Psychosocial Interventions for Enhancing Social Functioning in Severe Mental Illness: A Systematic Review and Meta-analysis
Article Information
Tanzeela Saeed1, Ghazala S. Virk2, Muhammad Sohail S. Mirza3*, Mehwish Aqueel4, Fnu Karishma5, Maaz Aqueel6, Taha Nadeem7, Muhammad Abdul Manan Mangral8, Binish Essani9
1Services Institute of Medical Sciences, Lahore, Pakistan
2Avalon University School of Medicine, Willemstad, Curacao
3Shandong University School of Medicine, Jinan, China
4Rosalind Franklin University of Medicine and Science, Illinois, USA
5Ghulam Muhammad Mahar Medical College, Sukkur, Pakistan
6University of Twin Cities, Minnesota, USA
7Allama Iqbal Medical College, Lahore, Pakistan
8Allama Iqbal Medical College, Lahore, Pakistan
9Jinnah Medical and Dental College, Karachi, Pakistan
*Corresponding Author: Muhammad Sohail S. Mirza, MBBS. Shandong University School of Medicine, Jinan, China.
Received: 30 July 2025; Accepted: 06 August 2025; Published: 15 August 2025.
Citation: Tanzeela Saeed, Ghazala S. Virk, Muhammad Sohail S. Mirza, Mehwish Aqueel, Fnu Karishma, Maaz Aqueel, Taha Nadeem, Muhammad Abdul Manan Mangral, Binish Essani. Psychosocial Interventions for Enhancing Social Functioning in Severe Mental Illness: A Systematic review and Meta-analysis. Journal of Psychiatry and Psychiatric Disorders 9 (2025): 259-268.
View / Download Pdf Share at FacebookAbstract
Background: Social functioning is a core domain of recovery in severe mental illness (SMI), yet remains under-addressed by pharmacological treatment. Psychosocial interventions offer promising avenues to improve social outcomes, but evidence remains fragmented. This review aims to evaluate psychosocial interventions in improving social functioning among individuals with SMI and explore how intervention type, comparator condition, and study quality influence outcomes. Methods: This review analyzed seven randomized controlled trials (RCTs), including a total of 1,093 participants. A random-effects model was used to calculate pooled standardized mean differences (SMDs). Subgroup analyses were conducted based on intervention type, control condition, and risk of bias. Results: Psychosocial interventions were associated with a significant improvement in social functioning (pooled SMD = 0.61, 95% CI: 0.12–1.09, p = 0.01). Subgroup analyses showed particularly strong effects for mindfulness-based approaches (SMD = 1.48) and those compared with treatment-as-usual (SMD = 1.14). In contrast, app-based interventions had a negative effect (SMD = –0.81). Differences by control condition were statistically significant (p < 0.00001). When studies with a high risk of bias were excluded in sensitivity analysis, the overall effect size increased (SMD = 0.94, 95% CI: 0.28–1.61). However, heterogeneity was high across studies (I² > 90%). Conclusion: Psychosocial interventions demonstrate a moderate, significant impact on social functioning in SMI, with variability influenced by intervention modality and comparator type. These findings highlight the need for function-focused psychosocial programs as essential components of recovery-oriented care.
Keywords
Psychosocial interventions, Severe mental illness (SMI), Social functioning, Schizophrenia, Bipolar disorder, Cognitive behavioral therapy (CBT).
Psychosocial interventions articles; Severe mental illness (SMI) articles; Social functioning articles; Schizophrenia articles; Bipolar disorder articles; Cognitive behavioral therapy (CBT) articles.
