Rare Case of Takayasu Arteritis with Simultaneous Stenosis and Dilatation with Infrarenal Aortic Aneurysm
Article Information
Anoop Nagpal, Uma Debi*, Lokesh Singh, M S Sandhu
Department of Radio diagnosis and Imaging, PGIMER, Chandigarh, India
*Corresponding author: Uma Debi, Department of Radio diagnosis and Imaging, PGIMER, Chandigarh, India
Received: 18 December 2020; Accepted: 04 January 2021; Published: 11 January 2021
Citation: Anoop Nagpal, Uma Debi, Lokesh Singh, M S Sandhu. Rare Case of Takayasu Arteritis with Simultaneous Stenosis and Dilatation with Infrarenal Aortic Aneurysm. Cardiology and Cardiovascular Medicine 5 (2021): 55-56.
View / Download Pdf Share at FacebookAbstract
Takayasu arteritis is a granulomatous vasculities involving aorta and its branches, leading to stenosis, thrombosis or sometimes aneurysm formation. Our patient is a 36 year old female presented clinically with symptoms consistent with arteritis and on imaging, shows presence of concurrent stenosis and aneurysmal dilation of right sided subclavian artery with dilatation of brachiocephalic trunk and celiac artery. It also demonstrated Saccular aneurysm with ulcerative plaques arising from the infrarenal aorta.
Keywords
Takayasu Arteritis
Article Details
1. Case History
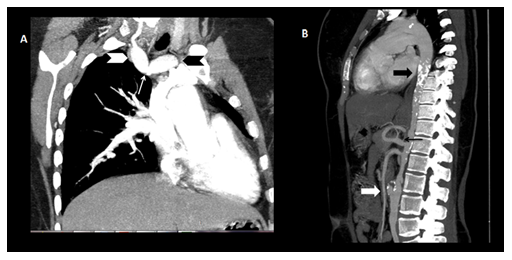
A 36 year old female patient with a history of intermittent claudication of extremities presented with right side throbbing headache associated with mild blurring of vision and dizziness. Physical examination revealed vascular bruit in right side of neck. Vital signs showed presence of high blood pressure (> 160/90) in both the upper limbs. CT angiography revealed focal stenosis of right subclavian artery origin (Figure 1A,thin white arrow), fusiform dilatation of brachicephalic trunk (black arrowhead), right subclavian artery distal to stenosis (white arrowhead) and celiac artery (Figure 1B,thin black arrow), and diffuse mural thickening of abdominal aorta with concentric calcified plaques (black arrow) causing moderate luminal narrowing and irregularity at places. It also demonstrated a saccular aneurysm (white arrow) measuring 2.1 x 1.9 cm in size with ulcerative plaques arising from the anterior aspect of infra-renal aorta at L2-L3 vertebral level.
Figure 1: CT angiography Reformatted coronal image (A) revealed focal stenosis of right subclavian artery origin (white arrow) and fusiform dilataion of brachicephalic trunk (black arrowhead) and right subclavian artery (white arrowhead). Sagittal reconstructed image (B) showing calcified plaques in aorta (black arrow), fusiform dilatation of celiac artery (thin black arrow) and saccular aneurysm in infrarenal arota (white arrow).
2. Discussion
Takayasu arteritis is a chronic granulomatous large vessel vasculitis of that affects the aorta, its branches and the pulmonary arteries leading to stenosis, occlusions and sometimes aneurysm formation. The disease is more commonly seen in women with age group of 10-40 years. Although, arterial stenosis is more commonly seen with this condition, but aneurysms formation are not that uncommon [1]. Concurrent involvement of stenosis and aneurysms are rarely seen. The inflammatory process in Takayasu arteritis can lead to proliferation of the intima causing stenosis of the involved vessel and damage of elastic lamina and muscularis media of the vessel wall leading to its aneurysmal dilatation [2]. Aortic aneurysms can be a fatal complication as it can lead to increase in risk of development of cardiac failure, aortic insufficiency, aortic dissection and rupture [3].
No disclaimers
Sources of support
none
References
- Sueyoshi E, Sakamoto I, Hayashi K. Aortic aneurysms in patients with Takayasu’s arteritis: CT evaluation. Am J Roentgenol 175 (2000): 1727-1733.
- Tso E, Flamm SD, White RD, Schvartzman PR, Mascha E, Hoffman GS. Takayasu arteritis: utility and limitations of magnetic resonance imaging in diagnosis and treatment. Arthritis Rheum 46 (2002): 1634-1642.
- Kun-Qi Yang, Yan-Kun Yang, Xu Meng, Ying Zhang, Hui-Min Zhang, Hai-Ying Wu, et al. Aortic Dissection in Takayasu Arteritis. Am J Med Sci 353 (2017): 342-352.