Retrospective analysis of Peroral Endoscopic Myotomy (POEM) for the treatment of Achalasia at Ordensklinikum Linz
Article Information
Rafael Wiedmer Chaparro1, Teresa Fritz1,2, Georg Spaun2, Alexander Ziachehabi2, Rainer Schöfl1,2*
1Medical Faculty, Johannes Kepler University Linz, Austria
2Oncology Centre, Ordensklinikum Linz, Austria
*Corresponding author: Rainer Schöfl, Medical Faculty, Johannes Kepler University Linz, Austria.
Received: 27 May 2021; Accepted: 04 June 2021; Published: 15 June 2021
Citation: Rafael Wiedmer Chaparro, Teresa Fritz, Georg Spaun, Alexander Ziachehabi, Rainer Schöfl. Retrospective analysis of Peroral Endoscopic Myotomy (POEM) for the treatment of Achalasia at Ordensklinikum Linz. Journal of Surgery and Research 4 (2021): 315-322.
View / Download Pdf Share at FacebookAbstract
Background: Peroral endoscopic myotomy (POEM) is a minimally invasive procedure for treatment of achalasia. We analyze success, complications and learning curve in a consecutive series in our hospital.
Patients and Methods: Our retrospective analysis comprises all patients with achalasia, who were treated from 2015 until 2018 with POEM. Preoperative evaluation was done with history, high resolution manometry, EGD and video-cinematography. Reevaluation was performed six weeks after POEM with EGD and a history was taken. 43 patients were treated with POEM, 22 (52%) females, 21 (49%) males. The mean age was 55 (17-84) years. Six patients (14%) had been treated with injection of botulinum toxin, 12 patients (28%) with balloon dilatation before. According to Chicago classification 30 patients (85.7%) suffered from type II, four patients (11%) from type III and two patients (6%) from type I. The mean length of myotomy was 8.5±0.5cm and was extended 2cm beyond the gastroesophageal junction.
Results: In 36 procedures with complete data the initial success rate was 92%, defined as Eckardt Score ≤3. Three patients (8%) suffered from recurrent symptoms later. Eckardt Score was reduced from 7.0±0.3 to 1.0±0.2 after POEM (p<0,0001). We observed five complications (11%), which resolved with conservative treatment. Sufficient information on postinterventional reflux disease was only available from 24 patients: seven patients (29%) had a new erosive esophagitis, two patients reported typical symptoms without esophagitis. The complication rate decreased within four years from 25% to 0. A similar phenomenon was observed with recurrencies (learning curve).
Conclusion: Peroral endoscopic myotomy is an effective and safe method for the treatment of achalasia. The learning curve is relatively flat.
Keywords
Minimally invasive, Peroral endoscopic myotomy, Achalasia
Minimally invasive articles; Peroral endoscopic myotomy articles; Achalasia articles
Minimally invasive articles Minimally invasive Research articles Minimally invasive review articles Minimally invasive PubMed articles Minimally invasive PubMed Central articles Minimally invasive 2023 articles Minimally invasive 2024 articles Minimally invasive Scopus articles Minimally invasive impact factor journals Minimally invasive Scopus journals Minimally invasive PubMed journals Minimally invasive medical journals Minimally invasive free journals Minimally invasive best journals Minimally invasive top journals Minimally invasive free medical journals Minimally invasive famous journals Minimally invasive Google Scholar indexed journals Peroral endoscopic myotomy articles Peroral endoscopic myotomy Research articles Peroral endoscopic myotomy review articles Peroral endoscopic myotomy PubMed articles Peroral endoscopic myotomy PubMed Central articles Peroral endoscopic myotomy 2023 articles Peroral endoscopic myotomy 2024 articles Peroral endoscopic myotomy Scopus articles Peroral endoscopic myotomy impact factor journals Peroral endoscopic myotomy Scopus journals Peroral endoscopic myotomy PubMed journals Peroral endoscopic myotomy medical journals Peroral endoscopic myotomy free journals Peroral endoscopic myotomy best journals Peroral endoscopic myotomy top journals Peroral endoscopic myotomy free medical journals Peroral endoscopic myotomy famous journals Peroral endoscopic myotomy Google Scholar indexed journals Achalasia articles Achalasia Research articles Achalasia review articles Achalasia PubMed articles Achalasia PubMed Central articles Achalasia 2023 articles Achalasia 