles Joint ganglia 2023 articles Joint ganglia 2024 articles Joint ganglia Scopus articles Joint ganglia impact factor journals Joint ganglia Scopus journals Joint ganglia PubMed journals Joint ganglia medical journals Joint ganglia free journals Joint ganglia best journals Joint ganglia top journals Joint ganglia free medical journals Joint ganglia famous journals Joint ganglia Google Scholar indexed journals Osteoarthritis articles Osteoarthritis Research articles Osteoarthritis review articles Osteoarthritis PubMed articles Osteoarthritis PubMed Central articles Osteoarthritis 2023 articles Osteoarthritis 2024 articles Osteoarthritis Scopus articles Osteoarthritis impact factor journals Osteoarthritis Scopus journals Osteoarthritis PubMed journals Osteoarthritis medical journals Osteoarthritis free journals Osteoarthritis best journals Osteoarthritis top journals Osteoarthritis free medical journals Osteoarthritis famous journals Osteoarthritis Google Scholar indexed journals Fishtail osteotomy articles Fishtail osteotomy Research articles Fishtail osteotomy review articles Fishtail osteotomy PubMed articles Fishtail osteotomy PubMed Central articles Fishtail osteotomy 2023 articles Fishtail osteotomy 2024 articles Fishtail osteotomy Scopus articles Fishtail osteotomy impact factor journals Fishtail osteotomy Scopus journals Fishtail osteotomy PubMed journals Fishtail osteotomy medical journals Fishtail osteotomy free journals Fishtail osteotomy best journals Fishtail osteotomy top journals Fishtail osteotomy free medical journals Fishtail osteotomy famous journals Fishtail osteotomy Google Scholar indexed journals Osteotomies articles Osteotomies Research articles Osteotomies review articles Osteotomies PubMed articles Osteotomies PubMed Central articles Osteotomies 2023 articles Osteotomies 2024 articles Osteotomies Scopus articles Osteotomies impact factor journals Osteotomies Scopus journals Osteotomies PubMed journals Osteotomies medical journals Osteotomies free journals Osteotomies best journals Osteotomies top journals Osteotomies free medical journals Osteotomies famous journals Osteotomies Google Scholar indexed journals Reverse V osteotomy articles Reverse V osteotomy Research articles Reverse V osteotomy review articles Reverse V osteotomy PubMed articles Reverse V osteotomy PubMed Central articles Reverse V osteotomy 2023 articles Reverse V osteotomy 2024 articles Reverse V osteotomy Scopus articles Reverse V osteotomy impact factor journals Reverse V osteotomy Scopus journals Reverse V osteotomy PubMed journals Reverse V osteotomy medical journals Reverse V osteotomy free journals Reverse V osteotomy best journals Reverse V osteotomy top journals Reverse V osteotomy free medical journals Reverse V osteotomy famous journals Reverse V osteotomy Google Scholar indexed journals Valgus angulation articles Valgus angulation Research articles Valgus angulation review articles Valgus angulation PubMed articles Valgus angulation PubMed Central articles Valgus angulation 2023 articles Valgus angulation 2024 articles Valgus angulation Scopus articles Valgus angulation impact factor journals Valgus angulation Scopus journals Valgus angulation PubMed journals Valgus angulation medical journals Valgus angulation free journals Valgus angulation best journals Valgus angulation top journals Valgus angulation free medical journals Valgus angulation famous journals Valgus angulation Google Scholar indexed journals
Article Details
1. Introduction
Corrective osteotomy of the distal humerus is the procedure of choice, as it is most successful in reducing symptoms and recurrence of cubitus varus deformity. The goal of the osteotomy is to correct the alignment of the elbow joint to a normal range of 5 to 15 degrees and create a stable joint. Cubitus varus deformity in children is a late complication of supracondylar humerus fracture. Malunion is the primary cause [1]. Most patients usually achieve normal elbow function after fracture healing. The deformity results in an unsightly appearance. Cosmesis is the primary concern of the child’s parents for deformity correction [2]. Although considered a cosmetic issue, many long-term complications of this deformity have been reported. These include ulnar nerve dislocation, ulnar neuropathy, snapping of the medial head of the triceps, secondary distal humeral or lateral condylar fracture, avascular necrosis of the distal humeral epiphysis, joint ganglia, osteoarthritis, posterior dislocation of the radial head, and posterolateral rotatory instability [3]. Cubitus varus deformity is triplanar, consisting of sagittal, coronal, and rotational components. There are numerous osteotomy techniques proposed in the past to address the correction of this deformity. Most osteotomies are