RAI Refractory Differentiated Thyroid Cancer Treated with Lenvatinib: Case Report
Article Information
Ivana Puliafito1#, Caterina Puglisi2*#, Stefania Marchisotta3, Pasquale Malandrino4, Paolo Giuffrida1, Francesca Esposito2, Angela Prestifilippo1, Dario Giuffrida1
#Authors were contributed equally to this work
1Medical Oncology Unit, Mediterranean Institute of Oncology, Viagrande (CT), Italy
2IOM Ricerca, Viagrande (CT), Italy
3Department of Endocrinology, Palermo, Italy
4Department of Endocrinology, Garibaldi Hospital, Catania, Italy
*Corresponding Author: Dr. Caterina Puglisi, IOM Ricerca via penninazzo 11, Viagrande, Catania, Italy
Received: 03 June 2020; Accepted: 30 June 2020; Published: 03 August 2020
Citation: Ivana Puliafito, Caterina Puglisi, Stefania Marchisotta, Pasquale Malandrino, Paolo Giuffrida, Francesca Esposito, Angela Prestifilippo, Dario Giuffrida. RAI Refractory Differentiated Thyroid Cancer Treated with Lenvatinib: Case Report. Journal of Cancer Science and Clinical Therapeutics 4 (2020): 229-236.
View / Download Pdf Share at FacebookAbstract
Background: Differentiated thyroid carcinoma (DTC) is the most common malignant tumor of the thyroid gland and causes local and/or distant metastases. Differentiated thyroid carcinoma (DTC) is the most common form, representing more than 90% of all thyroid cancers and derives from the follicular cells of the thyroid. Choroidal metastasis from DTC is extremely rare. Only a few cases have been reported in literature.
Case Summary: We report the case of a 43-year-old man with differentiated thyroid cancer. He underwent a total thyroidectomy plus a right latero-cervical lymphoadenectomy. Histological examination revealed a 7 mm papillary thyroid cancer, pT3N1b. Firstly treated with locoregional treatment. In February 2012 computer tomography (CT) scan and WBS showed a progression of disease with bilateral lung lesions, bilateral multiple jugular carotid lymphnodes and bone metastases localized in the IV thoracic rib. After progression disease he was treated with Lenvatinib 24 mg daily. Symptomatic choroid metastases were diagnosed 4 years after initial diagnosis, and were treated with external-beam radiation. Although treatment reduced local masses, a rapid progression of multiple metastatic lesions was observed. Conclusion: In our case, progression free survival with lenvatinib was in agreement with data of SELECT trial, this is a rare case of choroidal metastases from DTC.
Keywords
Differentiated thyroid cancer; Lenvatinib; Choroidal metastasis; Tyrosine kinase inhibitors; Bone metastases
Differentiated thyroid cancer articles, Lenvatinib articles, Choroidal metastasis articles, Tyrosine kinase inhibitors articles, Bone metastases articles
Differentiated thyroid cancer articles Differentiated thyroid cancer Research articles Differentiated thyroid cancer review articles Differentiated thyroid cancer PubMed articles Differentiated thyroid cancer PubMed Central articles Differentiated thyroid cancer 2023 articles Differentiated thyroid cancer 2024 articles Differentiated thyroid cancer Scopus articles Differentiated thyroid cancer impact factor journals Differentiated thyroid cancer Scopus journals Differentiated thyroid cancer PubMed journals Differentiated thyroid cancer medical journals Differentiated thyroid cancer free journals Differentiated thyroid cancer best journals Differentiated thyroid cancer top journals Differentiated thyroid cancer free medical journals Differentiated thyroid cancer famous journals Differentiated thyroid cancer Google Scholar indexed journals Lenvatinib articles Lenvatinib Research articles Lenvatinib review articles Lenvatinib PubMed articles Lenvatinib PubMed Central articles Lenvatinib 2023 articles Lenvatinib 2024 articles Lenvatinib Scopus articles Lenvatinib impact factor journals Lenvatinib Scopus journals Lenvatinib PubMed journals Lenvatinib medical journals Lenvatinib free journals