Recognizing and Diagnosing Abdominal Epilepsy in Adult Male Case Study
Article Information
Hesham Maged Mohammed Abdelfatah* and Mennatullah Mohamed Mustafa ElAgamy
Egyptian Ministry of Health, Cairo, Egypt
*Corresponding Author: Hesham Maged Mohammed Abdelfatah, Egyptian Ministry of Health, Cairo, Egypt.
Received: 07 February 2023; Accepted: 16 February 2023; Published: 20 February 2023
Citation:
Abdelfatah HMM, Mustafa ElAgamy MM. Recognizing and Diagnosing Abdominal Epilepsy in Adult Male Case Study. Journal of Psychiatry and Psychiatric Disorders 7 (2023): 21-24.
View / Download Pdf Share at FacebookAbstract
Abdominal Epilepsy (AE) is a very rare disorder; it is considered a category of temporal lobe epilepsies and was diagnosed by exclusion. AE is usually in the pediatric. However, there is recorded case of its occurrence in adults. AE can present with unexplained, cruel, and recurrent gastrointestinal symptoms such as paroxysmal severe pain, nausea, vomiting bloating, and diarrhea that improve with antiepileptic therapy. It is commonly linked with Electroencephalography (EEG) changes in the temporal lobes with symptoms that represent the involvement of the Central Nervous System (CNS) such as altered consciousness, confusion, and lethargy. That's Due to the mysterious nature of these symptoms; there is a greater chance of misdiagnosing of this case. We present the case of a 35-year-old man with AE who was misdiagnosed with psychogenic abdominal pain after doing multiple investigations with various medical branches in multiple hospital departments.
Keywords
Abdominal pain; Abdominal Epilepsy; Temporal lobe epilepsies; Electroencephalography; Psychogenic
Abdominal pain articles; Abdominal Epilepsy articles; Temporal lobe epilepsies articles; Electroencephalography articles; Psychogenic articles
Abdominal pain articles Abdominal pain Research articles Abdominal pain review articles Abdominal pain PubMed articles Abdominal pain PubMed Central articles Abdominal pain 2023 articles Abdominal pain 2024 articles Abdominal pain Scopus articles Abdominal pain impact factor journals Abdominal pain Scopus journals Abdominal pain PubMed journals Abdominal pain medical journals Abdominal pain free journals Abdominal pain best journals Abdominal pain top journals Abdominal pain free medical journals Abdominal pain famous journals Abdominal pain Google Scholar indexed journals Abdominal Epilepsy articles Abdominal Epilepsy Research articles Abdominal Epilepsy review articles Abdominal Epilepsy PubMed articles Abdominal Epilepsy PubMed Central articles Abdominal Epilepsy 2023 articles Abdominal Epilepsy 2024 articles Abdominal Epilepsy Scopus articles Abdominal Epilepsy impact factor journals Abdominal Epilepsy Scopus journals Abdominal Epilepsy PubMed journals Abdominal Epilepsy medical journals Abdominal Epilepsy free journals Abdominal Epilepsy best journals Abdominal Epilepsy top journals Abdominal Epilepsy free medical journals Abdominal Epilepsy famous journals Abdominal Epilepsy Google Scholar indexed journals Temporal lobe epilepsies articles Temporal lobe epilepsies Research articles Temporal lobe epilepsies review articles Temporal lobe epilepsies PubMed articles Temporal lobe epilepsies PubMed Central articles Temporal lobe epilepsies 2023 articles Temporal lobe epilepsies 2024 articles Temporal lobe epilepsies Scopus articles Temporal lobe epilepsies impact factor journals Temporal lobe epilepsies Scopus journals Temporal lobe epilepsies PubMed journals Temporal lobe epilepsies medical journals Temporal lobe epilepsies free journals Temporal lobe epilepsies best journals Temporal lobe epilepsies top journals Temporal lobe epilepsies free medical journals Temporal lobe epilepsies famous journals Temporal lobe epilepsies Google Scholar indexed journals Electroencephalography articles Electroencephalography Research articles Electroencephalography review articles Electroencephalography PubMed articles Electroencephalography PubMed Central articles Electroencephalography 2023 articles Electroencephalography 2024 articles Electroencephalography Scopus articles Electroencephalography impact factor journals Electroencephalography Scopus journals Electroencephalography PubMed journals Electroencephalography medical journals Electroencephalography free journals Electroencephalography best journals Electroencephalography top journals Electroencephalography free medical journals Electroencephalography famous journals Electroencephalography Google Scholar indexed journals Psychogenic articles Psychogenic Research articles Psychogenic review articles Psychogenic PubMed articles Psychogenic PubMed Central articles Psychogenic 2023 articles Psychogenic 2024 articles Psychogenic Scopus articles Psychogenic impact factor journals Psychogenic Scopus journals Psychogenic PubMed journals Psychogenic medical journals Psychogenic free journals Psychogenic best journals Psychogenic top journals Psychogenic free medical journals Psychogenic famous journals Psychogenic Google Scholar indexed journals Central Nervous System