aimed at correcting varus components only and are lddddddd as uniplanar osteotomies. Biplanar osteotomies correct both sagittal and coronal malalignment. Tridimensional osteotomies tend to correct rotational malalignment in addition to hyperextension and varus components. In a systematic review, Solfelt et al. [4] reported an overall complication rate of 14.5% and a poor outcome rate of 12.2% with the corrective procedures. The residual varus was the most common complication (5.9%), followed by nerve injuries (2.5%), infection (2.5%), and re-operation (2.3%). There was no single technique found to be safe and highly effective. To date, no standard gold technique gives the maximum possible deformity correction and cosmetic appearance that satisfies patient caretakers and minimizes complications. We used a modified reverse V osteotomy (fishtail osteotomy) with the calculated medial translation of distal fragments to correct varus and sagittal plane deformity and to prevent lateral condyle prominence. Yun et al. [5] described reverse V osteotomy (fixed by cross-pinning and wiring) for treating cubitus varus. This technique is advantageous over step-cut osteotomy because it provides more space for fixation over the distal segment. This simple technique provides adequate stability of the step cut with minimal complications. This study aims to report the clinical, radiological, and cosmetic outcomes of the modified reverse V osteotomy technique. The surgery aimed to correct the elbow so that it was anatomically and functionally identical to the opposite normal side.
2. Methodology and Materials
It is an observational study, a total of 14 children were treated for cubitus varus using a reverse V osteotomy. The study children were treated from January 2021 to December 2021 at Faridpur Medical College and Hospital, Faridpur, Bangladesh. A total of 14 patients had sustained a supracondylar humeral fracture, two a lateral condylar fractures, two a medial condylar fractures and one trans-physical separation. All the children had good elbow function with a full range of movement. The indication for surgery in all was cosmetic deformity.
2.1 Inclusion criteria:
- All patients had a childhood humeral fracture history.
- Patients were aged under <15 years.
2.2 Operation procedure:
Before planning the osteotomy, full-length radiographs of both upper limbs were taken with the elbow in full extension and the forearm in full supination. The method described by Oppenheim et al. was used to determine the humeral-elbow-wrist angle in both arms [6-10]. Valgus angulation was described as positive (+), and varus angulation as unfavourable (-). The amount of correction required was determined by adding the valgus angulation of the typical side to the varus angulation of the deformed side (Figure 1).
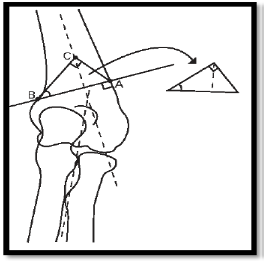
Figure 1: The line AB is perpendicular to the lateral supracondylar ridge located 5 mm to 10 mm above the olecranon fossa. Point C is determined proximal to line AB by the angle ABC (angle to be corrected) and angle ACB (which is always 90°).
The line AB is perpendicular to the lateral supracondylar ridge located 5 mm to 10 mm above the olecranon fossa. Point C is determined proximal to line AB by the angle ABC (angle to be corrected) and angle ACB (which is always 90°) (Figure 1). After removal of the triangle ABC, the distal humerus is rotated laterally and translated medially, so that point A comes to meet point C (Figure 2).
The humeral-elbow wrist angle is measured on the standard elbow, and the meeting point X of the axes of the humerus and forearm is located (Figure 3). Corrected construct with no medial or lateral prominence so that X and Y coincide (Figure 4). Corrected construct with lateral prominence (Figure 5). Point Y shows the intersection point between a line perpendicular to the forearm axis drawn from point X and the humeral axis. Y is medial to X, and point C must be moved medially by the distance X-Y to correct the lateral prominence. Corrected construct with medial prominence (Figure-6). Y is lateral to X, and point C must be moved laterally by the distance X-Y to correct the medial prominence. Which intersected the second line at 90°C This point of intersection was marked as point C (Figure 1). Thus, a triangle was formed with the angle ABC being the angle of the desired correction and the angle ACB being 90°. This triangle, which was then cut from the paper outline, was the area to be resected during surgery (Figure 1). After removal of this triangle, the entire distal humerus and forearm were rotated laterally and translated medially such that point A came to meet point C (Figure 2). This technique converted the humeral-elbow wrist angle to the normal valgus of the opposite elbow.
