Results of Arthroscopic Repair of Bankart Lesion in Chronic Anterior Instability of the Shoulder
Article Information
Halder RC1*, Rahaman SK1, Khan MMR3, Mamun MBA1, Faruqe O1, Islam MS2, Hoque M1, Rashid MMO2, Hossain GMJ2
1Department of Orthopedics, National Institute of Traumatology and Orthopedic Rehabilitation (NITOR), Dhaka, Bangladesh
2Department of Orthopedic Surgery, National Institute of Traumatology and Orthopedic Rehabilitation (NITOR), Dhaka, Bangladesh
*Corresponding Author: Rabin Chandra Halder, Department of Orthopedics, National Institute of Traumatology and Orthopedic Rehabilitation (NITOR), Dhaka, Bangladesh.
Received: 22 February 2023; Accepted: 13 March 2023; Published: 23 March 2023
Citation:
Halder RC, Rahaman SK, Khan MMR, Mamun MBA, Faruqe O, Islam MS, Hoque M, Rashid MMO, Hossain GMJ. Results of Arthroscopic Repair of Bankart Lesion in Chronic Anterior Instability of the Shoulder. Journal of Orthopedics and Sports Medicine 5 (2023): 151-165.
View / Download Pdf Share at FacebookAbstract
Background: The shoulder is the most commonly dislocated major joint, affecting roughly 2% of the general population. Long-term studies have demonstrated a correlation between the number of instability episodes and the risk of degenerative arthritis. In an effort to treat the unstable shoulder, orthopedic surgeons have described several different operations that may help to prevent recurrent subluxation or dislocation in chronic instability cases. This study has been undertaken to assess the short-term functional outcome of Arthroscopic repair of Bankart’s Lesion in patients with Chronic Anterior Instability of the Shoulder using Constant Murley’s Score.
Material and Method: This prospective observational study was carried out at the National Institute of Traumatology and Orthopedic Rehabilitation (NITOR), from July 2017 to June 2019. Twenty cases of chronic anterior shoulder dislocation meeting the inclusion and exclusion criteria were taken in this study and underwent arthroscopic repair of bankart lesion. Here, 3 or 4 anchors were used. Cases were followed up for 6 months. The outcome was assessed with Constant Murley Scoring.
Results: The mean age was 26.716.83 years with a male predominance (95%). Most cases were students (50%) and the main cause of injury was sports (50%). The mean recurrence number was 10.65 ± 4.75 times and was significantly associated with decreasing age. The mean interval between 1 injury and surgery was 3 ± 1.89 years. Bankart lesions were found in 20% of cases in pre-operative imaging. At the final follow-up, 2 (10%) cases of limited movement were found. In 18 (90%) cases, 3 anchors were used. Finally, there was significant improvement regarding pain status, activity of daily living, forward flexion, abduction, external rotation, internal rotation and power of shoulder muscle. In the last follow-up, 2 (10%) cases of limited movement were found. The mean CMS pre-operatively and post-operatively were 63.05 ± 5.23 and 88.25 6.29 respectively (p<0.05). In the final outcome, 16 (80%) scored excellent, 3 (15%) were found good and 1 (5%) was found poor.
Conclusion: It may be concluded that arthroscopic Repair of Bankart Lesion with suture anchors in chronic anterior instability of the shoulder is a safe surgery regardless of shoulder function or range of motion.
Keywords
Arthroscopic; Repair; Chronic Anterior Instability; Bankart Lesion
Orthopedics articles Orthopedics Research articles Orthopedics review articles Orthopedics PubMed articles Orthopedics PubMed Central articles Orthopedics 2023 articles Orthopedics 2024 articles Orthopedics Scopus articles Orthopedics impact factor journals Orthopedics Scopus journals Orthopedics PubMed journals Orthopedics medical journals Orthopedics free journals Orthopedics best journals Orthopedics top journals Orthopedics free medical journals Orthopedics famous journals Orthopedics Google Scholar indexed journals Rehabilitation articles Rehabilitation Research articles Rehabilitation review articles Rehabilitation PubMed articles Rehabilitation PubMed Central articles Rehabilitation 2023 articles Rehabilitation 2024 articles Rehabilitation Scopus articles Rehabilitation impact factor journals Rehabilitation Scopus journals Rehabilitation PubMed journals Rehabilitation medical journals Rehabilitation free journals Rehabilitation best journals Rehabilitation top journals Rehabilitation free medical journals Rehabilitation famous journals Rehabilitation Google Scholar indexed journals Shoulder dysfunction articles Shoulder dysfunction Research articles Shoulder dysfunction review articles Shoulder dysfunction PubMed articles Shoulder dysfunction PubMed Central articles Shoulder dysfunction 2023 articles Shoulder dysfunction 2024 articles Shoulder dysfunction Scopus articles Shoulder dysfunction impact factor journals Shoulder dysfunction Scopus journals Shoulder dysfunction PubMed journals Shoulder dysfunction medical journals Shoulder dysfunction free journals Shoulder dysfunction best journals Shoulder dysfunction top journals Shoulder dysfunction free medical journals Shoulder dysfunction famous journals Shoulder dysfunction Google Scholar indexed journals Joint dislocation articles Joint dislocation Research articles Joint dislocation review articles Joint dislocation PubMed articles Joint dislocation PubMed Central articles Joint dislocation 2023 articles Joint dislocation 2024 articles Joint dislocation Scopus articles Joint dislocation impact factor journals Joint dislocation Scopus journals Joint dislocation PubMed journals Joint dislocation medical journals Joint dislocation free journals Joint dislocation best journals Joint dislocation top journals Joint dislocation free medical journals Joint dislocation famous journals Joint dislocation Google Scholar indexed journals Fibrocartilaginous articles Fibrocartilaginous Research articles Fibrocartilaginous review articles Fibrocartilaginous PubMed articles Fibrocartilaginous PubMed Central articles Fibrocartilaginous 2023 articles Fibrocartilaginous 2024 articles Fibrocartilaginous Scopus articles Fibrocartilaginous impact factor journals Fibrocartilaginous Scopus journals Fibrocartilaginous PubMed journals Fibrocartilaginous medical journals Fibrocartilaginous free journals Fibrocartilaginous best journals Fibrocartilaginous top journals Fibrocartilaginous free medical journals Fibrocartilaginous famous journals Fibrocartilaginous Google Scholar indexed journals Glenoid labrum articles Glenoid labrum Research articles Glenoid labrum review articles Glenoid labrum PubMed articles Glenoid labrum PubMed Central articles Glenoid