Article Details
1. Introduction
Any mental, behavioral, or emotional disorder (substance use and developmental disorders excluded) resulting in serious functional impairment that substantially interferes with, or limits one or more life activities is SMI [1]. SMI is known to have significant social and financial implications, with detrimental effects on individuals, their families, and society at large [2, 3]. According to the World Economic Forum, by 2030, mental illness will be responsible for over half of the worldwide economic burden resulting from non-communicable diseases. Individuals with SMI are more likely to experience poverty, unemployment, and substandard housing, all of which have an adverse effect on their social inclusion and worsen mental illness. Improving social outcomes for this group is therefore of interest to clinicians, legislators, and numerous other stakeholders. However, this has turned out to be an extremely difficult undertaking [4]. Before the formalization of diagnostic criteria concerning type, severity, impairment, or illness duration, the term severe and persistent mental illness (SPMI) was utilized for many years [5]. Researchers sought to determine the proportion of individuals who met the SPMI criteria by applying specific criteria to a sample from an urban community mental health center, where 36% of participants had been diagnosed with schizophrenia or affective disorder. Their findings indicated that the percentage of individuals meeting the SPMI criteria ranged from 4% to 88%, depending on the criteria applied [6]. Social functioning, which encompasses the ability to fulfill important societal roles such as those of a worker, student, family member, partner, or friend [7], is widely recognized as a key measure of recovery and a significant predictor of quality of life in individuals with severe mental illness [8]. Both schizophrenia and bipolar disorder are characterized by impairments in social functioning, which seem to arise from multiple contributing factors. An increasing number of studies have identified robust associations between different types of affective dysregulation and reduced social functioning in individuals with both affective and non-affective psychotic disorders [9, 10]. This indicates that affective dysregulation might play a distinct role in contributing to social impairments in psychosis, separate from other influences such as neurocognitive or social-cognitive deficits. Since emotional experiences are formed, expressed, and regulated within social contexts, it is perhaps expected that those with difficulties managing emotions struggle in social situations [11]. This suggests that affective dysregulation may uniquely contribute to social difficulties in psychosis, acting independently from other factors like neurocognitive and social-cognitive deficits. Since emotional experiences are formed, expressed, and regulated within social contexts, it is perhaps expected that those with difficulties managing emotions struggle in social situations [12, 13].
Psychosocial interventions, such as case management, rehabilitation, and assertive community treatment, often involve visiting patients at home, serving as a model for a service organization, or providing rehabilitation activities to help patients lead a life outside of the hospital structure [14]. Assertive community treatment decreased the likelihood of relapse after six months, but case management's confidence intervals contain the potential for no difference with standard care (just three studies), indicating that rehabilitation had encouraging results in preventing relapse. These findings align with earlier, more comprehensive assessments that concluded aggressive community treatment had no protective impact on case management [15] but were successful in preventing recurrence [16].
Over a decade, enhancing mental well-being has been linked to an up to 8.2-fold reduction in the likelihood of developing mental illness in individuals without such conditions [17, 18], and it also increases the probability of recovery for those already experiencing mental illness [19, 20]. A recent scoping review [21] Identified over 80 peer-reviewed studies that support the notion that indicators or states of mental well-being can exist independently of a mental illness diagnosis. These studies also suggest that while both constructs share some common antecedents, they also have distinct ones. Furthermore, each construct requires measurement through specific scales, and psychological interventions may enhance both mental well-being and illness indicators, or they may affect only one of these areas [22]. Despite the increased research activity in this domain, the existing body of evidence remains fragmented due to variations in study design, participant demographics, and outcome measures. Moreover, the extent to which therapies improve quantifiable social functioning outcomes in individuals with SMIs has not been comprehensively reviewed in recent decades. There is an urgent need for a prompt and high-quality synthesis to aid researchers, clinicians, and policymakers in selecting and implementing evidence-based interventions. This review seeks to address this gap by examining the effectiveness of psychosocial interventions on social functioning outcomes in SMIs. By focusing on recent human RCTs with well-established outcome measures, this review aims to compile high-quality and generalizable evidence for application in both clinical practice and further research.
2. Materials and methods
2.1 Data Sources and Search Strategy
This review adhered to the PRISMA 2020 guidelines. An extensive literature search was conducted using PubMed/MEDLINE, Google Scholar, the Cochrane Central Register of Controlled Trials (CENTRAL), and ScienceDirect, encompassing all records from their inception to the present. The search strategy employed a mix of Medical Subject Headings (MeSH) and free-text terms related to psychosocial interventions, social functioning, and severe mental illness. Furthermore, reference lists from the chosen articles and relevant reviews were scrutinized to uncover additional eligible studies.