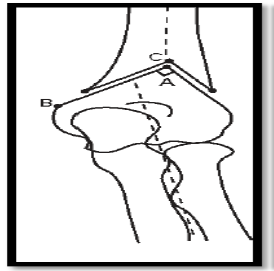
Figure 2: After removal of the triangle ABC, the distal humerus is rotated laterally and translated medially, so that point A comes to meet point C.
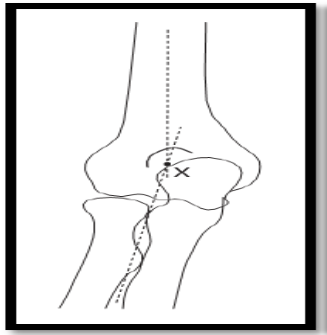
Figure 3: The humeral-elbow wrist angle is measured on the standard elbow, and the meeting point X of the axes of the humerus and forearm is located.
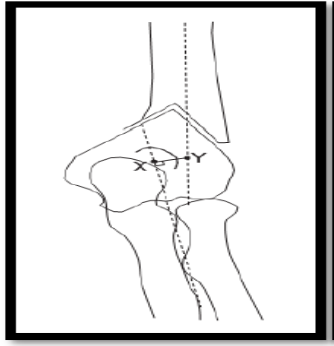
Figure 4: Corrected construct with no medial or lateral prominence so that X and Y coincide.
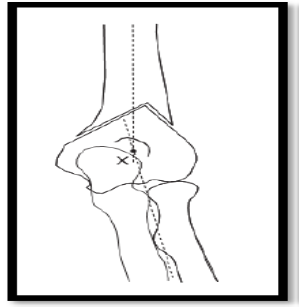
Figure 5: Corrected construct with lateral prominence.
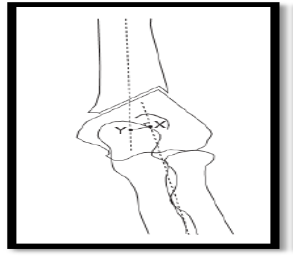
Figure 6: Point Y shows the intersection point between a line perpendicular to the forearm axis drawn from point X and the humeral axis. Y is medial to X, and point C must be moved medially by the distance X-Y to correct the lateral prominence. Corrected construct with medial prominence.
Diagrams of the pre-operative planning for the correction of varus. The line AB is perpendicular to the lateral supracondylar ridge located 5 mm to 10 mm above the olecranon fossa. Point C is proximal to line AB by the angle ABC (angle to be corrected) and angle ACB (Always 90°). After removal of the triangle ABC, the distal humerus is rotated laterally and translated medially, so that point A comes to meet point C. A line at right angles to the forearm axis was drawn from point X and crossed the humeral axis point at Y. Point C of the triangle ABC had to be moved medially or laterally by the distance X to Y for lateral or medial translation, respectively. This led to a slight change in the location of points A, B, and C but did not change the desired angles. Method of osteotomy and fixation. The surgery was performed under tourniquet control with the patient in the lateral position. The elbow was flexed to 90°, and a posterolateral approach was used. A longitudinal skin incision about 6 cm to 8 cm was made over the posterolateral aspect of the distal humerus. After superficial dissection, the triceps tendon was elevated from the lateral aspect to expose the distal humerus. The lateral supracondylar ridge was identified, and the point a marked. We used a small goniometer intra-operatively to construct the pre-operatively planned triangle. The first, second, and third osteotomy cuts were performed according to the pre-operative measurements with an oscillating saw and osteotomy. The triangular area ABC was resected, and the distal humerus and forearm rotated laterally to correct the varus deformity. Fixation was achieved with two lateral cross-wires and wiring, with care to avoid injury to the ulnar nerve. Postoperatively, a posterior elbow splint was applied in 90° of flexion. Active exercises were started two weeks after surgery.
