Treatment of Inter-MitraClip Regurgitation Due to Posterior Leaflet Cleft by Use of The Amplatzer Vascular Plug II device
Article Information
Neha M. Mantri, Gagan D. Singh, Thomas Smith, and Jason H. Rogers*
Division of Cardiovascular Medicine, University of California Davis Medical Center, Sacramento CA, 4860 Y Street, Suite 2820, USA
*Corresponding Author: Jason H. Rogers, Division of Cardiovascular Medicine, University of California
Davis Medical Center, Sacramento CA, 4860 Y Street, Suite 2820, USA
Received: 02 May 2017; Accepted: 05 May 2017; Published: 18 May 2017
View / Download Pdf Share at FacebookKeywords
Mitral Valve Surgery
Article Details
1. Introduction
Mitral valve surgery has historically been the treatment of choice for many patients with severe symptomatic mitral regurgitation (MR) due to primary degenerative valve disease and less often for those with secondary functional MR. However, nearly half of patients with significant MR are not offered therapy due to prohibitive surgical risk [1]. As a result, transcatheter therapies have been developed to treat symptomatic MR in these patients.
The MitraClip system (Abbott Vascular, Santa Clara CA) is an FDA-approved transcatheter therapy for high-risk patients with severe symptomatic MR. There remain significant technical challenges to the MitraClip procedure particularly in those patients with complex mitral valve anatomy. Challenging scenarios could include patients with wide flail gaps, focal or diffuse calcification, restricted leaflets, and the presence of clefts or deep scallops which can interfere with leaflet grasping. When significant residual MR exists and additional MitraClips are not anatomically feasible, current options are limited.
Successful implantation of the MitraClip and determination of the number of clips needed is highly dependent on valve leaflet anatomy and degree of resultant regurgitation or stenosis observed intra-procedurally after deployment of each clip. Mechanistically, the MitraClip system involves active grasping of both leaflets, which ensures security and enhances native leaflet coaptation. However, variable leaflet anatomy consisting of clefts or degenerated leaflet anatomy risks leaving residual jets between clips. The Amplatzer Vascular Plug (AVP) II and Amplatzer Duct Occluder (ADO) II devices, both constructed of a self-expanding nitinol mesh have been used to occlude residual regurgitant jets after MitraClip therapy. This case highlights a unique treatment strategy for intra-clip residual MR with the utilization of the AVP II device.
2. Case Report
An 88-year-old male with severe aortic stenosis, severe primary mitral regurgitation due to a flail posterior leaflet, diastolic heart failure (ejection fraction 70%), hypertension, type II diabetes mellitus, and hyperlipidemia presented to our emergency department with sudden onset of palpitations and chest pressure. He had developed NYHA III symptoms approximately three months prior to admission, with intermittent, progressive, lower extremity edema and dyspnea on exertion. On admission, he was found to be in rapid atrial fibrillation and in acute congestive heart failure exacerbation. He underwent transesophageal echocardiography (TEE) with direct current cardioversion and was placed on atrioventricular nodal agents and rhythm suppressive therapy with beta-blockers and amiodarone.
Given a prohibitively high Society of Thoracic Surgeon (STS) score of 11.6% for combined surgical aortic and mitral valve replacements, he underwent transcatheter aortic valve replacement (TAVR) with plan for subsequent MitraClip therapy. Given his severe, symptomatic aortic stenosis (aortic valve area of 0.69 cm2 and mean aortic valve gradient of 40 mm Hg), he initially underwent successful trans-femoral implantation of a 26 mm Edwards- Sapien S3 (Edwards, Irvine CA) aortic valve. The patient was placed on medical therapy with aggressive diuresis and afterload reduction. On follow-up, he had persistent NYHA III symptoms. Due to progressive dyspnea with minimal exertion, he was referred for transcatheter mitral valve repair [2-4].