Lenvatinib best journals Lenvatinib top journals Lenvatinib free medical journals Lenvatinib famous journals Lenvatinib Google Scholar indexed journals Choroidal metastasis articles Choroidal metastasis Research articles Choroidal metastasis review articles Choroidal metastasis PubMed articles Choroidal metastasis PubMed Central articles Choroidal metastasis 2023 articles Choroidal metastasis 2024 articles Choroidal metastasis Scopus articles Choroidal metastasis impact factor journals Choroidal metastasis Scopus journals Choroidal metastasis PubMed journals Choroidal metastasis medical journals Choroidal metastasis free journals Choroidal metastasis best journals Choroidal metastasis top journals Choroidal metastasis free medical journals Choroidal metastasis famous journals Choroidal metastasis Google Scholar indexed journals Tyrosine kinase inhibitors articles Tyrosine kinase inhibitors Research articles Tyrosine kinase inhibitors review articles Tyrosine kinase inhibitors PubMed articles Tyrosine kinase inhibitors PubMed Central articles Tyrosine kinase inhibitors 2023 articles Tyrosine kinase inhibitors 2024 articles Tyrosine kinase inhibitors Scopus articles Tyrosine kinase inhibitors impact factor journals Tyrosine kinase inhibitors Scopus journals Tyrosine kinase inhibitors PubMed journals Tyrosine kinase inhibitors medical journals Tyrosine kinase inhibitors free journals Tyrosine kinase inhibitors best journals Tyrosine kinase inhibitors top journals Tyrosine kinase inhibitors free medical journals Tyrosine kinase inhibitors famous journals Tyrosine kinase inhibitors Google Scholar indexed journals Bone metastases articles Bone metastases Research articles Bone metastases review articles Bone metastases PubMed articles Bone metastases PubMed Central articles Bone metastases 2023 articles Bone metastases 2024 articles Bone metastases Scopus articles Bone metastases impact factor journals Bone metastases Scopus journals Bone metastases PubMed journals Bone metastases medical journals Bone metastases free journals Bone metastases best journals Bone metastases top journals Bone metastases free medical journals Bone metastases famous journals Bone metastases Google Scholar indexed journals endocrine malignancy articles endocrine malignancy Research articles endocrine malignancy review articles endocrine malignancy PubMed articles endocrine malignancy PubMed Central articles endocrine malignancy 2023 articles endocrine malignancy 2024 articles endocrine malignancy Scopus articles endocrine malignancy impact factor journals endocrine malignancy Scopus journals endocrine malignancy PubMed journals endocrine malignancy medical journals endocrine malignancy free journals endocrine malignancy best journals endocrine malignancy top journals endocrine malignancy free medical journals endocrine malignancy famous journals endocrine malignancy Google Scholar indexed journals follicular carcinomas articles follicular carcinomas Research articles follicular carcinomas review articles follicular carcinomas PubMed articles follicular carcinomas PubMed Central articles follicular carcinomas 2023 articles follicular carcinomas 2024 articles follicular carcinomas Scopus articles follicular carcinomas impact factor journals follicular carcinomas Scopus journals follicular carcinomas PubMed journals follicular carcinomas medical journals follicular carcinomas free journals follicular carcinomas best journals follicular carcinomas top journals follicular carcinomas free medical journals follicular carcinomas famous journals follicular carcinomas Google Scholar indexed journals papillary articles papillary Research articles papillary review articles papillary PubMed articles papillary PubMed Central articles papillary 2023 articles papillary 2024 articles papillary Scopus articles papillary impact factor journals papillary Scopus journals papillary PubMed journals papillary medical journals papillary