articles Central Nervous System Research articles Central Nervous System review articles Central Nervous System PubMed articles Central Nervous System PubMed Central articles Central Nervous System 2023 articles Central Nervous System 2024 articles Central Nervous System Scopus articles Central Nervous System impact factor journals Central Nervous System Scopus journals Central Nervous System PubMed journals Central Nervous System medical journals Central Nervous System free journals Central Nervous System best journals Central Nervous System top journals Central Nervous System free medical journals Central Nervous System famous journals Central Nervous System Google Scholar indexed journals symptomatology articles symptomatology Research articles symptomatology review articles symptomatology PubMed articles symptomatology PubMed Central articles symptomatology 2023 articles symptomatology 2024 articles symptomatology Scopus articles symptomatology impact factor journals symptomatology Scopus journals symptomatology PubMed journals symptomatology medical journals symptomatology free journals symptomatology best journals symptomatology top journals symptomatology free medical journals symptomatology famous journals symptomatology Google Scholar indexed journals pathology articles pathology Research articles pathology review articles pathology PubMed articles pathology PubMed Central articles pathology 2023 articles pathology 2024 articles pathology Scopus articles pathology impact factor journals pathology Scopus journals pathology PubMed journals pathology medical journals pathology free journals pathology best journals pathology top journals pathology free medical journals pathology famous journals pathology Google Scholar indexed journals disturbance articles disturbance Research articles disturbance review articles disturbance PubMed articles disturbance PubMed Central articles disturbance 2023 articles disturbance 2024 articles disturbance Scopus articles disturbance impact factor journals disturbance Scopus journals disturbance PubMed journals disturbance medical journals disturbance free journals disturbance best journals disturbance top journals disturbance free medical journals disturbance famous journals disturbance Google Scholar indexed journals disorder articles disorder Research articles disorder review articles disorder PubMed articles disorder PubMed Central articles disorder 2023 articles disorder 2024 articles disorder Scopus articles disorder impact factor journals disorder Scopus journals disorder PubMed journals disorder medical journals disorder free journals disorder best journals disorder top journals disorder free medical journals disorder famous journals disorder Google Scholar indexed journals
Article Details
Abbreviations:
AE: Abdominal Epilepsy; EEG: Electroencephalography; CNS: Central Nervous System
1. Introduction
Abdominal Epilepsy (AE) is a rare disorder, when seen in adults and presents with paroxysmal symptoms of abdominal pathology that result from seizure activity [1]. The range of this disorder is characterized by (a) unexplained, paroxysmal gastrointestinal symptoms; (b) symptoms indicate Central Nervous System (CNS) disturbance; (c) abnormal finding in the Electroencephalography (EEG) with results specific for a seizure disorder; and (d) improvement of symptoms with anticonvulsant medications [2]. The history of abdominal epilepsy has reported only 36 cases in the English literature in the past 34 years [3]. Due to the rarity of reported cases, there is a precipitately needed for accurate diagnosis by increasing knowledge among physicians to avoiding misinterpretation of these symptoms as "functional" or "psychogenic" [4,5].
2. Case Presentation
The patient is a 40-year-old right-handed male. He presented to the gastrointestinal Clinic with recurrent episodes of severe acute epigastric abdominal pain for 2 months. These episodes were associated with nausea and sometimes vomiting followed by lethargy or confusion which lasted for a few minutes after each episode. Each episode of abdominal pain lasted for 15 to 20 minutes and occurred five to eight times per day. They were sudden onset and resolved spontaneously. His prenatal and natal developmental and past medical histories were unremarkable.
General and local examinations of the abdomen and nervous system examined did not show any significant findings. He was prescribed proton pump inhibitors and he was reviewed after one week. There's anything significant improvement in his symptoms. His complete blood picture, stool analysis, 24 hr. Holter ECG, ultrasound abdomen as seen in Figure 1.
Multisided post contrast CT Abdomen as seen in Figure 2. And upper GIT endoscopy with barium swallow studies was done as seen in Figure 3. Multisided CT scan of urinary tract as seen in Figure 4. All the results were unremarkable.
Following this he was referred to the immunity unit and he done multiple lab. Investigations as (ESR – CRP – Anti_DNA – Anti_CCP IgG – RNP_ab) as seen in Figure 5. All the results were unremarkable.