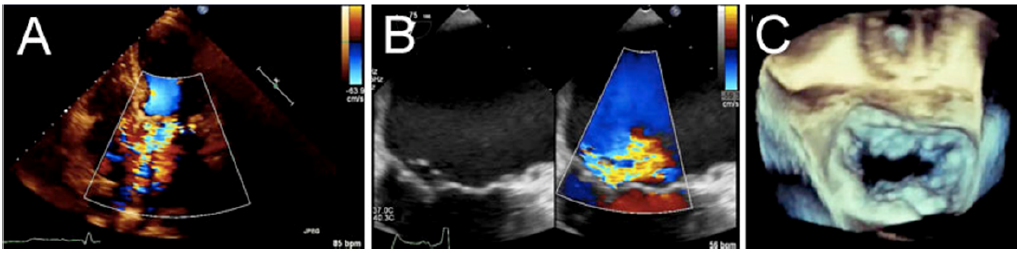
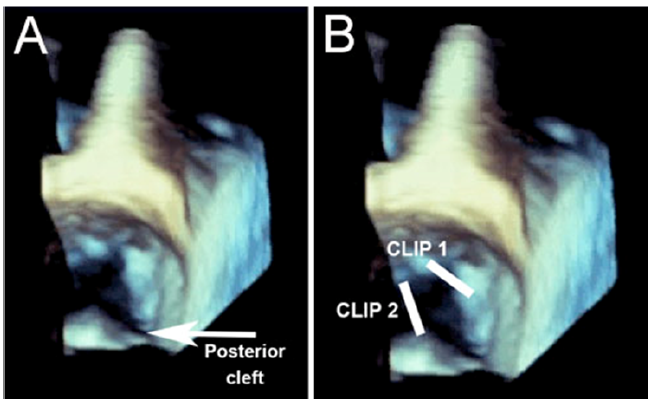
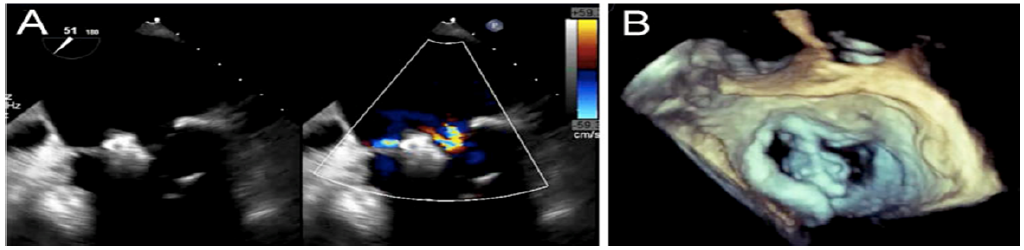
A transthoracic echocardiogram noted preserved left ventricular (LV) systolic function with an ejection fraction of 55% and 4+ mitral regurgitation. A transesophageal echocardiogram (TEE) showed primary mitral regurgitation with a flail posterior leaflet (P2/P3-- Carpentier II due to leaflet prolapse and chordal rupture) resulting in severe MR and a cleft between P2/P3 (Figure 1). Three-dimensional reconstruction demonstrated a large posterior cleft between P2/3 scallops (Figure 2A), which resulted in a complex regurgitant jet directed in the antero-lateral direction. Pre-procedural transmitral gradient was 1.6 mm Hg.
Pre-procedure catheterization revealed no significant coronary artery disease, and hemodynamics were significant for: mean right atrial pressure 20 mm Hg, mean pulmonary artery pressure of 34 mm Hg, mean wedge pressure of 19 mm Hg, mean left atrial pressure of 27 mm Hg, with end expiratory V waves of 57 mm Hg.
Figure 1: A. Baseline trans-thoracic echocardiogram with color Doppler demonstrating initial severe, 4+ mitral regurgitation B. Trans-esophageal echocardiogram post transcatheter aortic valve replacement showing severe central/medial MR from P2/P3 prolapse. C. 3-dimensional transesophageal echocardiogram baseline showing P2/P3 flail with chordal rupture.