free journals papillary best journals papillary top journals papillary free medical journals papillary famous journals papillary Google Scholar indexed journals Medullary thyroid carcinoma articles Medullary thyroid carcinoma Research articles Medullary thyroid carcinoma review articles Medullary thyroid carcinoma PubMed articles Medullary thyroid carcinoma PubMed Central articles Medullary thyroid carcinoma 2023 articles Medullary thyroid carcinoma 2024 articles Medullary thyroid carcinoma Scopus articles Medullary thyroid carcinoma impact factor journals Medullary thyroid carcinoma Scopus journals Medullary thyroid carcinoma PubMed journals Medullary thyroid carcinoma medical journals Medullary thyroid carcinoma free journals Medullary thyroid carcinoma best journals Medullary thyroid carcinoma top journals Medullary thyroid carcinoma free medical journals Medullary thyroid carcinoma famous journals Medullary thyroid carcinoma Google Scholar indexed journals intrathyroidal tumors articles intrathyroidal tumors Research articles intrathyroidal tumors review articles intrathyroidal tumors PubMed articles intrathyroidal tumors PubMed Central articles intrathyroidal tumors 2023 articles intrathyroidal tumors 2024 articles intrathyroidal tumors Scopus articles intrathyroidal tumors impact factor journals intrathyroidal tumors Scopus journals intrathyroidal tumors PubMed journals intrathyroidal tumors medical journals intrathyroidal tumors free journals intrathyroidal tumors best journals intrathyroidal tumors top journals intrathyroidal tumors free medical journals intrathyroidal tumors famous journals intrathyroidal tumors Google Scholar indexed journals
Article Details
1. Introduction
Thyroid cancer(TC) is the most common endocrine malignancy with steadily increasing incidence over the past several decades. This increase is likely due to a better detection since the majority of new cases are small intrathyroidal tumors, discovered incidentally by sensitive neck ultrasound [1, 2]. Differentiated thyroid carcinoma (DTC) is the most common form, representing more than 90% of all thyroid cancers and derives from the follicular cells of the thyroid; it includes papillary (PTC) and follicular carcinomas (FTC). Medullary thyroid carcinoma (MTC) accounts for about 2-3% of thyroid cancers and derives from the neuroendocrine “C” cells of the thyroid gland. Anaplastic (undifferentiated) thyroid carcinoma (ATC) represents the remaining 2%.
A good overall prognosis generally applies to young patients with DTC, with no extension beyond the thyroid capsule or absent local/distant metastases. These patients experience a high 10-year survival (about 85%) with standard primary treatment, including surgery and radioiodine therapy. Nevertheless, DTC can metastasize and patients with locally advanced or metastatic disease can become refractory to treatment with radioiodine. This subgroup of patients has a poor overall prognosis and an overall survival rate of less than 15% at 10 years [3]. Metastatic MTC and ATC have most poor prognosis. Conventional therapy, including radiotherapy and chemotherapy, is unsatisfactory for patients with metastatic MTC, ATC or DTC, progressing despite radioiodine and TSH suppressive thyroid hormone therapy. Thus new therapeutic approaches are needed [4, 5].
Recently the knowledge of molecular basis of thyroid cancer and genetic critical pathways involved in the development of specific histological subtypes has led to the development of new drugs whichtargetthese pathways. Targeted therapy refers to a new generation of cancer drugs able to interfere with a specific molecular target, typically proteins that have a critical role in tumor growth or progression. Therefore, the objective of this therapy is to disrupt pathways that are inappropriately activated in cancer cells [6]. Many tyrosine kinase inhibitors (TKIs) have been studied in patients with thyroid carcinoma (TC).