labrum 2023 articles Glenoid labrum 2024 articles Glenoid labrum Scopus articles Glenoid labrum impact factor journals Glenoid labrum Scopus journals Glenoid labrum PubMed journals Glenoid labrum medical journals Glenoid labrum free journals Glenoid labrum best journals Glenoid labrum top journals Glenoid labrum free medical journals Glenoid labrum famous journals Glenoid labrum Google Scholar indexed journals Bankart's lesion articles Bankart's lesion Research articles Bankart's lesion review articles Bankart's lesion PubMed articles Bankart's lesion PubMed Central articles Bankart's lesion 2023 articles Bankart's lesion 2024 articles Bankart's lesion Scopus articles Bankart's lesion impact factor journals Bankart's lesion Scopus journals Bankart's lesion PubMed journals Bankart's lesion medical journals Bankart's lesion free journals Bankart's lesion best journals Bankart's lesion top journals Bankart's lesion free medical journals Bankart's lesion famous journals Bankart's lesion Google Scholar indexed journals Young athletic articles Young athletic Research articles Young athletic review articles Young athletic PubMed articles Young athletic PubMed Central articles Young athletic 2023 articles Young athletic 2024 articles Young athletic Scopus articles Young athletic impact factor journals Young athletic Scopus journals Young athletic PubMed journals Young athletic medical journals Young athletic free journals Young athletic best journals Young athletic top journals Young athletic free medical journals Young athletic famous journals Young athletic Google Scholar indexed journals Physical activities articles Physical activities Research articles Physical activities review articles Physical activities PubMed articles Physical activities PubMed Central articles Physical activities 2023 articles Physical activities 2024 articles Physical activities Scopus articles Physical activities impact factor journals Physical activities Scopus journals Physical activities PubMed journals Physical activities medical journals Physical activities free journals Physical activities best journals Physical activities top journals Physical activities free medical journals Physical activities famous journals Physical activities Google Scholar indexed journals Orthopedic surgeons articles Orthopedic surgeons Research articles Orthopedic surgeons review articles Orthopedic surgeons PubMed articles Orthopedic surgeons PubMed Central articles Orthopedic surgeons 2023 articles Orthopedic surgeons 2024 articles Orthopedic surgeons Scopus articles Orthopedic surgeons impact factor journals Orthopedic surgeons Scopus journals Orthopedic surgeons PubMed journals Orthopedic surgeons medical journals Orthopedic surgeons free journals Orthopedic surgeons best journals Orthopedic surgeons top journals Orthopedic surgeons free medical journals Orthopedic surgeons famous journals Orthopedic surgeons Google Scholar indexed journals Bristow Latarjet articles Bristow Latarjet Research articles Bristow Latarjet review articles Bristow Latarjet PubMed articles Bristow Latarjet PubMed Central articles Bristow Latarjet 2023 articles Bristow Latarjet 2024 articles Bristow Latarjet Scopus articles Bristow Latarjet impact factor journals Bristow Latarjet Scopus journals Bristow Latarjet PubMed journals Bristow Latarjet medical journals Bristow Latarjet free journals Bristow Latarjet best journals Bristow Latarjet top journals Bristow Latarjet free medical journals Bristow Latarjet famous journals Bristow Latarjet Google Scholar indexed journals knee articles knee Research articles knee review articles knee PubMed articles knee PubMed Central articles knee 2023 articles knee 2024 articles knee Scopus articles knee impact factor journals knee Scopus journals knee PubMed journals knee medical journals knee free journals knee best journals knee top journals knee free medical journals knee famous journals knee Google Scholar indexed journals Muscle weakness articles Muscle weakness Research articles Muscle weakness review articles Muscle weakness PubMed articles Muscle weakness PubMed Central articles Muscle weakness 2023 articles Muscle weakness 2024 articles Muscle weakness Scopus articles Muscle weakness impact factor journals Muscle weakness Scopus journals Muscle weakness PubMed journals Muscle weakness medical journals Muscle weakness free journals Muscle weakness best journals Muscle weakness top journals Muscle weakness free medical journals Muscle weakness famous journals Muscle weakness Google Scholar indexed journals Arthroscopic repair articles Arthroscopic repair Research articles Arthroscopic repair review articles Arthroscopic repair PubMed articles Arthroscopic repair PubMed Central articles Arthroscopic repair 2023 articles Arthroscopic repair 2024 articles Arthroscopic repair Scopus articles Arthroscopic repair impact factor journals Arthroscopic repair Scopus journals Arthroscopic repair PubMed journals Arthroscopic repair medical journals Arthroscopic repair free journals Arthroscopic repair best journals Arthroscopic repair top journals Arthroscopic repair free medical journals Arthroscopic repair famous journals Arthroscopic repair Google Scholar indexed journals Neuromuscular disorders articles Neuromuscular disorders Research articles Neuromuscular disorders review articles Neuromuscular disorders PubMed articles Neuromuscular disorders PubMed Central articles Neuromuscular disorders 2023 articles Neuromuscular disorders 2024 articles Neuromuscular disorders Scopus articles Neuromuscular disorders impact factor journals Neuromuscular disorders Scopus journals Neuromuscular disorders PubMed journals Neuromuscular disorders medical journals Neuromuscular disorders free journals Neuromuscular disorders best journals Neuromuscular disorders top journals Neuromuscular disorders free medical journals Neuromuscular disorders famous journals Neuromuscular disorders Google Scholar indexed journals
Article Details
1. Introduction