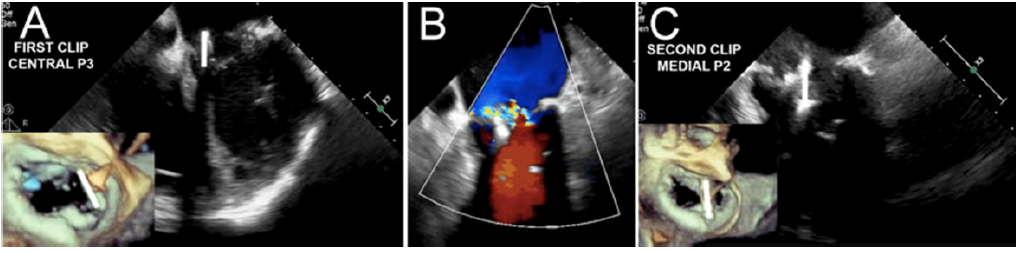
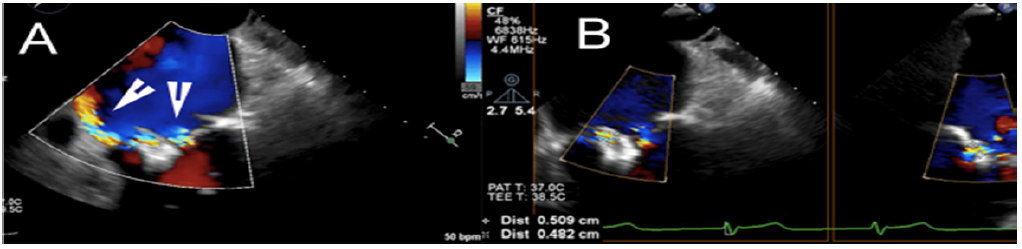
The procedural strategy involved implantation of two MitraClips straddling the posterior leaflet cleft. The first clip was planned for deployment in the central A3/P3 aspect and the second clip at the medial A2/P2 aspect (Figure 2B) with assessment of residual MR. Under general anesthesia, fluoroscopic, and TEE guidance, the first MitraClip was advanced via the transseptal route to the area of regurgitation over the central A3/P3 aspect (Figure 3A). The leaflets were grasped with one attempt. Echocardiographic analysis confirmed reduction in MR from severe (4+) to moderate (3+) (Figure 3B). The clip delivery system (CDS) was removed and an additional CDS was inserted. The second clip was positioned and deployed over the medial A2/P2 aspect with one grasp attempt (Figure 3C). After final grasp and tightening, residual MR was noted to be 2-3+. Interrogation by TEE demonstrated severe eccentric wall-hugging jet of “inter-clip” MR (Figure 4).
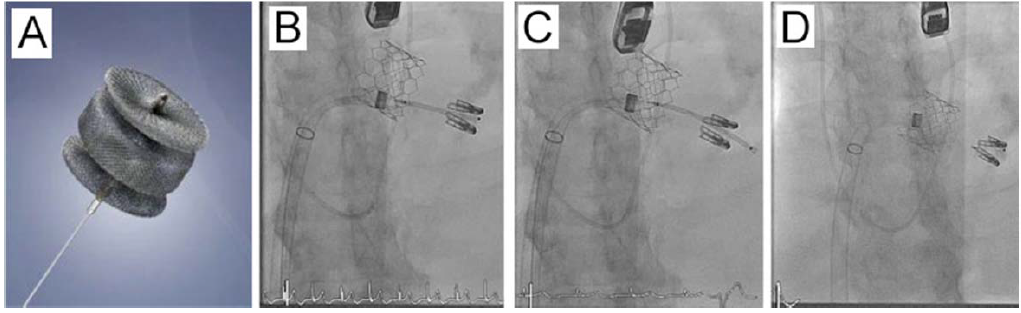
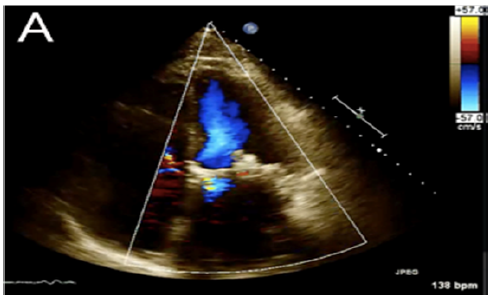
Based on fluoroscopic and TEE appearance and measurements, the 2nd clip could not be positioned any closer to the first clip due to presence of the posterior cleft. Alternatively, an additional clip could not be placed for similar reasons. However, measurements indicated that the residual jet was small enough for occluder placement. The Amplatzer Vascular Plug (AVP) II occluder device was utilized; the AVP II device differs from the ADO II device in that the waist and two retention discs are all the same diameter. A 6 F sheath was placed into the MitraClip guide catheter and then a 6 Fr 110 cm MP guide catheter was introduced the MitraClip guide into the left atrium. After measurement of the defect size by TEE (size 4.8 x 5.1 mm), a 10 mm AVP II occluder was selected. The inter-clip space was then wired using a straight Terumo wire and the MP guide was advanced between the two clips under fluoroscopy (Figure 5 A-D). Next, the 10mm AVP II was advanced through the guide and the distal retention disk was deployed. The system was retracted until in appropriate position and the remainder of the AVP was unsheathed and deployed. We achieved significant reduction in MR from 4 + to 1+ (Figure 6) with a final transmitral gradient of 2 mmHg. Post-procedure hemodynamics demonstrated a reduction in mean left atrial pressure to 17 mm Hg, with end expiratory V waves of 22 mm Hg.