2.2 Inclusion and Exclusion Criteria
The review sought to identify evidence from RCTs assessing the effectiveness of psychosocial interventions in enhancing social functioning in patients with SMI, i.e., schizophrenia spectrum disorders, bipolar disorder, MDD, and schizoaffective disorder. The inclusion criteria included studies with participants aged 18 years or older with a formal diagnosis of SMI based on standard diagnostic criteria, like the DSM or ICD. Only peer-reviewed English-language articles were considered. Eligible interventions comprised any structured psychosocial therapy intended to enhance social functioning, such as cognitive behavioral therapy (CBT), social skills training (SST), supported employment, family psychoeducation, cognitive remediation, assertive community treatment, peer support programs, and mindfulness-based interventions. Studies were required to include a comparison group receiving treatment as usual (TAU), placebo, wait-list control, or an alternative psychosocial intervention. The primary outcome was social functioning, assessed using validated instruments such as the Social and Occupational Functioning Assessment Scale (SOFAS), Social Functioning Scale (SFS), Personal and Social Performance Scale (PSP), or Global Assessment of Functioning (GAF). Studies that reported only qualitative outcomes or used unvalidated measures were excluded. Non-randomized studies, observational designs, cross-sectional studies, case series, reviews, and conference abstracts without accessible full texts were also excluded.
2.3 Study Selection Process
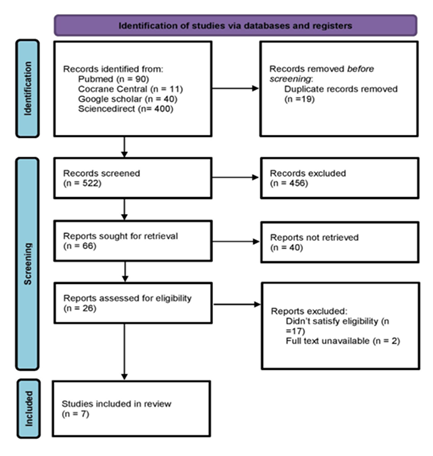
All records identified were organized using reference management software, and duplicate entries were eliminated before the screening process began. Two reviewers independently evaluated the titles and abstracts, after which they conducted a thorough assessment of the full-text articles. Any disagreements were addressed through discussion or, when needed, by involving a third reviewer. The PRISMA 2020 flow diagram illustrates the selection process in detail (Figure 1).
Data were extracted using a standardized template, which included details on study design, participant characteristics, intervention and control conditions, social functioning outcomes, effect sizes, follow-up periods, and risk of bias. The methodological quality of the included RCTs was evaluated using the Cochrane Risk of Bias 2 (RoB 2) tool.
2.4 Statistical Analysis
A meta-analysis was performed using a random-effects model when appropriate to account for the anticipated differences among studies. For continuous outcomes, SMDs with 95% CIs were computed. The I² statistic was utilized to assess statistical heterogeneity. Subgroup analyses were designed based on intervention type, SMI diagnosis, and study quality. Sensitivity analyses were conducted to test the stability of the results by omitting studies with a high risk of bias.
3. Results
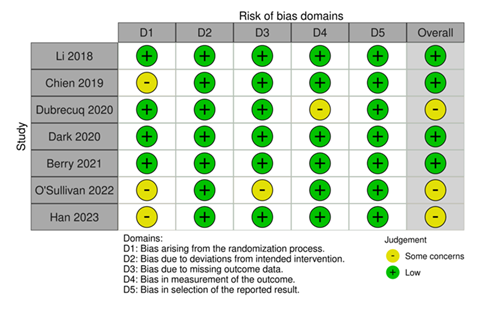
A comprehensive search across multiple databases yielded 541 records, with contributions from PubMed (90), Cochrane Central (11), Google Scholar (40), and ScienceDirect (400). Following the removal of 19 duplicate entries, 522 records were subjected to a screening process based on their titles and abstracts. This process resulted in the exclusion of 456 records, leaving 66 full-text articles for further eligibility evaluation. After a thorough review, nineteen studies were excluded because they either did not meet the eligibility criteria or lacked full-text access. A total of seven studies, with some low risk of bias (Figure 2), were included in the final review.