3. Result
This observational study was conducted with 14 children treated for cubitus varus using a reverse V osteotomy. All children had a childhood humeral fracture. Among the majority, about sixty percent of children were from the age range 1-2 years, 5(35.71%) children were from the age range 2-3 years, and only one child was from 0-1 years (Table 3). Table 4 shows the age distribution of the children studied, where 7(50%) children were from the age range 7-10 years, 5(35.71%) children were from the age range 3-6 and only two children under fifteen years. In our study, there are 9(64.29%) children were male, and 5(35.71%) children were female (Figure 7). We used Oppenheim’s (1989) grading system to grade our results. This grading system has four grades (Excellent, Good, Fair, and Poo) which are based on carrying angle (Degree) and range of movement (Degree) (Table 1). Table 2 shows the assessment of the results according to modified Oppenheim’s grading system (Table 5). According to our study, 11(78.57%) children had an excellent outcome without complications, and 3(21.43%) children had a good result without complications (Figure 8-10).
|
Grade |
Carrying angle (Degree) |
Range of movement (Degree) |
|
Excellent |
0 |
0 |
|
Good |
0-5 |
45200 |
|
Fair |
45205 |
44136 |
|
Poor |
>10 |
>20 |
Table 1: The grading system of Oppenheim (1989).
|
Outcomes |
Frequency |
Percentage |
Complication |
|
Excellent |
11 |
78.57 |
No |
|
Good |
3 |
21.43 |
No |
Table 2: Assessment of the results according to a modified Oppenheim et al. [11] system.
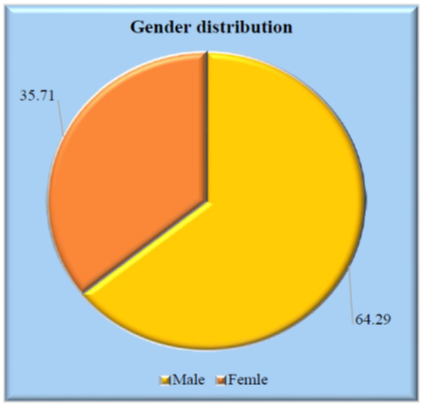
Figure 7: Gender distribution of the study children.
|
Age range (Years) |
Frequency |
Percentage |
|
0-1 |
1 |
7.14 |
|
44958 |
8 |
57.14 |
|
44987 |
5 |
35.71 |
Table 3: Age distribution of the patients based on childhood humeral fracture.
|
Age range (Years) |
Frequency |
Percentage |
|
45080 |
5 |
35.71 |
|
45206 |
7 |
50 |
|
≤15 |
2 |
14.29 |
Table 4: Age distribution of the study children during the study.
|
Variables |
Frequency |
Percentage |
|
Upper |
2 |
14.29 |
|
Middle |
4 |
28.57 |
|
Lower |
8 |
57.14 |
Table 5: Socio-demographical status of the study children.
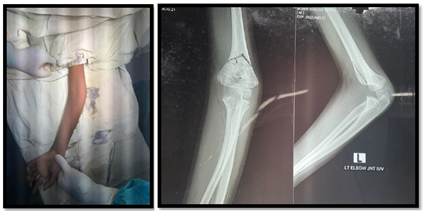
Figure 8: Pre-operative digital photographs of the patients.

Figure 9: Digital photographs during operation.
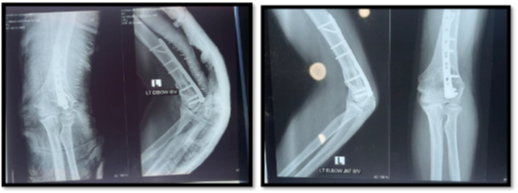
Figure 10: Post-operative photographs of the patients.