The recent American Thyroid Association (ATA) Guidelines for differentiated thyroid cancer suggest that the tyrosine kinase inhibitors are indicated in R A I- refractory DTC patients with metastatic, rapidly progressive, symptomatic and/or imminently threatening disease not sensible to local control using other approaches. Sorafenib and Lenvatinib were approved by the FDA for treatment of differentiated thyroid carcinoma in locally recurrent or metastatic, progressive DTC [7, 8]. Here we report a case of a patient with radioiodine refractory DTC treated with lenvatinib 24 mg daily obtaining a good PFS and presenting with symptomatic bilateral choroidal metastases four years after his initial diagnosis.
2. Case Presentation
A 43-year-old man with a longstanding multinodular goiter, presented with a painless right latero-cervical mass in March 2009. Ultrasound examination revealed a 9 mm nodule, in the right lobe of thyroid, with suspicious right latero-cervical neck lymphoadenopaty. He underwent a total thyroidectomy plus a right latero-cervical lymphoadenectomy. Histological examination revealed a 7 mm papillary thyroid cancer, follicular variant. According to TNM classification, the tumor was staged as pT3N1b (7/27 positive lymph nodes). The post-operative staging was positive for lung metastases and the patient received, between July 2009 and July 2011, three radioiodine treatments (total dose 300 mCi131I ). At the time of the first treatment cervical radioiodine uptake was 0.64% at 24 hour; serum Tg level 8,25 ng/ml and TSH 43 uU/ml. In June 2010, the patient received 100 mCi 131I; Tg was 16 ng/ml, TSH 34 uU/ml. Total body scan (TBS) showed only a right cervical radioiodine uptake and Tg was positive. In July 2011, the patient received the third radioiodine treatment, a TBS documented the same areas of increased activity already observed at previous scan. In addition level of Tg was 1014 ng /ml and TSH was 52 uU/ml. In February 2012 computer tomography (CT) scan and WBS showed a progression of disease with bilateral lung lesions, bilateral multiple jugular carotid lymphnodes and bone metastases localized in the IV thoracic rib (Figure 1-2).
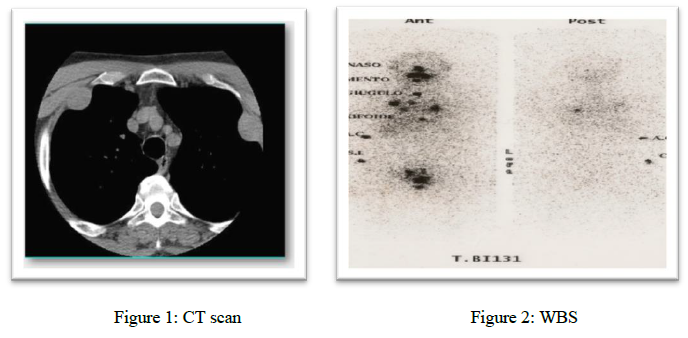
Figure 1-2: CT scan and WBS at first progression of disease showing bilateral lung lesions, bilateral jugular carotid lymphnodes and bone metastases.
In May 2012 the patient was enrolled in a clinical trial with lenvatinib (SELECT ), 24 mg total daily dose. From May 2012 to March 2013, a decrease of pulmonary nodules was observed by CT scan (Figure 3a-b). A decrease of Tg was evident from May 2012 to September 2012, followed by stabilization (Figure 4). In March 2013 a bone disease progression was observed and thyroglobulin increased from 188 ng/ml to 4873 ng/ml (Figure 4). Progression free survival of the patient was about 11 months in agreement with the results reported by the pivotal trial (SELECT). Therapy was well tolerated, reporting only hypertension grade 1, registered after 2 months of therapy and controlled with adequate medical therapy. Sporadic diarrhea was referred during treatment and was resolved by loperamide.
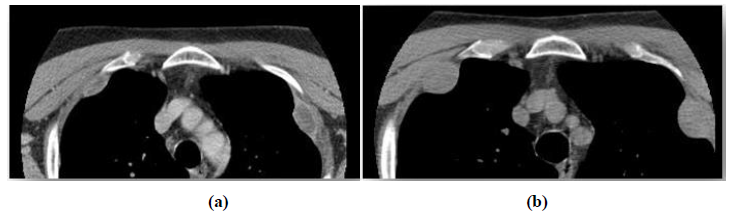
Figure 3a-b: CT scan May 2012 (a) and March 2013(b).