Figure 3: A. Intra-procedural trans-esophageal echocardiogram and superimposed 3-D reconstruction highlighting the location of the first clip location at central P3 position. B. Trans-esophageal color Doppler demonstrating mild- moderate MR remaining after first clip. C. Intra-procedural trans-esophageal echocardiogram and superimposed 3-D reconstruction highlighting the location of the second clip at medial P2 position.
After withdrawal of the MitraClip guide catheter back into the right atrium, significant right to left shunting through the interatrial septum (IAS) was noted. A MPA catheter was then used to re-access the atrial septal defect (ASD) and a 0.035’ J-wire placed in the left upper pulmonary vein. An 8 Fr Torqvue delivery sheath was advanced into the left atrium, and a 10 mm Amplatzer Septal Occluder was deployed across the ASD. Final TEE assessment demonstrated significant reduction in MR grade from 4+ to 1+, systolic predominance in pulmonary vein flow, and a final trans-mitral diastolic gradient of 6-8 mm Hg.
The patient was successfully extubated and transferred to the post-anesthesia care unit. The patient had no acute or in-hospital complications. He was successfully discharged on hospital day nine with continued medical therapy (Lasix, ACE inhibitor, dihydropyridine calcium channel blocker) and rivaroxaban for stroke prophylaxis. The patient received a 30-day follow up trans-thoracic echocardiogram demonstrating adequate valve function (Figure 7).
3. Discussion
We have described several unique features of this case. The presence of complex degenerative anatomy with flail leaflets, loss of chordal support, and deep clefts can lead to an inadequate reduction of MR despite placement of two or more MitraClips. Challenging scenarios also include patients with wide flail gaps, focal or diffuse calcification, or restricted leaflets, which can all complicate leaflet grasping. In particular, at the area of maximal MR (which frequently coincides with the region of maximal leaflet pathology), it is often difficult to grasp the leaflets for additional clip placement. When significant residual or inter-clip MR is seen, current treatment options are limited. We demonstrate a treatment strategy through utilization of the AVP II device to treat residual MR from a deep posterior leaflet cleft. In our case, when 2-3+ residual inter-clip MR was visualized, a 10 mm AVP II was placed with reduction to 1+ mitral regurgitation.
When a deep leaflet cleft is visualized, we have demonstrated the utility of intra-procedural planning with 3-D TEE to localize clip placement and possible occluder location if inter-clip MR persists. In this case, positioning of the two MitraClips was dependent on the location of the cleft, as we used the clips to “straddle” the cleft. Since an additional clip could not be placed at the cleft location, we adopted a “bail out” strategy utilizing a retrievable low profile device with a flexible delivery cable system.
There have been other reports utilizing this occluder technique. Taramasso et al. demonstrated the first-in-man case report of a patient with significant residual “intra-clip” jet treated by the implantation of an AVP II device. In this report, 4 years after transcatheter mitral repair with the MitraClip, a 64-year old gentleman presented with severe MR recurrence. Two further MitraClips were placed, with residual intra-clip MR and no further room for additional clips. An 18 mm AVP II was successfully deployed between the two clips with final echocardiography showing residual mild MR without evidence of mitral stenosis [5]. In a larger published series, Kubo et.al demonstrated the value of the Amplatzer Duct Occluder II (ADO II) device for the treatment of residual intra-clip or commissural MR. Nine patients with inadequate MR reduction (MR grade 3+ or 4+) despite best attempt at MitraClip therapy
were treated over a 7-month period with the MitraClip system. They were treated with the ADO II device at the timeof the initial MitraClip procedure (n = 7) or during a separate, second procedure (n = 2).
The investigators demonstrated significant, acute MR reduction using the ADO II device in all 9 patients [6]. Potential limitations and risks of occluder therapy do exist. These include inappropriate device sizing, device embolization, hemolysis, and leaflet erosion. In order to prevent many of the aforementioned complications, defining the location and size of the residual regurgitant jets through fluoroscopy, echocardiography, and clinical judgment is of utmost importance. In all 9 patients, Kubo showed MR reduced to < 2+, with decreases in left atrial pressure and normalization of systolic pulmonary vein flow. Importantly, there was no increase in the transmitral diastolic gradient after ADO II deployment, nor was there evidence of hemolysis. One significant complication did arise during this technique, which involved ADO II embolization into the right coronary artery, resulting in an inferior ST-segment elevation myocardial infarction 9 hours after the procedure. Although the mechanism was not clear, it is presumed that the device was undersized to that of the defect or that leaflet integrity at the occluder location was suboptimal.