Shoulder instability and its treatment were described even in ancient times by Greek and Egyptian physicians. Evidence of shoulder dislocation has been found in archaeological examinations of human shoulders several thousand years old [1]. This problem can be particularly troubling to patients by causing them pain, weakness and shoulder dysfunction. The shoulder is considered the most commonly dislocated joint in the human body accounting for almost half of all joint dislocations with a reported incidence of 17 per 100000 per year [2-4]. Bankart published a paper in 1920 noting that dislocations cause the humeral head to press anteriorly out of the glenoid cavity, tearing the fibro cartilaginous labrum as well as the capsule and periosteum from the anterior aspect of the neck of the scapula [5]. This traumatic detachment of the glenoid labrum has been called the Bankart's lesion. Bankart described the detachment of the anterior inferior labrum from the glenoid rim as a cause of anterior instability [5]. The shoulder is the most commonly dislocated major joint, affecting roughly 2% of the general population. Eighty percent of shoulder dislocations are anterior, with 10% posterior and 10% multidirectional. Males are affected to a higher degree than females, at a ratio of 3:1 [6,7]. The young athletic population makes up the largest portion of patients with shoulder instability, and when treated non-operatively, has a recurrent dislocation rate approaching 71% [8-11]. Long-term studies have demonstrated a correlation between the number of instability episodes and the risk of degenerative arthritis [12-14]. Shoulders with recurrent instability that are not treated have a higher prevalence of moderate and severe arthropathy than those that are treated surgically [13]. Thus, definitive treatment of instability is crucial not only in ensuring a return to function but as a means of decreasing the incidence of degenerative arthropathies. Early surgical treatment reduces recurrence rates and improves functional outcomes in young adults engaged in physical activities [15-17]. The overall goal of treatment is to repair the capsulolabral ligamentous complex to restore glenohumeral stability and surgical intervention reduces the risk of recurrence to only 6% to 23% [18-20]. In an effort to treat the unstable shoulder, orthopedic surgeons have described several different operations that may help to prevent recurrent subluxation or dislocation. But the optimal surgical treatment of recurrent traumatic anterior shoulder instability remains a debated topic. Numerous studies have demonstrated the functional importance of the anterior-inferior capsular labral structures in maintaining glenohumeral joint stability across a wide range of motion [21-24]. These findings highlight the relevance of the Inferior Glenohumeral Ligament/Labral Complex (IGLLC) in delivering a stabilizing force, particularly when the knee is abducted and externally rotated. Several procedures have emerged as viable options for treating chronic anterior shoulder instability. In this country, the Bristow Latarjet, Bankart, Putti-Platt, and Magnuson-Stack processes are prevalent, with a regional predilection for a specific technique. The Bristow-Latarjet procedure has been modified multiple times; yet, the recurrence rate in two major series has been between 8.5 and 13 percent [25-27]. Other problems with this repair have been limitations in external rotation and muscle weakness [26]. The Putti-Platt procedure has a reported recurrence rate ranging from 0% to 12.5%, and a recent report by Hawkins revealed that glenohumeral osteoarthrosis can develop as a late complication in patients undergoing this procedure [27,28]. The functional results of the Magnuson-Stack procedure have been less satisfactory, a common complaint being the loss of external rotation, and thus, limitations in returning to overhead activities [29]. Bankart repair, also known as anatomic repair, is currently the treatment of choice according to various surveys of surgeons, with >90% of surgeons choosing the Bankart procedure as the initial repair for recurrent instability [30-32]. Repair of Bankart Lesion procedures has greatly advanced in the 90 years since Bankart first characterized this lesion. For years, open Repair of Bankart Lesionwas the gold standard, with success rates ranging from 75% to 100%; however, postoperative complications such as restriction to external rotation and secondary osteoarthritis were concerns [33-36]. The popularity of the open Repair of Bankart Lesion has evolved into the development of arthroscopic Bankart repair. It gained popularity since it began almost 30 years ago because of improved arthroscopic equipment and increased experience of surgeons [37-39]. Compared with open Bankart repair, arthroscopic Repair of Bankart Lesion gives the potential advantages of smaller skin incisions, more complete inspection of the Glenohumeral joint with access to all areas of the joint for repair, shorter surgical times, less postoperative pain, decreased blood loss, decreased narcotic usage, reduced hospitalization time, improved shoulder motion and a decreased risk of complications with maximum preservation of external rotation [40-46]. However, several early studies comparing open Repair of Bankart Lesions and arthroscopic procedures suggest a poorer prognosis in the arthroscopic groups, with recurrence rates of up to 34% [47]. These initial studies are based on older methods of fixation including staple capsulorrhaphy and transglenoid suturing. Arthroscopic techniques have advanced with techniques that more closely resemble the open procedure. The primary modification of the arthroscopic technique, accurate placement of suture anchors, has resulted in a significant decrease in recurrence after arthroscopic stabilization. Recent papers have indicated steadily decreasing rates of recurrence with the arthroscopic repair of Bankart lesions, ranging from 4% to 17% when suture anchors are used [48-53]. This study has been undertaken to assess the functional outcome of Arthroscopic repair of Bankart’s Lesion in patients with anterior recurrent shoulder dislocation using Constant Murley's Score (1987) (CMS).
2. Objectives
General Objective:
To evaluate the outcome of Arthroscopic Repair of Bankart Lesion for the treatment of chronic anterior instability of the shoulder joint
Specific Objectives:
- To evaluate the clinical improvement regarding anterior instability of the shoulder
- To see the functional outcome
- To observe the complications of the procedure
3. Methodology and Materials
This prospective observational study was carried out at the National Institute of Traumatology and Orthopedic Rehabilitation (NITOR), from July 2017 to June 2019. Twenty cases of chronic anterior shoulder dislocation meeting the inclusion and exclusion criteria were taken in this study and underwent arthroscopic repair of bankart lesion. Here, 3 or 4 anchors were used. Cases were followed up for 6 months. For statistical analysis, SPSS version 20 was used as a statistical tool. The final outcome was assessed using the Constant Murley’s Score (CMS).
Inclusion criteria
- Patients aged 17-45 years old
- Clinically diagnosed chronic anterior dislocation or subluxation of the shoulder joint.