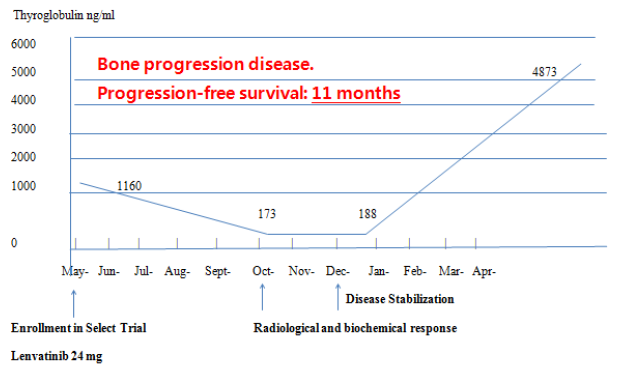
Figure 4: Thyroglobulin levels during treatment.
In May 2013, the patient started treatment with zoledronic acid, 4 mg infusional dose. After one month, patient complained diplopia, decreased visual acuity with concomitant dizziness. A cranial CT scan revealed the presence of multiple brain metastases and intraorbital bilateral lesions (Figure 5a), confirming the clinical suspicion of disease progression. A fundoscopic examination showed bilateral choroidal lesions, measuring ~11mm in diameter. This diagnosis was confirmed by orbital magnetic resonance imaging (MRI).
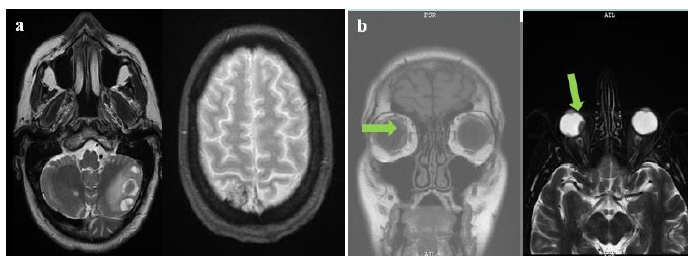
Figure 5a-b: Cranial CT scan (a) and MRI scanning (b) showing brain and choroidal metastases.
In July 2013, the administration of Lenvatinib was stopped and the patient received external-beam radiation to the retro bulbar space, consisted in a total dose of 30Gy, with benefits on visual symptoms. Unfortunately, despite good regression of brain lesions, a bone disease progression with pain was observed in September 2013. Patient was treated with two cycles of doxorubicine 60 mg/m2 once every three weeks. In November 2013, a TBS revealed a rapid lymphnodal and lung disease progression and patient received a new treatment with three cycles of Vinorelbine 30 mg/m2/weekly and 5-fluorouracil 750 mg/m2/die e.v. weekly, whit concomitant zoledronic acid bolus, 4 mg once every 28 days. A further clinical worsening led patient to exitus (Table 1).
