Rare Glomerular Presentation of Essential Cryoglobulinemia without HCV Infection
Article Information
Dragana Markovic1*, Petar Djuric1, Aleksandar Jankovic1, Ljiljana Bogdanovic3, Snezana Pešic1, Nada Dimkovic4, Radomir Naumovic1,2
1Clinical Department for Nephrology, Zvezdara University Medical Center, Belgrade, Serbia
2Medical Faculty, University of Belgrade, Belgrade, Serbia
3Institute of Pathology, Medical Faculty, University of Belgrade, Serbia
4Academy of Medical Sciences of the Serbian Medical Society, Serbia
*Corresponding Author: Dragana Markovic, Clinical Department for Nephrology, Zvezdara University Medical Center, Belgrade, Serbia
Received: 15 January 2021; Accepted: 02 February 2021; Published: 10 March 2021
Citation: Dragana Marković, Petar Djurić, Aleksandar Janković, Ljiljana Bogdanović, Snežana Pešić, Nada Dimkovic, Radomir Naumović. Rare Glomerular Presentation of Essential Cryoglobulinemia without HCV Infection. Archives of Clinical and Medical Case Reports 5 (2021): 280-286.
View / Download Pdf Share at FacebookAbstract
Membranoproliferative glomerulonephritis (MPGN) is characterized by mesangial cell proliferation and structural changes in glomerular capillary walls and double-contoured glomerular basement membrane (GBM). Usually, it is connected with cryoglobulinemia which is defined by the presence of a circulating, a cold-precipitating immunoglobulin. The chemical and immunological features of the cryoglobulins are used to define three types of cryoglobulinemia. In this report we describe the third case of MPGN type II with essential cryoglobulinemia without HCV infection, which is usually defined in the literature as MPGN type II. Here, we present 61-years old woman previously diagnosed with MPGN in 2012 at another institution. At that time, she was not examined in terms of cryoglobulinemia. Initially she was treated with pulses of methylprednisolone, then oral corticosteroids until cessation when complete remission was achieved. Meanwhile, she had two relapses of the disease. In October 2020 we re-evaluated her and found out positive cryoglobulins in repeating testing. Serological studies for anti-neutrophil cytoplasmic antibodies (ANCA), myeloperoxidase and proteinase 3, anti-double stranded DNA antibodies, anti-hepatitis C antibodies, anti-HIV antibodies and anti-hepatitis B surface antibodies were all negative. Serum M protein or monoclonal IgM were not detected. Percutaneous renal biopsy was compatible with the diagnosis of MPGN. Based on clinical, laboratory and histological evaluation, it was concluded that the patient had a MPGN with essential cryoglobulinemia. Therapy with mycophenolate mofetil had a beneficial effect on the course of disease and the patient achieved partial remission and stabile renal function for the last 3 months of follow-up. Since the therapy for MPGN with essential cryoglobulinemia is not standardized, further research in the field is needed.
Keywords
Cryoglobulinemia; Membranoproliferative glomerulonephritis
Cryoglobulinemia articles; Membranoproliferative glomerulonephritis articles
Cryoglobulinemia articles Cryoglobulinemia Research articles Cryoglobulinemia review articles Cryoglobulinemia PubMed articles Cryoglobulinemia PubMed Central articles Cryoglobulinemia 2023 articles Cryoglobulinemia 2024 articles Cryoglobulinemia Scopus articles Cryoglobulinemia impact factor journals Cryoglobulinemia Scopus journals Cryoglobulinemia PubMed journals Cryoglobulinemia medical journals Cryoglobulinemia free journals Cryoglobulinemia best journals Cryoglobulinemia top journals Cryoglobulinemia free medical journals Cryoglobulinemia famous journals Cryoglobulinemia Google Scholar indexed journals Membranoproliferative glomerulonephritis articles Membranoproliferative glomerulonephritis Research articles Membranoproliferative glomerulonephritis review articles Membranoproliferative glomerulonephritis PubMed articles Membranoproliferative glomerulonephritis PubMed Central articles Membranoproliferative glomerulonephritis 2023 articles Membranoproliferative glomerulonephritis 2024 articles Membranoproliferative glomerulonephritis Scopus articles Membranoproliferative glomerulonephritis impact factor journals Membranoproliferative glomerulonephritis Scopus journals Membranoproliferative glomerulonephritis PubMed journals Membranoproliferative glomerulonephritis medical journals Membranoproliferative glomerulonephritis free journals Membranoproliferative glomerulonephritis best journals Membranoproliferative glomerulonephritis top journals Membranoproliferative glomerulonephritis free medical journals Membranoproliferative glomerulonephritis famous journals Membranoproliferative glomerulonephritis Google Scholar indexed journals glomerulonephritis articles glomerulonephritis Research articles glomerulonephritis review articles glomerulonephritis PubMed articles glomerulonephritis