2024 articles Achalasia Scopus articles Achalasia impact factor journals Achalasia Scopus journals Achalasia PubMed journals Achalasia medical journals Achalasia free journals Achalasia best journals Achalasia top journals Achalasia free medical journals Achalasia famous journals Achalasia Google Scholar indexed journals reflux disease articles reflux disease Research articles reflux disease review articles reflux disease PubMed articles reflux disease PubMed Central articles reflux disease 2023 articles reflux disease 2024 articles reflux disease Scopus articles reflux disease impact factor journals reflux disease Scopus journals reflux disease PubMed journals reflux disease medical journals reflux disease free journals reflux disease best journals reflux disease top journals reflux disease free medical journals reflux disease famous journals reflux disease Google Scholar indexed journals Gastroesophageal reflux diseases articles Gastroesophageal reflux diseases Research articles Gastroesophageal reflux diseases review articles Gastroesophageal reflux diseases PubMed articles Gastroesophageal reflux diseases PubMed Central articles Gastroesophageal reflux diseases 2023 articles Gastroesophageal reflux diseases 2024 articles Gastroesophageal reflux diseases Scopus articles Gastroesophageal reflux diseases impact factor journals Gastroesophageal reflux diseases Scopus journals Gastroesophageal reflux diseases PubMed journals Gastroesophageal reflux diseases medical journals Gastroesophageal reflux diseases free journals Gastroesophageal reflux diseases best journals Gastroesophageal reflux diseases top journals Gastroesophageal reflux diseases free medical journals Gastroesophageal reflux diseases famous journals Gastroesophageal reflux diseases Google Scholar indexed journals dysphagia articles dysphagia Research articles dysphagia review articles dysphagia PubMed articles dysphagia PubMed Central articles dysphagia 2023 articles dysphagia 2024 articles dysphagia Scopus articles dysphagia impact factor journals dysphagia Scopus journals dysphagia PubMed journals dysphagia medical journals dysphagia free journals dysphagia best journals dysphagia top journals dysphagia free medical journals dysphagia famous journals dysphagia Google Scholar indexed journals postoperative reflux symptoms articles postoperative reflux symptoms Research articles postoperative reflux symptoms review articles postoperative reflux symptoms PubMed articles postoperative reflux symptoms PubMed Central articles postoperative reflux symptoms 2023 articles postoperative reflux symptoms 2024 articles postoperative reflux symptoms Scopus articles postoperative reflux symptoms impact factor journals postoperative reflux symptoms Scopus journals postoperative reflux symptoms PubMed journals postoperative reflux symptoms medical journals postoperative reflux symptoms free journals postoperative reflux symptoms best journals postoperative reflux symptoms top journals postoperative reflux symptoms free medical journals postoperative reflux symptoms famous journals postoperative reflux symptoms Google Scholar indexed journals
Article Details
1. Introduction
Peroral endoscopic myotomy is a minimally invasive procedure for the treatment of achalasia. We analyzed the outcome of POEM at Ordensklinikum Linz and, based on our experience, evaluated the safety and efficacy of the method.
2. Method
This retrospective data analysis included all achalasia patients treated with POEM from January 2015 to August 2018 at Ordensklinikum Linz. The preoperative evaluation included a high-resolution manometry (Chicago classification), EGD (esophagogastroduodenoscopy), video cinematography, and an assessment of the patients’ clinical symptoms (Eckardt score) [1,2]. We performed POEM in endotracheal anesthesia with CO2 insufflation. After submucosal injection, a mucosal incision was performed about 12cm above the cardia, and a submucosal tunnel was created beyond the cardia into the proximal portion of the stomach. The inner annular muscle was then transected from 2cm distal to the cardia in proximal direction, to about 3cm below the mucosal incision. The longitudinal muscles were preserved. Finally, the entrance of the tunnel was closed with clips. Follow-up investigations at 6 weeks after POEM consisted of a control gastroscopy and an assessment of clinical symptoms.