The studies that were included involved a total of 1,093 participants, with 550 in the intervention groups and 543 in the control groups. A diverse range of psychosocial interventions was represented, including cognitive-behavioral therapies, mindfulness-based programs, digital and social media interventions, and social cognition or skills training. The control conditions varied and included TAU, face-to-face psychotherapy, enhanced standard care (ESC), and app-based comparators. Social functioning was the primary outcome across all studies and was assessed using validated scales, including the GAF, PSP, SLOF, and SFS. The summary of the studies included is shown in Table 1.
Table 1: Characteristics of included studies
3.1 Overall Meta-Analysis
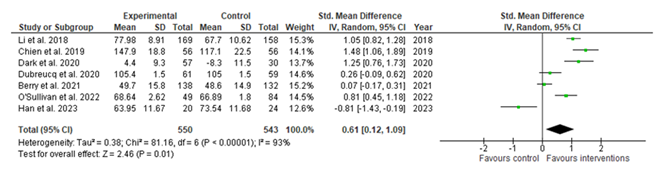
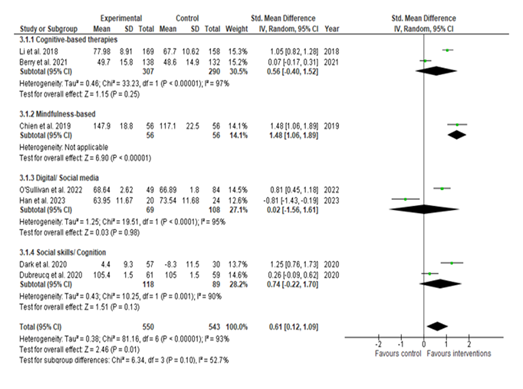
Across all studies, psychosocial interventions had a moderate and statistically significant effect on improving social functioning among individuals with severe mental illness. The pooled SMD was 0.61 with a 95% CI of 0.12 to 1.09, and the test for overall effect was significant (Z = 2.46, p = 0.01). However, there was substantial heterogeneity across studies, with an I² value of 93%, Tau² of 0.38, and Chi² of 81.16 (df = 6, p < 0.00001), indicating considerable variation in effect sizes across the included trials (Figure 3).
3.2 Subgroup Analysis by Type of Control
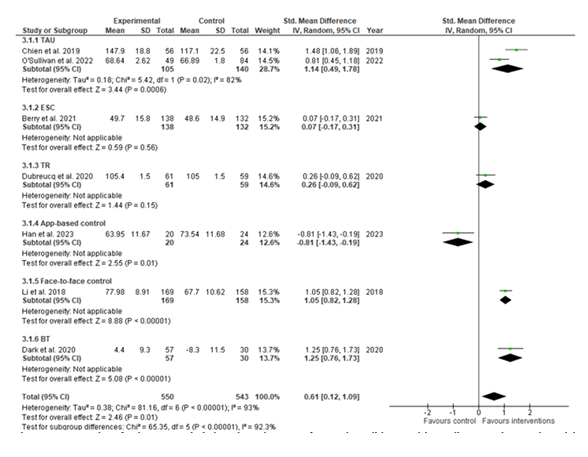
Subgroup analysis based on the type of control revealed notable differences. Interventions compared to TAU yielded the strongest effect, with a pooled SMD of 1.14 (95% CI: 0.49 to 1.78, p < 0.001). Similarly, interventions outperformed face-to-face and therapeutic rehabilitation controls, which also demonstrated statistically significant benefits. Conversely, one study using an app-based comparator showed a negative effect favoring the control condition (SMD = -0.81, 95% CI: -1.43 to -0.19) [29]. The test for subgroup differences was significant (Chi² = 65.35, df = 5, p < 0.00001), suggesting that the type of control condition played a significant role in influencing outcomes (Figure 4).