Then he referred to the psychiatrist in view of psychogenic abdominal pain. He was taken antidepressants and antipsychotic medication without any improvement and he was referred to the neurology department for a second opinion.
MRI brain was found to be normal as seen in Figure 6. At this time, an epileptic etiology was suspected. a 30-minute awake EEG was made which revealed an abnormality in the form of repetitive sharp waves in the right temporal leads which were highly suggestive of an epileptogenic focus arising from the right temporal lobe as seen in Figure 7.
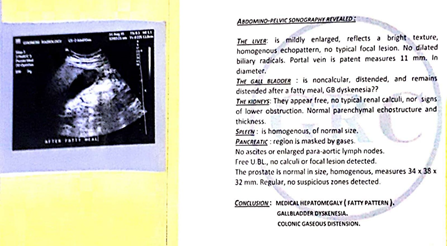
Figure 1: Abdominal-pelvic ultrasound.

Figure 2: Multisided post contrast CT abdomen.
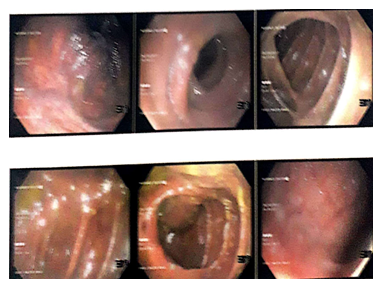
Figure 3: Upper GIT endoscopy with barium swallow.
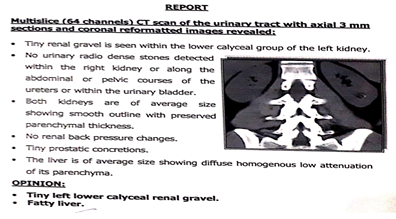
Figure 4: Multisided CT scan of urinary tract.
Figure 5: Immunity lab results.
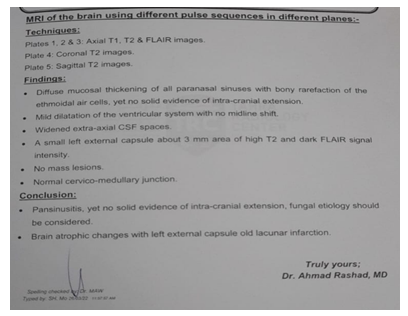
Figure 6: Brain MRI.
Then, the diagnosis of AE was made and he was started on oxcarbazepine 450mg BID. With regular follow-up visits every 2 weeks and was compliant with his medication. A follow-up over a 6 months period showed a progressive decrease in seizure frequency and has been asymptomatic.
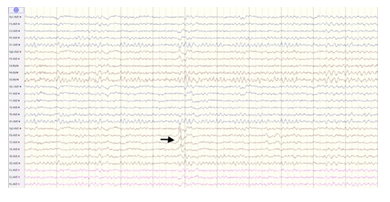
Figure 7: EEG findings of a 40-year-old male patient with abdominal epilepsy.
3. Discussion
Abdominal Epilepsy (AE) is a rare disorder and a vague nature of its symptoms; it is usually misdiagnosed or missed from diagnosis. It commonly occurs in the pediatric, but there is also documentation of its occurrence in adults [6]. It is characterized by unexplained, paroxysmal GI complaints, symptoms of a CNS disturbance, an abnormal EEG finding specific for a seizure disorder and improvement with anticonvulsant drugs [3].
AE has a variety of presenting symptoms. GI symptoms include paroxysmal pain, nausea, vomiting bloating, and diarrhea, whereas the CNS symptoms can comprise of dizziness, lethargy, headache, confusion, syncope, alternative levels of consciousness's [3,7]. As AE is also a type of autonomic epilepsy, it can be associated with some autonomic symptoms such as pallor or cold sweating, dry mouth? constipation [8]. Abdominal auras can also be found with manual and oral automatisms, that is, an auto motor seizure [9].
Although many explanations for abdominal epilepsy were outlined, the cause still remains unclear. We hypothesize that the Sylvain fissure and insular cortex lying right beneath it could be the origin of the seizure as they harmonization with the locations of the abdomen on the Sensory homunculus. Also, the M2 portion of the middle cerebral artery courses through the Sylvain fissure [10]. Any pathology of the vessel, particularly at this segment could be assumed to play a role in epilepsies of the temporoparietal lobes. Phan et al. [11] recorded a case of ictal abdominal pain with parietal lobe hemorrhage and proposed the role of the somatosensory area I in pain perception. There have been previously reported cases of ictal abdominal pain with right parietooccipital encephalomalacia, biparietal atrophy and bilateral perisylvian polymicrogyria [12,13].