3. Results
Forty-three consecutive patients treated with POEM were evaluated; 22 (51.8%) were women and 21 (48.8%) were men. The patients’ mean age was 55.1 years (range, 17 to 84 years). Six patients (13.9%) had undergone previous treatment with botulinum toxin injections, and 12 patients (27.9%) with pneumatic balloon dilatation. In accordance with the Chicago classification, 30 patients (85.7%) had type II achalasia, 4 (11.4%) had type III achalasia, and 2 patients (5.7%) had type I achalasia. The mean myotomy length was 8.5 cm ± 0.5, and extended to 2 cm beyond the gastroesophageal junction. Of 36 interventions (including follow-up investigations) that could be evaluated, initial treatment success (defined as an Eckardt score < 3) was achieved in 33 cases (91.7%). Three patients developed recurrent disease. Overall, the Eckardt score was reduced significantly from 7.0 ± 0.3 to 1.0 ± 0.2 (p<0.0001) post-POEM. We observed 5 complications (11.4%; arterial bleeding in 2 patients, pneumothorax in 2 patients, and pneumonia in 1 patient), all of which could be managed by conservative treatment. With regard to de novo gastroesophageal reflux disease postoperatively, we were able to evaluate 24 datasets. Nine patients (37.5%) had erosive esophagitis or symptomatic reflux disease. Grade A (20.8%) and grade B (8.3%) erosive esophagitis according to the Los Angeles classification were diagnosed by endoscopy in 7 patients. A further 2 patients reported typical symptoms of reflux disease (NERD).
4. Discussion
In our analysis, peroral endoscopic myotomy was associated with an initial treatment success rate of 91.7% (n=33). Treatment success was defined as an Eckardt score of ≤3 at 6 weeks post-POEM. The procedure resulted in a significant reduction of the Eckardt score (7.0 ± 0.3 vs. 1.0 ± 0.2; p<0.0001). Disease recurrence was observed in 3 patients (8.3%). In a prospective study comprising 500 patients, Inoue et al. reported a treatment success rate of >90% and a reduction of the mean ES from 6.0 to 1.0. In a recent randomized controlled study, the authors registered initial success rates of 92% [3]. In two randomized controlled studies, the authors reported initial treatment success rates of about 92% [4,5]. We registered a complication rate of 11.6%. Corresponding figures 1-5 and tables 1,2 in recent studies varied from 0% to 30% because we lack a consensus regarding the definition of complications. The study most similar to ours is a prospective investigation of 500 patients, conducted by Inoue et al., who registered a complication rate of 3.2%. A retrospective analysis of 1300 patients treated with POEM in Japan reported a complication rate of 3.7% [3-5]. In our study, complication rates increased with age (46-60 years 10% vs. 61-75 years 15.4% vs. 76-90 years 28.6%). Younger patients (<45 years) had no complications. This is attributed to the greater vulnerability of tissue and the generally reduced regenerative capacity with advancing age. The discrepancy between our complication rates and those reported earlier is best explained by the small sample size, missing data sets due to the retrospective nature of the study, and the learning curve related to the complexity of the method. The lattermost factor is confirmed by complication rates in the individual years of treatment. Complication rates fell successively from 25% and 20% in the first two years to 8.3% in 2017 and 0% in 2018. The falling complication rates over time may be viewed as a manifestation of the learning curve.