4. Discussion
The surgical techniques described for the correction of cubitus varus differ in their approach to the distal humerus, the method of osteotomy, and the type of fixation [6-13]. The standard surgical approaches to the distal humerus are lateral, medial, posterolateral, and posterior [14-22]. In our study, we used a posterolateral approach since we thought it was more cosmetic than the other alternatives. Lateral closing-wedge, medial opening-wedge, step-cut, and dome-shaped osteotomies have been described [6-16]. In 1988, DE Rosa and Graziano [6] described a step-cut osteotomy for the correction of cubitus varus. This was based on the precise cutting of the wedge so that a cortical spike on the distal fragment allowed fixation by a single cortical screw. This functioned in the same way as an intact periosteal hinge, allowing control of the osteotomy. We believe the described technique has significant advantages over the original step-cut osteotomy. The osteotomy is performed at a higher level, providing better bone fixation. It also provides more space for fixation of the distal fragment so that if performed in an adult, a reconstruction plate or a dynamic compression plate can be used with more than two screws in the distal fragment. Although the original step-cut osteotomy provided some stability because of its configuration, the cortical beak was too narrow and prone to fracture or cut out of the screw. Our osteotomy is inherently stable because of its firm wedge fit with adequate bony columns on both the medial and lateral sides. A lateral prominence due to the translation of the distal fragment is a frequent cause of poor cosmetic results [18-20]. A Lazy-S or a Z-deformity is commonly seen. Wong et al. [20] reported a lateral condylar prominence in 14 of the 22 patients in their series. They suggested that this might remodel with time. However, Ippolito et al. [19] in a long-term follow-up of corrective osteotomy for cubitus varus, described the persistence of this deformity at the final follow-up [19]. Levine et al. [15] pointed out the importance of medial displacement of the distal humerus to decrease the prominence of the Post-operative a) anteroposterior and b) lateral radiographs six weeks after the osteotomy showing good healing and fixation by crossed K- wires inserted from the lateral side with additional wiring lateral humeral condyle. The amount of displacement was decided by the gross appearance of the operation. However, medial displacement disrupted the periosteum on the medial side, leading to instability and difficulty with fixation. Dome osteotomy has been popularized by Japanese surgeons and allows the residual prominence of the lateral condyle to be corrected by rotation in both the coronal and horizontal planes [7,12,23]. However, the decision regarding the exact amount of translation required is based on the surgeon's intraoperative assessment [15,21,23]. There is no provision for pre-operative calculation, and there is always a chance that over or under-translation may occur. Our technique of pre-operative planning can prevent lateral prominence by precisely calculating the location of point C of the osteotomy. Various methods of fixation of the osteotomy, both internal and external, have been described [6]. Kirschner (K-) wire fixation is simple, can be used in a child with an open physics and can be easily removed after the union. However, external immobilization for three to five weeks is usually recommended with simple K-wire fixation [23]. Plate and screw fixation offers the best stability and allows early elbow movement. [11] Usually, there is an insufficient length for the fixation of the distal fragment [11-17]. The loss of fixation may complicate De Rosa and Graziano's [6] use of a cortical screw because of a fracture of the narrow beak used for fixation. External fixation may be in the form of a simple uniplanar fixator or an Ilizarov ring fixator [7,9,15,16]. These may have some advantages but can be inconvenient and uncomfortable for the child [7,15]. Our technique of K-wire fixation was modified to increase stability. Both cross-pins were inserted from the lateral side, reducing the chance of iatrogenic injury to the ulnar nerve. This configuration provided resistance to varus and valgus forces at the osteotomy site [25]. We believe that additional wiring of the K-wires enhanced the stability of the construct. Pre-operative clinical appearance of the children's left/right sided cubitus Varus, b) pre-operative anteroposterior radiograph (right) showing a varus deformity of 22° compared with the average right side (left), c) post-operative AP radiographs and d) photograph showing the good cosmetic result.
5. Conclusion and Recommendations
In conclusion, we recommend this technique as a safe, reliable, reproducible, and technically easy procedure for the correction of cubitus varus deformity.
Limitations of the study:
The limitations of our study include a small sample size; no comparison was made with other established techniques in this study.
Funding:
No funding sources
Conflict of interest:
None declared
Ethical approval:
The study was approved by the Institutional Ethics Committee.
References
- Høyer A. Treatment of supracondylar fracture of the humerus by skeletal traction in an abduction splint. JBJS 34 (1952): 623-637.
- Labelle H, Bunnell WP, Duhaime M, et al. Cubitus varus deformity following supracondylar fractures of the humerus in children. Journal of pediatric orthopedics 2 (1982): 539-546.
- O'Driscoll SW, Spinner RJ, McKee MD, et al. Tardy posterolateral rotatory instability of the elbow due to cubitus varus. JBJS 83 (2001): 1358-1369.
- Solfelt DA, Hill BW, Anderson CP, et al. Supracondylar osteotomy for the treatment of cubitus varus in children: a systematic review. The bone and joint journal 96 (2014): 691-700.
- Yun YH, Shin SJ, Moon JG. Reverse V osteotomy of the distal humerus for the correction of cubitus varus. The Journal of Bone and Joint Surgery. British volume 89 (2007): 527-531.