- Instability severity index score <6
- MRI and other imaging showing Ant or Ant-inferior capsulolabral injury or Hill-sacks lesion <20%
Exclusion criteria
- Revision Bankart’s
- Habitual or voluntary anterior instability
- Recurrent dislocation with osteoarthritis and rotator cuff tear.
- Previous history of shoulder surgery
- Large glenoid fracture or Hill Sachs lesion.
- Patients with MDI (multi-directional instability).
- Patients with neuromuscular disorders.
4. Results
During this study, a total number of 20 patients with chronic anterior shoulder dislocation who fulfilled the inclusion criteria for this thesis were selected (Figure 1-6). Patients were treated operatively by arthroscopic Repair of Bankart Lesion. All patients were followed up for 6 months. In this series, the following results were obtained (Table 1-3).
|
Characteristic |
Frequency |
Percentage (%) |
|
Age in year |
||
|
16-22 |
6 |
30 |
|
23-29 |
9 |
45 |
|
30-36 |
3 |
15 |
|
37-43 |
2 |
10 |
|
Total |
20 |
100 |
|
Mean ± SD |
26.7 ± 6.83 |
100 |
Table 1: Distribution of cases according to Age in year (N=20).
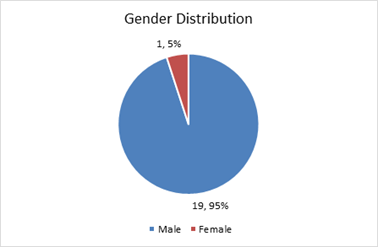
Figure 1: Distribution of the participants by Gender.
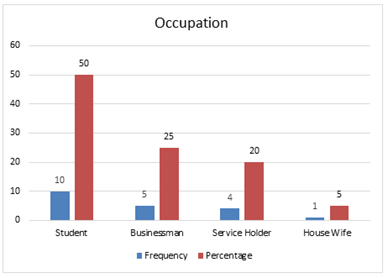
Figure 2: Distribution of the participants by occupation.
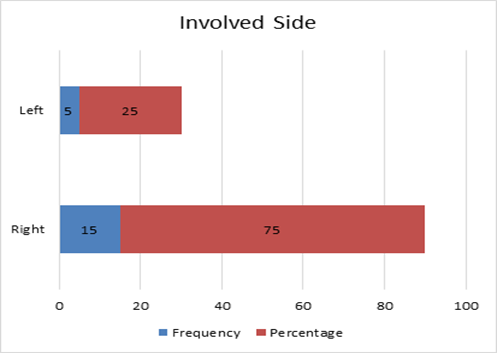
Figure 3: Distribution of Participants by involved side (N=20).
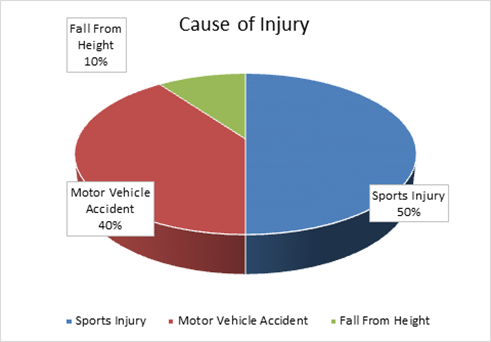
Figure 4: Distribution of participants by cause of injury (N=20).
|
Characteristic |
Frequency |
Percentage (%) |
|
Length of immobilization after 1st dislocation (in days) |
||
|
0-5 |
7 |
35 |
|
45205 |
13 |
65 |
|
Total |
20 |
100 |
|
Mean ± SD |
5.55 ± 3.12 |
|
|
Frequency of recurrence |
||
|
4-9 |
9 |
45 |
|
42278 |
7 |
35 |
|
16-21 |
4 |
20 |
|
Total |
20 |
100 |
|
Mean ± SD |
10.65 ± 4.75 |
|
|
MRI findings |
||
|
Hill Sachs |
12 |
60 |
|
Bankart |
8 |
40 |
Table 2: Distribution of cases according to Length of immobilization after 1st dislocation, Frequency of recurrence and MRI findings of study patients (N=20).
|
Characteristic |
Frequency |
Percentage (%) |
|
Complications |
||
|
No Complication |
18 |
90 |
|
Limited movement |
2 |
10 |
|
Total |
20 |
100 |
|
Number of anchors used |
||
|
3 |
18 |
90 |
|
4 |
2 |
10 |
|
Total |
20 |
100 |
Table 3: Distribution of cases according to complications and anchor used of study patients (N=20).
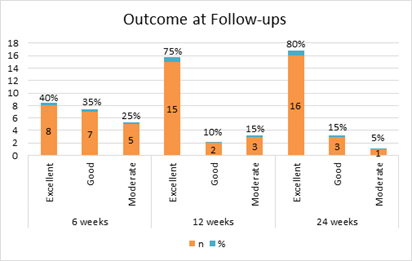
Figure 5: Outcome of patients according to CMS score at different follow-ups (N=20).
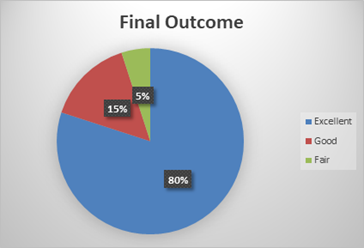
Figure 6: Final outcome at the last follow-up (N=20).