PubMed Central articles glomerulonephritis 2023 articles glomerulonephritis 2024 articles glomerulonephritis Scopus articles glomerulonephritis impact factor journals glomerulonephritis Scopus journals glomerulonephritis PubMed journals glomerulonephritis medical journals glomerulonephritis free journals glomerulonephritis best journals glomerulonephritis top journals glomerulonephritis free medical journals glomerulonephritis famous journals glomerulonephritis Google Scholar indexed journals cryoglobulins articles cryoglobulins Research articles cryoglobulins review articles cryoglobulins PubMed articles cryoglobulins PubMed Central articles cryoglobulins 2023 articles cryoglobulins 2024 articles cryoglobulins Scopus articles cryoglobulins impact factor journals cryoglobulins Scopus journals cryoglobulins PubMed journals cryoglobulins medical journals cryoglobulins free journals cryoglobulins best journals cryoglobulins top journals cryoglobulins free medical journals cryoglobulins famous journals cryoglobulins Google Scholar indexed journals Lupus Erythematosus articles Lupus Erythematosus Research articles Lupus Erythematosus review articles Lupus Erythematosus PubMed articles Lupus Erythematosus PubMed Central articles Lupus Erythematosus 2023 articles Lupus Erythematosus 2024 articles Lupus Erythematosus Scopus articles Lupus Erythematosus impact factor journals Lupus Erythematosus Scopus journals Lupus Erythematosus PubMed journals Lupus Erythematosus medical journals Lupus Erythematosus free journals Lupus Erythematosus best journals Lupus Erythematosus top journals Lupus Erythematosus free medical journals Lupus Erythematosus famous journals Lupus Erythematosus Google Scholar indexed journals treatment articles treatment Research articles treatment review articles treatment PubMed articles treatment PubMed Central articles treatment 2023 articles treatment 2024 articles treatment Scopus articles treatment impact factor journals treatment Scopus journals treatment PubMed journals treatment medical journals treatment free journals treatment best journals treatment top journals treatment free medical journals treatment famous journals treatment Google Scholar indexed journals CT articles CT Research articles CT review articles CT PubMed articles CT PubMed Central articles CT 2023 articles CT 2024 articles CT Scopus articles CT impact factor journals CT Scopus journals CT PubMed journals CT medical journals CT free journals CT best journals CT top journals CT free medical journals CT famous journals CT Google Scholar indexed journals surgery articles surgery Research articles surgery review articles surgery PubMed articles surgery PubMed Central articles surgery 2023 articles surgery 2024 articles surgery Scopus articles surgery impact factor journals surgery Scopus journals surgery PubMed journals surgery medical journals surgery free journals surgery best journals surgery top journals surgery free medical journals surgery famous journals surgery Google Scholar indexed journals Leukemia articles Leukemia Research articles Leukemia review articles Leukemia PubMed articles Leukemia PubMed Central articles Leukemia 2023 articles Leukemia 2024 articles Leukemia Scopus articles Leukemia impact factor journals Leukemia Scopus journals Leukemia PubMed journals Leukemia medical journals Leukemia free journals Leukemia best journals Leukemia top journals Leukemia free medical journals Leukemia famous journals Leukemia Google Scholar indexed journals Syndrome articles Syndrome Research articles Syndrome review articles Syndrome PubMed articles Syndrome PubMed Central articles Syndrome 2023 articles Syndrome 2024 articles Syndrome Scopus articles Syndrome impact factor journals Syndrome Scopus journals Syndrome PubMed journals Syndrome medical journals Syndrome free journals Syndrome best journals Syndrome top journals Syndrome free medical journals Syndrome famous journals Syndrome Google Scholar indexed journals
Article Details
1. Introduction
Cryoglobulinemia is defined by the presence of a circulating, a cold-precipitating immunoglobulin [4]. The chemical and immunological features of the cryoglobulins are used to define three types of cryoglobulinemia. Type I cryoglobulinemia or simple cryoglobulinemia is characterized by a single monoclonal Ig, which is usually an IgM or IgG. In type II cryoglobulinemia, polyclonal immunoglobulins form immune complexes with one or more monoclonal immunoglobulins. The most common form combines a monoclonal IgM and polyclonal IgG (mixed monoclonal cryoglobulinemia). Finally, type III cryoglobulinemia involves only polyclonal immunoglobulins. Polyclonal IgM and IgG may form immune complexes (mixed polyclonal cryoglobulinemia) [5].
In this report, we describe the third case of MPGN type II with essential cryoglobulinemia without HCV infection which is usually defined in the literature as MPGN type II.