3.3 Subgroup Analysis by Type of Intervention
When categorized by the nature of the psychosocial intervention, mindfulness-based interventions demonstrated the largest positive effect, with an SMD of 1.48 (95% CI: 1.06 to 1.89). Social cognition and skills-based interventions also showed favorable results, though the pooled effect did not reach statistical significance. Digital or social media-based interventions yielded mixed results and were associated with a negligible pooled effect (SMD = 0.02, 95% CI: -1.56 to 1.61). Cognitive-based therapies demonstrated a modest but non-significant effect (SMD = 0.56, 95% CI: -0.40 to 1.52). The test for subgroup differences by intervention type was not statistically significant (Chi² = 6.31, df = 3, p = 0.10), indicating that intervention modality alone did not account for the observed heterogeneity (Figure 5).
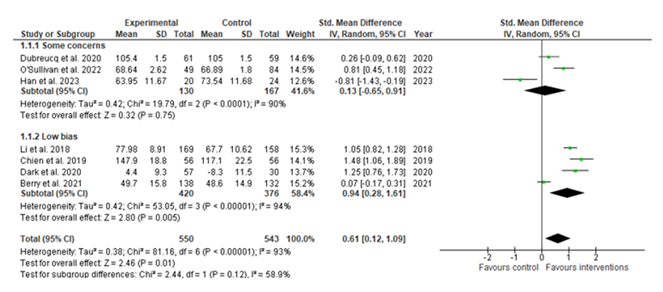
3.4 Risk of Bias and Quality-Based Subgroup Analysis
The RoB 2 tool was used to evaluate the risk of bias. Of the included studies, three were classified as having some concerns, and four were deemed low risk. The pooled analysis using a random-effects model demonstrated a statistically significant effect favoring the intervention, with an SMD of 0.61 (95% CI: 0.12 to 1.09, p = 0.01). Subgroup analysis indicated that studies with low risk of bias showed a significant benefit (SMD: 0.94, 95% CI: 0.28 to 1.61, p = 0.005), whereas studies with some concerns demonstrated no statistically significant effect (SMD: 0.13, 95% CI: -0.65 to 0.91, p = 0.75). The test for subgroup differences was not statistically significant (Chi² = 2.44, p = 0.12), suggesting no conclusive evidence that the observed effect differed by risk of bias level. However, the direction and magnitude of the effect were more favorable in trials with low risk of bias. Overall heterogeneity was high (I² = 93%), indicating considerable variability among studies. These findings highlight the potential benefit of the intervention, particularly in methodologically robust trials, while also emphasizing the need for cautious interpretation due to the high heterogeneity (Figure 6).
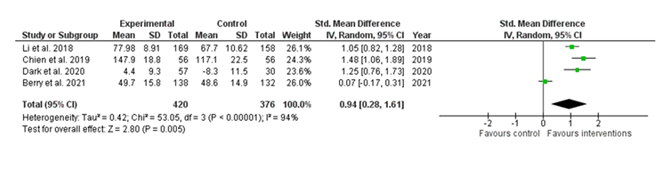
3.5 Sensitivity Analysis
A sensitivity analysis was conducted by excluding the three studies with some concerns to assess the robustness of the main findings. The analysis of the remaining four studies showed an increased and statistically significant pooled effect size of 0.94 (95% CI: 0.28 to 1.61), with a Z-value of 2.80 (p = 0.005). Heterogeneity remained high (I² = 94%), but this finding suggests that the overall effect observed in the main analysis was sensitive to the inclusion of low-quality studies and may be more reliable when limited to trials of moderate or high methodological rigor (Figure 7).