5. Discussion
Recurrent dislocation is the most common complication of traumatic anterior instability of the shoulder joint. The incidence of the recurrence rate in most reported literature was high in the young age group which was up to 71% [8-11]. In case of Multi-Directional Instability (MDI), multidirectional support is needed which cannot be repaired by arthroscopic procedure. So, this was excluded from the present study. In the present study, the mean age was 26.74 ± 6.83 years, ranging from 17 to 42 years. Maximum age incidence was found in 23-29 years of age (45%, n-9). Six cases (30%) in the 16-22 years age group. 3 (15%) in the 30-36 age group and 2 (10%) cases were found in the 37-43 age groups [54,55]. In another study by Jiang et al. [56] a total of 50 cases of chronic anterior shoulder dislocation were studied where the mean age of the cases was 27.6 years ranging from 16 to 50 years [54]. Also supported by the study of Itoi et al. [8]. where they concluded that the young athletic population makes up the largest portion of patients with shoulder instability. Out of 20 patients 19 (95%) were male and only 1 (5%) was female, with a male-female ratio of 19:1. So, male patients were predominant in this study. This was supported by another previous study where they found a male-female ratio of 3:1.6 However, Owens et al. [6] carried out their epidemiological study among the military personnel of the USA; the possibility of selection bias cannot be ruled out. In the study which was carried out among the urban population of Sweden, Kroner et al. [4] found almost similar prevalence among both genders (male 53.7%). Although incidence peaks were detected in the age groups 21-30 years for men and 61-80 years for women. As a result, among the younger population, males are the most likely to suffer from a repeated shoulder dislocation. The higher percentage of male cases in this study is much more than in any other studies, which can be explained by the fact that even in the present century, males were more involved in activities requiring overhead heavy movement of the shoulder in our country. Regarding occupation of the cases, 10 (50%) were students. 5 (25%) were businessmen, 4 (20%) were service holders and the rest 1 (5%) was a housewife. It was expected from the mechanism of injury that manual workers should be the predominant sufferer of this injury [62], though the present study could not include even a single case of the manual worker. The possible explanation is that the higher cost of the used anchors restricts the low-income group of people to choose this procedure. Among 20 patients 5 (25%) had left-sided and 15 (75%) had right-sided chronic shoulder dislocation. the left shoulder involved patients were non-dominant and right-sided patients were dominant. The higher incidence of the dominant side is not known, but suppositions are that direction of violence, and lack of coordination may play a part in the etiology. Regarding the causes of 1 injury, out of 20 patients, 10 (50%) had a sports injury, 8 (40%) had a motor vehicle accident and 2 (10%) had a history of falls from height. This data supports the proposition that young adults engaged in physical activities are the predominant sufferer [15]. In this series, out of 20 cases, during the first incidence, 7 (35%) were immobilized between 0 to 5 days. The rest 13 (65%) were immobilized for between 6 to 10 days. No association between the duration of immobilization and functional outcome is seen in this study. Again, the risk of recurrence was assessed by several authors who found no relation between the duration of the first immobilization and the rate of recurrence [55,56]. In 9 (45%) cases, dislocation recurred 4-9 times before surgery. Seven (35%) cases recurred 10-15 times and the rest 4 (20%) recurred 16-21 times previously. When the age of cases was less or equal to 22 years, the mean number of recurrences was 12.33 ± 3.39 times. But, when the age was greater than 22 years, the mean number of recurrences was 9.93 ± 15.17 times. Their series showed that the age of 20 years was the most important risk factor for recurrence [55]. Randeli et al. [59] also showed in the series that age below 22 years was significantly associated with recurrence. Among 20 cases, most of the cases (55%, n=11) were operated within 1 to 2 years of 1 event. Eight (40%) cases were operated within 3 to 5 years of the event. The remaining 1 (5%) case was operated on after 5 years of the initial event. The mean interval was 3 ± 1.89 years. In the series of Jiang et al. [56] the average time between the first dislocation and surgery was 57.9 months (range, 0.9-290 months) which was quite similar to the current study.54 No association was found between the duration and outcome. After radiological evaluation (X-ray and MRI) evaluation pre-operatively, the Hill Sachs lesion was the predominant lesion (60%, n-12) found among the cases. Bankart lesion was found in 8 (40%) cases. In the series of Voos et al. [60] they found 44% of cases of Hill Sachs lesions. In a systemic review and meta-analysis of 8 studies, found Bankart lesion in 21% of cases of recurrent anterior shoulder dislocation [33]. Though the result is similar to the present study, there are several studies, where Bankart lesions were the predominant lesion in chronic anterior shoulder dislocation. Such as, in the series of Kim et al. [61] they found Bankart lesions in 61% of their cases.58 Again, no difference was found in the outcome between the type of lesions. Regarding complications of the patients, 2 (10%) cases of limited movement were found. The rest 18 (90%) showed no complications. There were no infections, neuropathies, or implant failures. As the follow-up period was only 3 months, no cases of recurrence were found which is the most common complication after surgery [33,57,59] During surgery, in 18 (90%) cases, 3 anchors were used. In the rest 2 (10%) cases, 4 anchors were used. In the study of Voos et al. [60] 7 (10%) were treated with 1 anchor, 18 patients (25%) with 2 anchors, 39 (53%) required 3 anchors, and 9 (12%) required 4 or more anchors. In the present study, the use of 4 anchors was not needed and no cases could be stabilized with 1 anchor. Outcome of the study was reached by using the Constant Murley score [60]. To reach the score, pain status, daily life activity, shoulder movement, and functional ability were assessed both pre-operatively and finally using the Constant