2. Case Presentation
A 61-year old woman was hospitalized at our department in November 2020. for reevaluation and second renal biopsy. She was previously diagnosed with MPGN in 2012 at another institution when clinical manifestation of disease included nephrotic proteinuria and hematuria without renal failure (proteinuria 5g/24h, urine: 15-20 red blood cells/high-power field). At that time, the patient was not examined in terms of cryoglobulinemia. Initially she was treated with pulses of methylprednisolone, then oral corticosteroids in a dose of 40mg until cessation when complete remission was achieved. In October 2017, immunosuppressive therapy (cyclophosphamide and prednisone) was reintroduced due to disease relapse (proteinuria 6g/24h, creatinine 162umol/L), until complete remission was achieved in October 2018. Thereafter, she continued with small doses of corticosteroids until September 2019, when she stopped therapy. She suffered from hypertension and hypothyroidism-both well regulated with medications.
| Variables | Results |
| Leukocytes, 10^9/L | 7.2 |
| Erythrocytes, 10^12/L | 3.63 |
| Hemoglobin, g/dl | 11.0 |
| Hematocrit, % | 34.1 |
| Thrombocytes, 10^9/L | 102 |
| S-Creatinine, umol/L | 136 |
| S-Urea, mmol/L | 10.9 |
| S-Cholesterol, mmol/L | 6.6 |
| S-Triglycerides, mmol/L | 1.7 |
| S-Total proteins, g/L | 66 |
| S-Albumins, g/L | 38 |
| CRP, mg/L | 24.3 |
| IgA, g/L | 2.65 |
| IgM, g/L | 0.89 |
| IgG, g/L | 8.4 |
| C3, g/L | 1.01 |
| C4, g/L | 0.21 |
| Urine analysis | Results |
| Color | Yellow |
| Specific gravity | 1.015 |
| pH | 5.0 |
| Protein | 3+ |
| Glucose | negative |
| Ketone | negative |
| Blood | +- |
| Bilirubin | negative |
| Urobilinogen | normal |
| Nitrite | negative |
| Leukocyte esterase | negative |
| Urine sediment | WBC 3-5, RBC 3-5 |
| 24h urinary protein excretion | 5.71; 2.46; 1.86; 1.88g/24h |
WBC-white blood cells; RBC-red blood cells
Table 1: Blood laboratory tests and urine analysis at admission.
Percutaneous renal biopsy was performed, and pathohistological analysis revealed: out of 6 glomeruli, one was completely sclerotic, but in others the lobulation was emphasized with a pronounced thickening of GBM which in some segments has a duplicated appearance. Mesangial segmental proliferation was present as well as rare mononuclear cells with altered surrounding interstitium. Groups of atrophic tubules with edematously altered interstitium and permeated mononuclear infiltrate in one part formed a larger aggregate. Blood vessels experienced wall thickening. Immunofluorescence microscopy: IgA-, IgG+, IgM-/+, C1q+, C3+-C3++ staining in all specimens. The finding was compatible with the diagnosis of MPGN (see Figure 1).
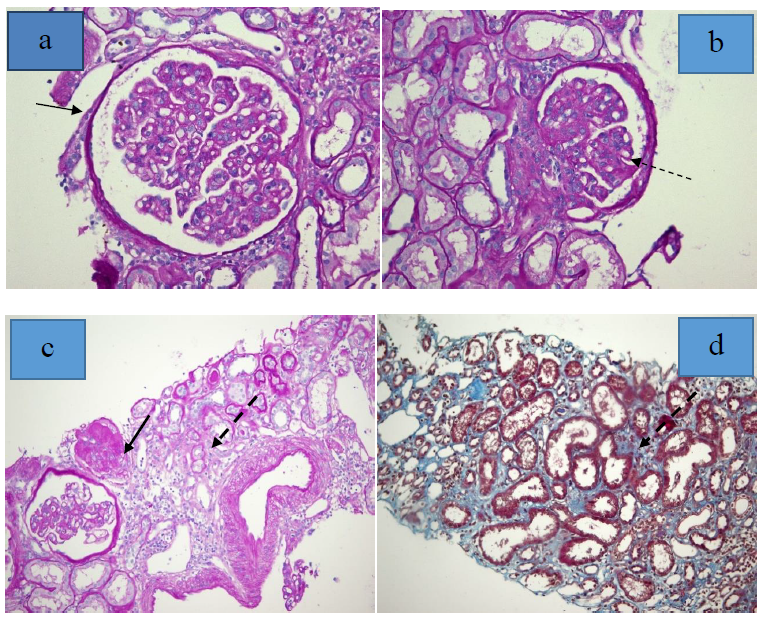
Figure 1: Mesangial hypercellularity (which gives a lobulated appearance) and capillary wall thickening, diffuse duplication of the GBM in several segments of glomeruli (a, b - PAS stain, x 400). One glomerulus was globally sclerotic (c - PAS stain, x 200), interstitial fibrosis (best shown in Masson's trichrome stain (d)) and tubular atrophy and inflammation (c). (Thin dashed arrow-duplicated GBM, thick solid arrow-sclerotic glomerulus, thin solid arrow-lobular glomerulus, dashed arrow-mesangial modification).