An additional application of the AVP II has been seen in treatment of paravalvular leak (PVL), a frequent complication after the implantation of a prosthetic valve. Due to the high risk associated with surgical re-operation to close the defect or replace the prosthesis, the development of newer devices, including the AVP II and III, have been proposed as an alternate strategy for percutaneous closure. In a recent study by Sanchez-Recalde et al., closure was attempted for 23 PVL (17 mitral and 6 aortic). In mitral PVL, the first option was to implant an AVP III device, although in some cases an ADO was finally used due to the morphology, PVL size, or interference of the AVP III with a disc in the prosthesis. When choosing the device the largest and smallest diameters of the defect were measured with 3-D TEE reconstruction, and a device equal to, or 1-2 mm larger than the defect was used. Overall, the ADO II was used in 2 (9%) of cases, while the AVP II was used in 18 (86%) of cases [7]. In our case the AVP II was utilized rather than the ADO II occluder due to the side availability of diameters, ranging from 3 to 22 mm. The ADO II occluder has waist sizes of only 5 and 6 mm and it was felt this was too small for the defect. In regards to structure, the most significant difference between the AVP II and ADO devices is the difference in size between the retention discs disc and central waist. The ADO has a 4-6 mm difference, while the AVP II device has a similar size; this may, theoretically, contribute to better anchoring of the AVP II device.
In summary, given the relatively limited clinical experience with the use of occluder devices for the treatment of residual MR after MitraClip therapy, operators should always adopt a ”MitraClip first” and “occluder second only if needed” approach. Whether or not performing occluder therapy at the time of the index procedure is superior to a later staged procedure is not known. It appears that the main early risk is device embolization, which may be mitigated by performing a gentle “tug test” prior to device release.
4. Conclusion
In conclusion, we have shown a novel and effective intra-procedural treatment option for inter-clip MR, particularly
when the addition of an adjunctive clip is not feasible. As the use of transcatheter therapies for MR increases, particularly in patients with prohibitively high surgical risk, operators often face unique challenges given the complex anatomy of the mitral valve. We have encountered wide flail gaps, focal or diffuse calcification, restricted leaflets, and the presence of deep clefts or scallops, all of which can interfere with leaflet grasping. Moreover, with the use of more than a single clip, the risk of residual jets between clips increases, necessitating further recommendations on treatment options for inter-clip MR.
We describe a unique case in which the MitraClip device was utilized first, however subsequent addition of the AVP II occluder, served to adequately treat severe primary MR due to a flail posterior leaflet and rupture chord. When a deep leaflet cleft is visualized, we have demonstrated the utility in intra-procedural planning with 3-D TEE to localize clip and utilize occluder placement if inter-clip MR is encountered. Limited case series have demonstrated the value of the ADO II device for inter-clip or commissural MR, however, we provide step by step technique which can be utilized in treatment of substantial inter-clip MR. Given the relatively limited clinical experience, the procedure is heavily operator dependent; it is encouraged to utilize 3D reconstruction for pre-procedural planning and discuss risks and benefits with the patient prior to the procedure.
References
- Estévez-Loureiro, Rodrigo. Effect of advanced chronic kidney disease in clinical and echocardiographic outcomes of patients treated with MitraClip system. International Journal of Cardiology 198 (2015): 75-80.
- Glower DD, S Kar and A Trento. Percutaneous mitral valve repair for mitral regurgitation in high-risk patients: results of the EVEREST II study. Journal of American College of Cardiology 64 (2014): 172-181.
- Paranskaya L, D’Ancona G, et al. Residual mitral valve regurgitation after percutaneous mitral valve repair with the MitraClip system is a risk factor for adverse one-year outcome. Catheter Cardiovasc Interv 81 (2014): 609-617.
- Feldman T, Wassermann HS, Hermann HC, et al. Percutaneous mitral valve repair using the edge-to-edge technique: Six month results of the EVEREST Phase I Clinical Trial. J Am Coll Cardiol 46 (2005): 2134?2140.
- Taramasso M, Zuber M, Gruner C, Gaemperli O, Nietlispach F, et al. First-in-man report of residual “intra-clip” regurgitation between two MitraClips treated by Amplaztzer Vascular Plug II. EuroIntervention 11 (2016):1537-40.
- Kubo S, Cox JM, Mizutani Y, et al. Transcatheter procedure for residual mitral regurgitation after MitraClip implantation using Amplatzer Duct Occluder II. J Am Coll Cardiol Intv 9 (2016): 1280-1288.
- Sanchez-Recalde A, Moreno R, et al. Immediate and Mid-term Clinical Course After Percutaneous Closure of Paravalvular Leakage. Rev Esp Cardiologia 67 (2014): 615-623.