Murley tool. In this study, the mean pre-operative pain score was 10.8 ± 2.09. Finally, the pain status improved to a mean score of 13.75 ± 1.74. This improvement is significant (p-value <0.05). Pain status had not decreased even in a single case suggesting that the anchor was not malpositioned as it is the most common cause of pain in arthroscopic repair of bankart lesions [61]. The mean pre-operative activity of daily living score was 15.4 ± 1.31. After 6 months of operation, the activity of daily living status improved to a mean score of 18.25 ± 0.97. This improvement was significant (p-value <0.05). In the series of Jiang et al. [56] the mean post-operative daily living score was 17.87 ± 1.54 which was similar to the present study. The mean forward flexion was 104.25:15.83 degrees. Finally, the forward flexion improved to a mean score of 136.25 ± 19.05 degrees. This improvement is significant (p-value <0.05). Their study showed mean pre-operative forward flexion was 167.6 ± 18.5 degrees which was significantly improved to 1704.7 degrees finally [54]. The mean abduction was 101.5 ± 12.99 degrees. Finally, the abduction improved to a mean score of 140.75 ± 17.64 degrees. This improvement was significant (p-value <0.05). Again, in the series of Leroux et al. [65] they showed significant improvement in shoulder abduction post-operatively [62]. The mean external rotation score was 5.6 ± 1.04. Finally, the external rotation score status improved to a mean score of 8.2 ± 0.89. The mean internal rotation score was 5.9 ± 1.02. Finally, the internal rotation score status improved to a mean score of 8.1 ± 0.79. In both variables, improvement was significant (p-value <0.05) [63,64]. The score was activity-based, not in degree. Other several studies measure external rotation in degrees such as in the series of the mean post-operative external rotation was 56.56 ± 116.6 and degrees [54]. No study is found to measure the external rotation based on activity. But internal rotation was measured in a scoring system in different literature. In the series of Leroux et al. [65] the mean postoperative internal rotation score was 9.3 ± 1.1 [62]. The mean power score was 14.45 ± 4.9. Finally, the power score status improved to a mean score of 22.75 ± 43.99. This improvement was significant (p-value <0.05). Jaju et al. [66] measured the power with UCLA score and found mean post-operative power was 118.33 ± 4.8 which was not significantly improved than its pre-operative status. As in their study, immediate post-operative power was measured instead of measuring it finally, the improvement was not significant. The mean total Constant Murley score was 63.05 ± 5.23. Finally, the power score status improved to a mean score of 88.25 ± 6.29. This improvement is significant (p-value <0.05). The weighted average of the mean Constant Murley score of 3 studies was 78.6 also after a significant improvement.64-66 In the series of Jiang et al. [56] the mean post-operative Constant Murley score was 97.7 ± 42.7.54 The discrepancy in the final score can be explained by the fact that this scoring criterion varies among observers which is a drawback of this criterion [9]. Among the 20 cases, 16 (80%) scored excellent as per Constant Murley criteria finally. Three (15%) were found good and 1 (5%) was found fair. This outcome suggests that in selected cases, arthroscopic repair of bankart lesions is an effective tool to manage chronic anterior shoulder dislocation [66].
6. Conclusion and Recommendations
It may be stated that arthroscopic Repair of Bankart Lesion with suture anchors in recurrent anterior shoulder dislocation is a safe operation in terms of shoulder function and range of motion. Based on the findings of this study, it is suggested that a long-term study with a high sample size and a longer follow-up period be conducted, as well as a multi-centric study, which is ideal.
Limitations of the study:
The study sample was small to draw a conclusion and long-term outcomes could not be assessed.
Funding
Self
Conflict of interest
None
Ethical approval
Yes
References
- Brorson S. Management of fractures of the humerus in Ancient Egypt, Greece, and Rome: an historical review. Clinical Orthopaedics and Related Research, 467 (2009): 1907-1914.
- Hovelius L. Incidence of shoulder dislocation in Sweden. Clinical orthopaedics and related research 166 (1982): 127-131.
- Dietch J, Mehlman CT, Foad SL, et al. Traumatic anterior shoulder dislocation in adolescents. The American journal of sports medicine 31 (2003): 758-763.
- Kroner K, Lind T, Jensen J. The epidemiology of shoulder dislocations. Archives of orthopedic and trauma surgery 108 (1989): 288-290.
- Bankart AB. Congenital Absence of the Ulna. Proceedings of the Royal Society of Medicine. Mar; 13 (1920): 211-212.
- Owens BD, Duffey ML, Nelson BJ, et al. The incidence and characteristics of shoulder instability at the United States Military Academy. The American journal of sports medicine 35 (2007): 1168-1173.
- Hovelius L, Olofsson A, Sandstorm B, et al. Nonoperative treatment of primary anterior shoulder dislocation in patients. Forty years of age and younger: a prospective twenty-five-year follow-up. The Journal of Bone and Joint Surgery. American 90 (2008): 945-952.
- Itoi E, Hatakeyama Y, Sato T, et al. Immobilization in external rotation after shoulder dislocation reduces the risk of recurrence: a randomized controlled trial. The Journal of Bone and Joint Surgery American Volume 89 (2007): 2124-2131.
- Leroux T, Wasserstein D, Veillette C, et al. Epidemiology of primary anterior shoulder dislocation requiring closed reduction in Ontario, Canada. The American journal of sports medicine 42 (2014): 442-450.
- Liavaag S, Brox J, Pripp AH, et al. Immobilization in external rotation after primary shoulder dislocation did not reduce the risk of recurrence: a randomized controlled trial. The Journal of Bone and Joint Surgery. American Volume 93 (2011): 897-904.
- Longo UG, van der Linde JA, Loppini M, et al. Surgical versus nonoperative treatment in patients up to 18 years old with traumatic shoulder instability: a systematic review and quantitative synthesis of the literature. Arthroscopy: The Journal of Arthroscopic & Related Surgery 32 (2016): 944-952.
- Hovelius L, Augustini BG, Fredin H, et al. Primary anterior dislocation of the shoulder in young patients: a ten-year prospective study. The Journal of Bone and Joint Surgery. American Volume 78 (1996): 1677-1684.
- Hovelius L, Sacboe M. Arthropathy after primary anterior shoulder dislocation 223 shoulders prospectively followed up for twenty-five years. The Journal of Shoulder and Elbow Surgery 18 (2009): 339-347.
- Samilson RL, Prieto V. Dislocation arthropathy of the shoulder. The Journal of Bone and Joint Surgery. American Volume 65 (1983): 456-460.
- Bedi A, Ryu RK. The treatment of primary anterior shoulder dislocations. Instructional course lectures, 58 (2009): 293-304.
- Kim SH, Ha KI, Kim SH. Repair of Bankart Lesion in traumatic anterior shoulder instability: open versus arthroscopic technique. Arthroscopy: The Journal of Arthroscopic and Related Surgery 18 (2002): 755-763.
- Kirkley A, Griffin S, Richards C, et al. Prospective randomized clinical trial comparing the effectiveness of immediate arthroscopic stabilization versus immobilization and rehabilitation in first traumatic anterior dislocations of the shoulder. Arthroscopy: The Journal of Arthroscopic and Related Surgery 15 (1999): 507-514.