|
Date |
Medical examination |
Diagnosis |
Treatment |
|
March 2009 |
Ultrasound examination |
9 mm nodule, in the right lobe of thyroid, with suspicious right latero-cervical neck lymphoadenopaty |
thyroidectomy plus a right latero-cervical lymphoadenectomy |
|
July 2009 |
First radioiodine treatments |
||
|
June 2010 |
Second radioiodine treatments (100 mCi 131I) |
||
|
July 2011 |
third radioiodine treatment |
||
|
February 2012 |
CT scan and WBS |
progression of disease with bilateral lung lesions, bilateral multiple jugular carotid lymphnodes and bone metastases localized in the IV thoracic rib |
|
|
May 2012 |
lenvatinib 24 mg total daily dose |
||
|
From May 2012 to March 2013 |
CT scan |
decrease of pulmonary nodules; bone disease progression |
|
|
May 2013 |
zoledronic acid (4 mg infusional dose) |
||
|
June 2013 |
cranial CT scan; fundoscopic examination; MRI |
multiple brain metastases and bilateral choroidal lesions |
|
|
July 2013 |
Stopping of Levatinib administration; external beam radiation (30Gy) |
||
|
September 2013 |
two cycles of doxorubicine(60 mg/m2 once every three weeks) |
||
|
November 2013 |
TBS scan |
rapid lymphnodal and lung disease progression |
Vinorelbine (30 mg/m2/weekly) and 5-fluorouracil (750 mg/m2/die e.v. weekly), whit concomitant zoledronic acid bolus, (4 mg once every 28 days) |
Table 1: Summury case report.
3. Discussion
Thetyrosine kinase inhibitors (TKIs) aim to inhibit tumour angiogenesis and have a significant role in treatment of thyroid cancer. A phase III trial (DECISION) of sorafenib in radioiodine (RAI)-refractory thyroid cancer showed a median progression-free survival (PFS) of 10.8 months in the sorafenib group, compared to 5.8 months in the placebo group. Lenvatinib, also approved for RAI-refractory thyroid cancer, is an antiangiogenic TKI that inhibits the VEGF1–3, PDGF, KIT, RET receptors, FGF1–4. FGFR plays a key role in the development of resistance against anti-angiogenic drugs. In a phase III trial (SELECT) on RAI-refractory DTC, the Lenvatinib group showed a PFS of 18.3 months, compared to 3.6 months in the placebo group [9]. Our patient with diagnoses of RAI refractory DTC, received treatment with lenvatinib 24 mg showing a good PFS and adequate safety in agreement with data of registrative trial.
The patient on progression to lenvatinib showed an aggressive disease with rare metastases localized in choroid in addition to lymph nodes, lung and bone. Metastatic thyroid carcinoma rarely involves the orbit. In spite of being infrequent from all cancer type, the most frequent origins of orbital metastases are breast, prostate, kidney and melanoma, and less frequently arising from prostate, kidney and gastrointestinal tract tumors [10]. Besides the 22 cases of thyroid carcinoma with metastases to the choroid reported in a review from 1979 to 2012 [11], other 10 cases have been reported up till now [12-21]. Among the 32 cases reported in literature, the most common primary tumor was papillary thyroid carcinoma, occurred in 13 cases [11-17]. In 9 cases primary tumour was follicular hystotype and in 6 cases medullary thyroid carcinoma [11, 18-21].
As in our case, choroidal metastases were reported later in the course of the disease. The diagnosis of choroidal metastasis from thyroid carcinoma is usually based on clinical judgment and results of non invasive diagnostic techniques such as ultrasonography, transillumination, CT, and/or MRI scanning. Because a very limited number of patients have been reported, no data exist describing the best and most effective treatment of this condition. Treatment options for choroidal metastases secondary to DTC included131I ablation therapy, external beam radiation and surgical enucleation. Enucleation is the treatment of choice in choroidal and/or orbital metastases causing significant loss of vision and/or persistent symptoms such as pain [22]. In our patient, external-beam radiation resulted in satisfactory regression of the bilateral choroidal masses and represents a valid option of treatment. Although infrequent, orbital metastasis from thyroid carcinoma are possible correlating with a worse prognosis.
4. Conclusion
Treatment with TKI is a standard of care in advanced RAI refractory DTC showing an advantage in PFS and a good tolerability. Although it is extremely rare, the possibility of choroidal metastasis should be considered in case of pain or loss vision in patient with long history of thyroid malignancy due to progression disease. Periodic ocular examination is necessary to detect these metastases earlier and even in case of asymptomatic presentation.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Acknowledgements
The authors thank the patient involved the study.