Based on clinical, laboratory and histological evaluation, it was concluded that the patient had a MPGN with essential cryoglobulinemia. Since she had previously been treated with cyclophosphamide and prednisone, we commenced treatment with mycophenolate mofetil (2g/24h) divided into two doses. This therapy had a beneficial effect on the course of disease and the patient achieved partial remission and stabile renal function for the last 3 months of follow-up.
3. Discussion
There are not many cases of essential mixed II cryoglobulinemia and MPGN described in the literature, especially in the absence of hepatitis C virus infection. Namely, in available literature we found only two cases: Taiwanese authors presented female patient of the same age and with very similar clinical presentation as our patient, but they confirmed cryoglobulinemia-monoclonal gammapathy afterward. Male patient presented by Indian authors was younger (34 years) and his laboratory findings have shown significantly higher levels of urea and creatinine, while urine analysis was very similar to that of our patient.
Initially, our patient was treated in another institution when she was diagnosed as MPGN but cryoglobulinemia was not considered at that time. Crioglobulinemia was diagnosed after eight years, in October 2020, at our institution. In November 2020 the presence of cryoglobulins was confirmed for the second time and a re-biopsy was performed. Serum cryoglobulin testing involves a manual qualitative method. The test is based on the properties of cryoglobulins to group and precipitate in the cold, but dissolve at the high temperature. Negative results should be checked in 7 days. If cryoglobulins are present, additional testing is required that involves characterization and typing of the cryoglobulins. According to this, we repeated the test twice (both time positive), but more precise analysis of cryoglobulins was not available at that time. Still, considering the clinical presentation of disease, associated glomerulonephritis, typical histological finding, and absence any relevant ethiological factor linked to cryoglobulinaemia, we characterized her to have most likely essential cryoglobulinemia. In the further follow up of our patient, we should think about finding specific cause of cryoglobulinemia.
Apart from renal involvement, no other manifestation of EC was present. MPGN is the most frequent histologic finding in patients with essential cryoglobulinemia with subendothelial deposits. On immunofluorescence, deposits of immunoglobulin and complement are always present [8]. Immunofluorescence shows subendothelial and mesangial deposits of IgM, IgG, C3 and frequently C1q [8] like in our patient. Renal disease at presentation of cryoglobulinemia is apparent in less than 25% of patients, but develops in about 50% over time [8]. More than a half has proteinuria and/or hematuria. Nephrotic syndrome is diagnosed in 20% of patients and acute nephritic syndrome in 20% [7]. In our patient the disease was manifested by mild renal insufficiency with subnephrotic proteinuria. No standard treatment for essential cryoglobulinemia associated with MPGN treatment was suggested and decisions should be made purely on the basis of clinical experience. Acute nephritic and/or severe vasculitis flare-ups may be treated with high-dose of intravenous steroid pulses followed by a short-term course of oral prednisolone and cytotoxic drugs [8]. Patients who develop progressive renal disease are candidates for dialysis or transplantation. This patient had three partial remissions and last one was achieved by the protocol with mycophenolate mofetil. Still, we need longer follow-up period to establish the effect of such therapy and the course of disease. Since the therapy for MPGN with essential cryoglobulinemia is not standardized, further research in the field is needed.
References
- Bassam Alchi and David Jayne. Membranoproliferative glomerulonephritis. Pediatr Nephrol 25 (2010): 1409-1418.
- Naveed Masani, Kenar D Jhaveri, and Steven Fishbane. Update on Membranoproliferative GN. Clin J Am Soc Nephrol 9 (2014): 600-608.
- Maurizio Salvadori and Giuseppina Rosso. Reclassification of membranoproliferative glomerulonephritis: Identification of a new GN: C3GN. World J Nephrol 5 (2016): 308-320.
- Naveed Masani, Kenar DJhaveri, and Steven Fishbane. Update on Membranoproliferative GN. Clin J Am Soc Nephrol 9 (2014): 600-608.
- StéphanieHarel, Alexis Talbot. Cryoglobulinemia for use. Rev Prat 68 (2018): 1107-1112.
- Anne Claire Desbois, Patrice Cacoub, David Saadoun. Cryoglobulinemia: An update in 2019. Revue du Rhumatisme 86 (2019): 241-248.
- Hsu Jung-Hui, Fang Yu-Wei, Yang An-Hung, et al. Mixed cryoglobulinemic membranoproliferative glomerulonephritis due to monoclonal gammopathy of undetermined significance. Medicine 97 (2018): e12416.
- Satish S, Rajesh R, George K, et al. Membranoproliferative glomerulonephritis with essential cryoglobulinemia. Indian J Nephrol 18 (2008): 80-82.