- Chamlers PN, Mascarenhas R, Leroux T, et al. Do arthroscopic and open stabilization techniques restore equivalent stability to the shoulder in the setting of anterior glenohumeral instability? A systematic review of overlapping meta-analyses. Arthroscopy: The Journal of Arthroscopic and Related Surgery 31 (2015): 355-363.
- Arciero RA, Wheeler JH, Ryan JB, et al. Arthroscopic Repair of Bankart Lesionversus nonoperative treatment for acute, initial anterior shoulder dislocations. The American journal of sports medicine 22 (1994): 589-594.
- Hobby J, Griffin D, Dunbar M. et al. Is arthroscopic surgery for stabilisation of chronic shoulder instability as effective as open surgery? A systematic review and meta-analysis of 62 studies including 3044 arthroscopic operations. The Journal of bone and joint surgery. British volume 89 (2007): 1188-1196.
- Bankart ASB. The pathology and treatment of recurrent dislocation of the shoulder-joint. British Journal of Surgery 26 (1938): 23-29.
- Moseley HF, Overgaarde kB. The anterior capsule mechanism in the recurrent dislocation of the shoulder. Morphological and clinical studies with special references to the glenoid labrum and the glenohumeral ligaments. The Journal of Bone and Joint Surgery. British Volume 44 (1973): 913.
- Turkel SJ, Panio MW, Marshall JL, et al. Stabilizing mechanisms preventing anterior dislocation of the glenohumeral joint. The Journal of bone and joint surgery. American volume 63 (1981): 1208-1217.
- Galinat BJ, Howell SM. The containment mechanism: the primary stabilizer of the glenohumeral joint. Orthop Trans 11 (1987): 458.
- O'Brien SJ, Neves MC, Amoczky SP, et al. The anatomy and histology of the inferior glenohumeral ligament complex of the shoulder. The American journal of sports medicine 18 (1990): 449-456.
- Trog JS, Balduini FC, Bonci C, et al. A modified Bristow-Helfet-May procedure for recurrent dislocation and subluxation of the shoulder. Report of two hundred and twelve cases. The Journal of bone and joint surgery. American volume 69 (1987): 904-913.
- Hovelius L, Albrektsson B, Berg E, et al. Bristow-Latarjet procedure for recurrent anterior dislocation of the shoulder: a 2-5 year follow-up study on the results of 112 cases. ActaOrthopaedicaScandinavica 54 (1983): 284-290.
- Hawkins R, Angelo RL. Glenohumeralosteoarthrosis. A late complication of the Putti-Platt repair. The Journal of bone and joint surgery. American volume 72 (1990): 1193-1197.
- Wolf EM, Wilk RM, Richmond JC. Arthroscopic Repair of Bankart Lesionusing suture anchors. Operative techniques in orthopaedics 1 (1991): 184-191.
- Berendes TD, Pilot P, Nagels J, et al. Survey on the management of acute first-time anterior shoulder dislocation amongst Dutch public hospitals, Archives of orthopedic and trauma surgery 135 (2015): 447-454.
- Boileau P, Richou J, Lisai A, et al. The role of arthroscopy in revision of failed open anterior stabilization of the shoulder. Arthroscopy: The Journal of Arthroscopic & Related Surgery 25 (2009): 1075-1084.
- Chong M, Karataglis D, Learmonth D. Survey of the management of acute traumatic first-time anterior shoulder dislocation among trauma clinicians in the UK. The Annals of The Royal College of Surgeons of England 88 (2006): 454-458.
- An VVG, Sivakumar BS, Phan K, et al. A systematic review and meta- analysis of clinical and patient-reported outcomes following two procedures for recurrent traumatic anterior instability of the shoulder: Latarjet procedure vs. Bankart repair. Journal of shoulder and elbow surgery 25 (2016): 853-863.
- Hubell JD, Ahmad S, Bezenoff LS, et al. Comparison of shoulder stabilization using arthroscopic transglenoid sutures versus open capsulolabral repairs: a 5-year minimum follow-up. The American journal of sports medicine 32 (2004): 650-654.
- Freedman KB, Smith AP, Romeo AA, et al. Open Repair of Bankart Lesionversus Arthroscopic Repair with Transglenoid Sutures or Bioabsorbable Tacks for Recurrent Anterior Instability of the Shoulder: A 6-Month Study. The American journal of sports medicine 32 (2004): 1520-1527.
- Owens BD, Cameron KL, Peck KY, et al. Arthroscopic versus open stabilization for anterior shoulder subluxations. Orthopedic journal of sports medicine 3 (2015): 2325967115571084.
- Green MR, Christensen KP. Arthroscopic versus open Bankart procedures: a comparison of early morbidity and complications. Arthroscopy: The Journal of Arthroscopic & Related Surgery 9 (1993): 371-374.
- Speer KP, Deng X, Borrero S, et al. Biomechanical evaluation of a simulated Bankart lesion. The Journal of bone and Joint Surgery. American Volume 76 (1994): 1819-1826.
- Cole BJ, L'insalata J, Irrgang J, et al. Comparison of arthroscopic and open anterior shoulder stabilization: a two to six-year follow-up study. The Journal of Bone and Joint Surgery. American Volume 82 (2000): 1108.
- Arciero RA, Taylor DC, Snyder RJ, et al. Arthroscopic bioabsorbable tack stabilization of initial anterior shoulder dislocations: a preliminary report. Arthroscopy: The Journal of Arthroscopic and Related Surgery 11 (1995): 410-417.
- Bacilla P, Field LD, Savoie III FH. Arthroscopic Repair of Bankart Lesion in a high demand patient population. Arthroscopy: The Journal of Arthroscopic & Related Surgery 13 (1997): 51-60.
- Bankart B. Recurrent or habitual dislocation of the shoulder-joint. British Medical Journal 2 (1920): 1132.
- Kartus J, Ejerhed L, Funck E, et al. Arthroscopic and open shoulder stabilization using absorbable implants A clinical and radiographic comparison of two methods. Knee Surgery, Sports Traumatology, Arthroscopy 6 (1998): 181-188.