Recurrent abdominal pain also seen in cases of visceral hyperalgesia, peptic ulcer disease and abdominal migraine [14,15]. The most common differential diagnosis for AE is abdominal migraine as they have many overlapping symptoms. Duration of the symptoms may be used to differentiate the two disorders; the duration is being longer in abdominal migraine than in AE. The EEG result is usually abnormal in AE and may be used to confirm the diagnosis of AE [6].
Patients with AE may have the following possible features in the EEGs:
- Patients may have normal EEG in the interictal periods and diagnosis must not be purely based on an EEG [15].
- Extra-temporal origins of epileptic foci; secondary generalization.
- There are strong suggestions that EEG doing after the first 24 hours after the epileptic episode can detect abnormalities to a greater extent [16].
4. Conclusion
This case exhibits how conclusive diagnosis of AE can be challenging with longer time-consuming as the symptomatology is unclear and as the suspicion and incidence is low especially in adults. As AE might often be omission or misdiagnosed, it should be taken into account in patients presenting with episodic, recurrent and paroxysmal GI complaints along with symptoms suggestive of CNS disturbance that's do not improve with standard treatment guide line and after thoroughly excluding the more common causes in order to accurately diagnosis. Considering EEG, preferably a video-EEG for such patients so that their symptoms are not falsely labelled as psychogenic If the EEG findings are abnormal, the treatment involves the antiepileptic drugs with regular follow-up. 450 mg oxcarbazepine BID effective in the management of AE for our case.
Human ethics:
Consent was obtained by all participants in this study.
Conflict of interest statement:
The authors have no relevant conflicts of interest to disclose.
Funding:
None
Acknowledgments:
None
References
- Franzon RC, Lopes CF, Schmutzler KM, et al. Recurrent abdominal pain: when should an epileptic seizure be suspected? Arq Neuropsiquiatr 60 (2002): 628-630.
- Dutta SR, Hazarika I, Chakravarty BP. Abdominal epilepsy, an uncommon cause of recurrent abdominal pain: a brief report. Gut 56 (2007): 439-441.
- Zinkin NT, Peppercorn MA. Abdominal epilepsy. Best Pract Res Clin Gastroenterol 19 (2005): 263-274.
- Lo Bianco G, Thomson S, Vigneri S, et al. Abdominal epilepsy, a rare cause of abdominal pain: the need to investigate thoroughly as opposed to making rapid attributions of psychogenic causality. J Pain Res 13 (2020): 457-460.
- Balabhadra A, Ali N, Balabhadra R. Abdominal epilepsy - an uncommon constellation. 144th Annual Meeting American Neurological Association 86 (2019): 0.
- Mpondo BCT, Mwasada G, Nyundo AA. Abdominal epilepsy, an uncommon cause of chronic and recurrent abdominal pain: a case report. Clin Case Rep 4 (2016): 1117-1119.
- Peppercorn MA, Herzog AG. The spectrum of abdominal epilepsy in adults. Am J Gastroenterol 84 (1989): 1294-1296.
- Singhi PD, Kaur S. Abdominal epilepsy misdiagnosed as psychogenic pain. Postgrad Med J 64 (1988): 281-282.
- Henkel A, Noachtar S, Pfänder M, et al. The localizing value of the abdominal aura and its evolution: a study in focal epilepsies. Neurology 58 (2002): 271-276.
- Navarro-Orozco D, Sánchez-Manso JC. Treasure Island FL: StatPearls Publishing, Neuroanatomy, Middle Cerebral Artery (2020).
- Phan TG, Cascino GD, Fulgham J. Ictal abdominal pain heralding parietal lobe haemorrhage. Seizure 10 (2001): 56-59.
- Siegel AM, Williamson PD, Roberts DW, et al. Localized pain associated with seizures originating in the parietal lobe.. Epilepsia 40 (1999): 845-855.
- García-Herrero D, Fernández-Torre JL, Barrasa J, et al. Abdominal epilepsy in an adolescent with Bilateral Perisylvian Polymicrogyria. Epilepsia 39 (1998): 1370-1374.
- Di Lorenzo C, Youssef NN, Sigurdsson L, et al. Visceral hyperalgesia in children with functional abdominal pain. J Pediatr 139 (2001): 838-843.
- Kshirsagar VY, Nagarsenkar S, Ahmed M, et al. Abdominal epilepsy in chronic recurrent abdominal pain. J Pediatr Neurosci 7 (2012): 163-166.
- Hirtz D, Ashwal S, Berg A, et al. Practice parameter: evaluating a first nonfebrile seizure in children: report of the quality standards subcommittee of the American Academy of Neurology, The Child Neurology Society, and The American Epilepsy Society. Neurology 55 (2000): 616-623.