- DeRosa GP, Graziano GP. A new osteotomy for cubitus varus. Clinical orthopaedics and related research 1 (1988): 160-165.
- Kanaujia RR, Ikuta Y, Muneshige H, et al. Dome osteotomy for cubitus varus in children. Acta Orthopaedica Scandinavica 59 (1988): 314-317.
- Kim HS, Jahng JS, Han DY, et al. Modified step-cut osteotomy of the humerus. Journal of Pediatric orthopedics Part B 7 (1998): 162-166.
- Koch PP, Exner GU. Supracondylar medial open wedge osteotomy with external fixation for cubitus varus deformity. Journal of Pediatric Orthopaedics B 12 (2003): 116-122.
- Laupattarakasem W, Mahaisavariya B, Kowsuwon W, et al. Pentalateral osteotomy for cubitus varus. Clinical experiences of a new technique. The Journal of Bone and Joint Surgery British 71 (1989): 667-670.
- Oppenheim WL, Clader TJ, Smith C, et al. Supracondylar humeral osteotomy for traumatic childhood cubitus varus deformity. Clinical orthopaedics and related research 1 (1984): 34-39.
- Uchida Y, Ogata K, Sugioka Y. A new three-dimensional osteotomy for cubitus varus deformity after supracondylar fracture of the humerus in children. Journal of pediatric orthopedics. 1991 May 1; 11(3):327-31.
- French PR. Varus deformity of the elbow following supracondylar fractures of the humerus in children. The Lancet. 1959 Sep 26;274(7100):439-41.
- Carlson Jr SC, Rosman MA. Cubitus varus: a new and simple technique for correction. Journal of Pediatric Orthopaedics. 1982 Jan 1;2(2):199-201.
- Levine MJ, Horn BD, Pizzutillo PD. Treatment of posttraumatic cubitus varus in the pediatric population with humeral osteotomy and external fixation. Journal of Pediatric Orthopaedics. 1996 Sep 1;16(5):597-601.
- Karatosun V, Alekberov C, Alici E, Ardiç CO, Aksu G. Treatment of cubitus varus using the Ilizarov technique of distraction osteogenesis. The Journal of Bone and Joint Surgery. British volume. 2000 Sep;82(7):1030-3.
- Bellemore MC, Barrett IR, Middleton RW, Scougall JS, Whiteway DW. Supracondylar osteotomy of the humerus for correction of cubitus varus. The Journal of Bone and Joint Surgery. British volume. 1984 Aug;66(4):566-72.
- Barrett IR, Bellemore MC, Kwon YM. Cosmetic results of supracondylar osteotomy for correction of cubitus varus. Journal of Pediatric Orthopaedics. 1998 Jul 1;18(4):445-7.
- Ippolito E, Moneta MR, d'Arrigo C. Post-traumatic cubitus varus. Long-term follow-up of corrective supracondylar humeral osteotomy in children. The Journal of Bone and Joint surgery. American Volume. 1990 Jun 1;72(5):757-65.
- Wong HK, Lee EH, Balasubramaniam P. The lateral condylar prominence. A complication of supracondylar osteotomy for cubitus varus. The Journal of bone and joint surgery. British volume. 1990 Sep; 72(5):859-61.
- Tien YC, Chih HW, Lin GT, Lin SY. Dome corrective osteotomy for cubitus varus deformity. Clinical Orthopaedics and Related Research®. 2000 Nov 1; 380:158-66.
- Blasier RD. The triceps-splitting approach for repair of distal humeral malunion in children. A report of a technique. American Journal of Orthopedics (Belle Mead, NJ). 1996 Sep 1;25(9):621-4.
- Kumar K, Sharma VK, Sharma R, Maffulli N. Correction of cubitus varus by French or dome osteotomy: a comparative study. Journal of Trauma and Acute Care Surgery. 2000 Oct 1;49(4):717-21.
- Graham B, Tredwell SJ, Beauchamp RD, Bell HM. Supracondylar osteotomy of the humerus for correction of cubitus varus. Journal of pediatric orthopedics. 1990 Mar 1;10(2):228-31.
- Zionts LE, McKellop HA, Hathaway R. Torsional strength of pin configurations used to fix supracondylar fractures of the humerus in children. The Journal of Bone and Joint surgery. American Volume. 1994 Feb 1;76(2):253-6.