- Levy DM, Cole BJ, Bach Jr BR. History of surgical intervention of anterior shoulder instability. Journal of shoulder and elbow surgery 25 (2016): 139-150.
- McIntyre F, Caspari RB, Savoie III FH. The arthroscopic treatment of posterior shoulder instability: two-year results of a multiple suture technique. Arthroscopy: The Journal of Arthroscopic and Related Surgery, Volume 13 (1997): 426-432.
- McIntyre LF, Caspari RB, Savoie III FH. The arthroscopic treatment of multidirectional shoulder instability: two-year results of a multiple suture technique. Arthroscopy: The Journal of Arthroscopic and Related Surgery 13 (1997): 418-425.
- Savoie III FH, Miller CD, Field LD. Arthroscopic reconstruction of traumatic anterior instability of the shoulder: the Caspari technique. Arthroscopy: The Journal of Arthroscopic and Related Surgery 13 (1997): 201-209.
- Lenters TR, Franta AK, Wolf EM, et al. Arthroscopic compared with open repairs for recurrent anterior shoulder instability: a systematic review and meta- analysis of the literature. The Journal of Bone and Joint Surgery. American Volume 89 (2007): 244-254.
- Masten III FA. Overview and directions for future research. In: Masten FA, Fu FH, Hawkins RJ eds. The Shoulder: A Balance of Mobility and Stability, 1st ed. Rosemont, Illinois: American academy of Orthopedic surgeons (1993): 3-5.
- Mazzocca AD, Brown FM, Carreira DS, et al. Arthroscopic anterior shoulder stabilization of collision and contact athletes. The American Journal of sports medicine 33 (2005): 52-60.
- Kim SH, Ha K, Cho YB, et al. Arthroscopic anterior stabilization of the shoulder: two to six-year follow-up. The Journal of Bone and Joint Surhery, American Volume 85 (2003): 1511-1518.
- Fabbriciani C, Milano G, Demontis A, et al. Arthroscopic versus open treatment of Bankart lesion of the shoulder a prospective randomized study. Arthroscopy: The Journal of Arthroscopic and Related Surgery 20 (2004): 456-462.
- Cho NS, Hwang JC, Rhee YG. Arthroscopic stabilization in anterior shoulder instability: collision athletes versus noncollision athletes. Arthroscopy: The Journal of Arthroscopic and Related Surgery 22 (2006): 947-953.
- Carreira DS, Mazzocca AD, Oryhon J, et al. A prospective outcome evaluation of arthroscopic Bankart repairs: minimum 2-year follow-up. The American journal of sports medicine 34 (2006): 771-777.
- Boileau P, Bicknell RT, EiFegoun AB, et al. Arthroscopic Bristow procedure for anterior instability in shoulders with a stretched or deficient capsule: the "belt-and-suspenders" operative technique and preliminary results. Arthroscopy: The Journal of Arthroscopic & Related Surgery 23 (2007): 593-601.
- Jiang CY, Lui X, Li FL, et al. Do reduction and healing of the bony fragment really matter in arthroscopic bony Bankart reconstruction? A prospective study with clinical and computed tomography evaluations. The American journal of sports medicine 41 (2013): 2617-2623.
- Jobe FW, Bradley JP. The diagnosis and nonoperative treatment of shoulder injuries in athl Clinics in sports medicine 8 (1989): 419-438.
- Flinkkila T, Hyvonen P, Ohtonen P, et al. Arthroscopic Bankart repair: results and risk factors of recurrence of instability. Knee Surgery, Sports Traumatology, Arthroscopy 18 (2010): 1752-1758.
- Randelli P, Ragone V, Carminati S, et al. Risk factors for recurrence after Repair of Bankart Lesiona systematic review. Knee Surgery Sports Traumatology, Arthroscopy 20 (2012): 2129-2138.
- Voos JE, Livermore RW, Feeley BT, et al. Prospective evaluation of arthroscopic Bankart repairs for anterior instability. The American journal of sports medicine 38 (2010): 302-307.
- Kim DS, Yoon YS, Yi CH. Prevalence comparison of accompanying lesions between primary and recurrent anterior dislocation in the shoulder. The American journal of sports medicine 38 (2010): 2071-2076.
- Hayashida K, Yoneda M, Nakagawa S,et al. Arthroscopic Bankart suture repair for traumatic anterior shoulder instability: analysis of the causes of a recurrence. Arthroscopy: The Journal of Arthroscopic and Related Surgery 14 (1998): 295-301.
- Constant CR, Murley AH. A clinical method of functional assessment of the shoulder. Clinical orthopaedics and related research 214 (1987): 160-164.
- DeFroda S, Bokshan S, Stern E, et al. Arthroscopic Repair of Bankart Lesionfor the management of anterior shoulder instability: indications and outcomes. Current reviews in musculoskeletal medicine 10 (2017): 442-441.
- Leroux T, Bhatti A, Khoshbin A, et al. Combined arthroscopic Repair of Bankart Lesionand remplissage for recurrent shoulder instability. Arthroscopy: The Journal of Arthroscopic and Related Surgery 29 (2017): 1693-1701.
- Jaju R, Aziz AM, Sadigale V. Functional results of arthroscopic bankart's Repair (ABR) in bankart's lesion of the shoulder. International Journal of Orthopaedics 4 (2018): 1109-1115.
- Zhu YM, Zhang J, Shen JW, et al. Arthroscopic Repair of Bankart Lesioncombined with remplissage technique for the treatment of anterior shoulder instability with engaging Hill-Sachs lesion: a report of 49 cases with a minimum 2-year follow up. The American journal of sports medicine 39 (2011): 1640-1648.
- Haviv B, Mayo L, Biggs D. Outcomes of arthroscopic" remplissage": capsulotenodesis of the engaging large Hill-Sachs lesion. Journal of orthopedic surgery and research 6 (2011): 29.
- Boileau P, O'Shea K, Vargas P, et al. Anatomical and functional results after arthroscopic Hill-Sachs remplissage. The Journal of Bone and Joint Surgery. American Volume 94 (2012): 618-626.