References
- Siegel R, Naishadham D, Jemal A. Cancer statistics. CA Cancer J Clin 63 (2013): 11-30.
- National Cancer Institute. Surveillance epidemiology and end results program: Cancer stat facts: thyroid cancer (2015).
- Schlumberger MJ. Papillary and follicular thyroid carcinoma.N Engl J Med 338 (1998): 297-
- Smit J. Treatment of advanced medullary thyroid cancer.Thyroid Res 6 Suppl 1(2013): S7.
- Keutgen XM, SadowskiSM, Kebebew E. Management of anaplastic thyroid cancer. GlandSurg 4 (2015): 44-51.
- Giuffrida D, Prestifilippo A, Scarfia A, et al. New treatment in advanced thyroid cancer.J Oncol (2012): 391629.
- Haugen BR, Alexander EK, Bible KC, et al. 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer: The American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid 26 (2016): 1-133
- NCCN Clinical Practice Guidelines in Oncology, Thyroid Carcinoma (2015).
- Laursen R, Wehland M, Kopp S, et al. Effects and Role of Multikinase Inhibitors in Thyroid Cancer.Curr Pharm Des 22 (2016): 5915-5926
- Arepalli S, Kaliki S, Shields CL. Choroidal metastases: origin, features, and therapy.Indian J Ophthalmol 63 (2015): 122-127
- Besic N, Luznik Z. Choroidal and orbital metastases from thyroid cancer.Thyroid 23(2013): 543-551
- Torun N, Reyhan M, Yapar AF, et al. Choroidal Metastasis of Papillary Thyroid Carcinoma Demonstrated on SPECT-CT.ClinNuclMed 41 (2016): 403-404
- Makhija C, Su YB, Goldner W. Unusual Case of Papillary Thyroid Carcinoma with Choroidal Metastasis.Thyroid 25 (2015): 860-864
- Kiratli H, Tarlan B, Söylemezoglu F. Papillary thyroid carcinoma: bilateral choroidal metastases with extrascleral extension.Korean J Ophthalmol 27 (2013): 215-218
- Fountas A, Tigas S, Giotaki Z, et al. Choroidal metastasis from papillary thyroid cancer: An unusual feature of a common disease.Ann Endocrinol (Paris) 78 (2017): 64-66
- Palaniswamy SS, Subramanyam P. Unusual Sites of Metastatic and Benign I 131 Uptake in Patients with Differentiated Thyroid Carcinoma.Indian J EndocrinolMetab 22 (2018): 740-750
- ChacónGonzález M, IbáñezMuñoz A, Rodríguez Vicente L, et al. Choroidal metastases as initial manifestation of a papillary thyroid carcinoma: A case report. Metástasis coroidea comoprimera manifestación de carcinoma papilar de tiroides: a propósito de un caso.ArchSocEspOftalmol 95 (2020): 94-97
- Papastefanou VP, Arora AK, Hungerford JL, et al. Choroidal metastasis from follicular cell thyroid carcinoma masquerading as circumscribed choroidal haemangioma.Case Rep OncolMed (2014): 251-817.
- Patil D, Kumaraswamy Kattepur A, Kodaganur Gopinath S, et al. Iodophilic synchronous phalangeal and choroidal metastasis from follicular thyroid carcinoma: a case report and review.Eur Thyroid J 3 (2014): 134-136
- Chowdhury MS, Awal MA. Choroidal Metastasis from Follicular Thyroid Carcinoma: A Rare Case Report.Bangladesh J. Nuclear Med 20 (2018): 155-158.
- Hong J. Bilateral Choroidal Metastases as Initial Presentation of Widespread Follicular Thyroid Cancer. The Medicine Forum 20 (2019): 18-19.
- Avram AM, Gielczyk R, Su L, et al. Choroidal and skin metastases from papillary thyroid cancer: case and a review of the literature. J Clin Endocrinol Metab 89 (2004): 5303-5307