In a prospective study of 40 patients treated with POEM, procedure time and the incidence of inadvertent mucosotomy were investigated in order to define a learning curve. Mastery of the operative technique in POEM has been evidenced by a decrease in both parameters; these remained constant in endoscopists who had performed more than 20 procedures [6,7]. In a similar prospective study comprising 93 patients, the procedure time plateaued and mastery of technique was achieved after 60 POEMs [8]. Gastroesophageal reflux diseases after the procedure was observed in 37.5% of cases, defined as the endoscopic diagnosis of erosive reflux disease or the presence of typical clinical symptoms. The body of published data concerning the development of reflux disease post-POEM is very diverse. In a recent systematic review, 1542 POEMs were analyzed and reflux esophagitis was established in 35.3% of cases. In the previously mentioned multicenter study from Japan comprising 1300 interventions, erosive reflux esophagitis was observed in 63% of cases and typical reflux symptoms in 15% [3,9]. In summary, our results concur with those of large randomized studies in regard of therapy response (reduction of the Eckardt score) and the development of reflux. This may be regarded as a quality characteristic. Complication rates were in keeping with international averages, with due regard to a potential learning curve for a complex intervention. The advantages and disadvantages of POEM compared to other methods are addressed in the following. In a randomized controlled study published in 2019, Ponds et al. compared POEM and pneumatic balloon dilatation (PBD) in regard of treatment success (defined as an Eckardt score ≤3 and the absence of serious complications or the need for renewed treatment during the two-year follow-up period). Of 126 patients, 63 received POEM and 63 were treated with PBD. The long-term success of treatment was 92% in the POEM group, compared to 54% in the PBD group. The latter group had 2 serious complications, including an esophageal perforation. No complications were observed in the POEM group. The study confirmed the significant superiority of POEM compared to PBD in regard of safety and efficacy [5]. In 2018 Schlottmann et al. published a review in which the outcome of POEM was compared with that of laparoscopic Heller myotomy (LHM). After 12 months, the symptoms of dysphagia were improved in 93.5% of patients treated with POEM, whereas the same was noted in 91.0% of those treated with LHM. After 24 months, clinical symptoms were improved in 92.7% of the POEM group versus 90.0% of the LHM group. The results lead to the conclusion that POEM is at least as effective as LHM [10]. In a meta-analysis published in 2018, Repici et al. compared LHM and POEM in regard of postoperative reflux symptoms. Of 1542 patients treated with POEM, 19.0% had symptoms of reflux. In contrast, the reflux rate in LHM patients was markedly lower (8.8%). Likewise, the rates of postoperative reflux esophagitis were markedly higher after POEM (29.4%) than after LHM (7.6%) [9]. One potential advantage of LHM with fundoplication compared to POEM is the lower probability of postoperative reflux disease. Long-term data from randomized controlled trials will be needed to evaluate POEM further and compare LHM with POEM.
|
CHICAGO classification |
Cardia |
Body of the esophagus |
|
CHICAGO I |
No relaxation |
No motility |
|
CHICAGO II |
No relaxation |
Longitudinal tone without propulsive peristalsis |
|
CHICAGO III |
No relaxation |
Hypertensive peristalsis |
Table 1: Classification of achalasia by high-resolution manometry [9]
|
Symptoms |
At every meal |
Daily |
Weekly |
Did not occur |
|
Dysphagia |
3 |
2 |
1 |
0 |
|
Regurgitation |
3 |
2 |
1 |
0 |
|
Chest pain |
3 |
2 |
1 |
0 |
|
Weight loss |
>10 kg |
5-10 kg |
<5 kg |
did not occur |
|
3 |
2 |
1 |
Table 2: Eckardt score [10]
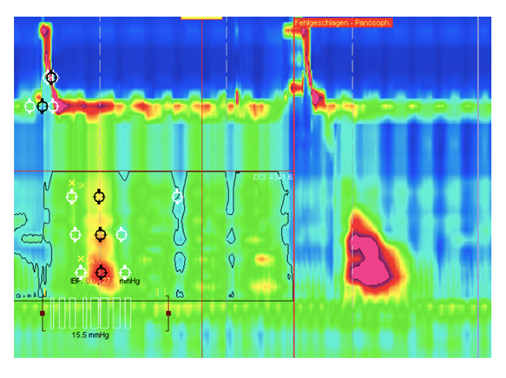
Figure 1: Achalasia Chicago II
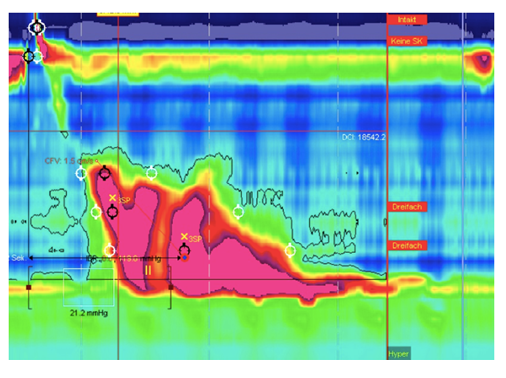
Figure 2: Achalasia Chicago III
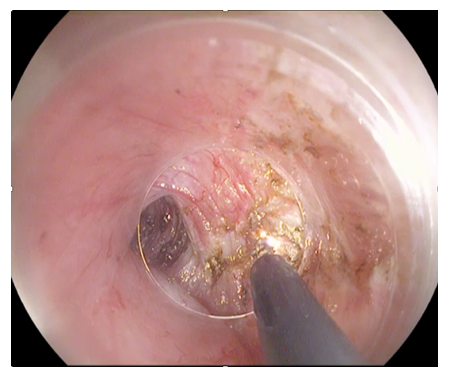
Figure 3: Myotomy during POEM
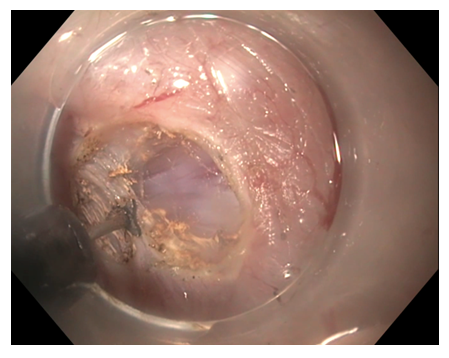
Figure 4: Myotomy during POEM: Transection of the annular muscle, preserved longitudinal muscles
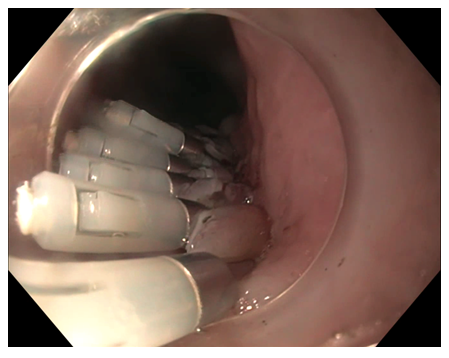
Figure 5: Closure of the myotomy tunnel with clips
5. Conclusion
In our setting, peroral endoscopic myotomy proved to be an effective and safe method for the treatment of achalasia.
References
- Pandolfino JE, Kwiatek MA, Nealis T, et al. Achalasia: a new clinically relevant classification by high-resolution manometry. Gastroenterology 135 (2008): 1526-1533.
- Eckardt VF. Clinical presentations and complications of achalasia. Gastrointest Endosc Clin N Am 11 (2001): 281-292
- Shiwaku H, Inoue H, Onimaru M, et al. Multicenter collaborative retrospective evaluation of peroral endoscopic myotomy for esophageal achalasia: analysis of data from more than 1300 patients at eight facilities in Japan. Surg Endosc 34 (2020): 464-468.
- Inoue H, Sato H, Ikeda H, et al. Per-Oral Endoscopic Myotomy: A Series of 500 Patients. J Am Coll Surg 221 (2015): 256-264.
- Ponds FA, Fockens P, Lei A, et al. Effect of Peroral Endoscopic Myotomy vs Pneumatic Dilation on Symptom Severity and Treatment Outcomes Among Treatment-Naive Patients With Achalasia: A Randomized Clinical Trial. JAMA 322 (2019): 134-144.
- Crespin OM, Liu LWC, Parmar A, et al. Safety and efficacy of POEM for treatment of achalasia: a systematic review of the literature. Surg Endosc 31 (2017): 2187-2201.
- Kurian AA, Dunst CM, Sharata A, et al. Peroral endoscopic esophageal myotomy: defining the learning curve. Gastrointest Endosc 77 (2013): 719-725.
- Patel KS, Calixte R, Modayil RJ, et al. The light at the end of the tunnel: a single-operator learning curve analysis for per oral endoscopic myotomy. Gastrointest Endosc 81 (2015): 1181-1187.
- Repici A, Fuccio L, Maselli R, et al. GERD after per-oral endoscopic myotomy as compared with Heller’s myotomy with fundoplication: a systematic review with meta-analysis. Gastrointest Endosc 87 (2018): 934-943.
- Schlottmann F, Luckett DJ, Fine J, et al. Laparoscopic Heller Myotomy Versus Peroral Endoscopic Myotomy (POEM) for Achalasia. Ann Surg 267 (2018): 451-460