Discussion
This meta-analysis demonstrated that psychosocial interventions exert a statistically significant and moderately strong effect on improving social functioning in individuals with SMI. The pooled SMD of 0.61 (95% CI: 0.12–1.09) aligns with previous meta-analyses that have consistently emphasized the efficacy of psychosocial modalities, particularly when embedded in collaborative, structured care models. For example, a meta-analysis by Patel et al. [30] found a pooled SMD of 0.84 (95% CI: 0.49–1.19), with even larger effects (SMD = 0.93) observed at follow-up periods beyond 12 months. These findings reinforce the idea that social functioning improvements may be more gradual and durable over time, suggesting that social gains typically lag behind symptomatic improvement [31, 32]. A key contribution of our study is its examination of heterogeneity across intervention types and control groups, which provides a more nuanced understanding of contextual effectiveness. Our subgroup analysis showed that interventions compared to TAU yielded significantly larger effects than those compared to active digital or application-based controls. This aligns with previous studies [24], where participants receiving mindfulness-based psychoeducation had significantly better post-intervention scores on the SLOF scale compared to those receiving TAU or CPGP controls (between-group mean difference = 18.8–43.3; p < 0.01). While our subgroup analysis indicated that digital or app-based interventions produced smaller effect sizes compared to therapist-led interventions, the broader literature suggests they are both feasible and well-tolerated among individuals with SMI [33]. Despite initial concerns around limited access to smartphones, internet connectivity, and technological familiarity, most participants in digital intervention studies have reported high levels of usability and engagement [34]. In fact, some users voluntarily accessed additional content beyond the required sessions, indicating intrinsic motivation and user satisfaction. Although a subset of individuals—particularly those with limited prior exposure to technology [35]—did encounter challenges, these were often overcome with structured guidance, such as peer coaching or introductory training modules [36]. This suggests that the effectiveness of digital interventions may be enhanced when paired with human support systems. Future research should explore blended approaches that integrate digital tools with therapeutic guidance to maximize outcomes while maintaining accessibility.
The type of intervention also moderated the outcomes. Mindfulness-based interventions showed the largest effect size in our analysis (SMD = 1.48), consistent with the studies reporting that such interventions not only improve social functioning but also target negative symptoms such as apathy, withdrawal, and emotional blunting [37-39]. This is especially relevant given the limited efficacy of pharmacotherapy in these domains. Similarly, cognitive remediation (CR) and social cognition training (SCT) have shown promise in treating cognitive impairment. Previous research has found significant long-term gains in both social functioning and expressive/experiential negative symptoms following CR compared to healthy behavior training, further underscoring the relevance of psychosocial methods targeting cognitive-affective mechanisms [40, 41]. Moreover, our findings are in line with evidence suggesting that early intervention windows, especially within the first six months, may be particularly sensitive periods for psychosocial gains. It has been reported that targeting attenuated psychotic symptoms (APS) during this period can mediate improvements in role and social functioning [42, 43]. This may explain the stronger effects seen in shorter-term interventions within our dataset and supports the argument for early and intensive engagement. Interestingly, our study highlights the moderating role of study quality. Sensitivity analyses showed that excluding high-risk studies or studies with some concerns increased the pooled effect size (SMD = 0.94), and subgroup analyses indicated that studies rated as low risk yielded stronger effects than high-risk studies. This corresponds with previous reviews, where methodological rigor significantly influenced effect estimates [44, 45], and underscores the need for robust trial designs in future psychosocial intervention research. This study possesses several methodological strengths. It integrates control-type stratification, intervention-type subgrouping, and sensitivity analysis by risk of bias, comprehensive risk of bias assessment using RoB 2. The review also adheres to PRISMA 2020 standards and includes studies from diverse clinical settings and populations. Nonetheless, there are several limitations to this study. The number of included studies remains small, which limits statistical power and generalizability. Considerable heterogeneity was present (I² > 90%), even within subgroup analyses, suggesting unmeasured moderators such as therapist training, fidelity, participant engagement, or cultural adaptation may influence outcomes. Additionally, few studies reported long-term follow-up data, which restricts insights into the durability of effects. Finally, variability in outcome measurement tools (e.g., GAF, PSP, SLOF) complicates direct comparisons across studies, though this is common in psychosocial literature.
Conclusion
This review shows that psychosocial interventions produce moderate, significant improvements in social functioning among individuals with severe mental illness. Mindfulness-based and face-to-face modalities yield important effects. Our findings reinforce the importance of early, structured psychosocial strategies in promoting functional recovery, particularly where pharmacological treatment alone is insufficient. The results highlight the impact of intervention quality and study design, as higher methodological rigor influenced effect estimates. Despite substantial heterogeneity, sensitivity analyses confirmed the robustness of the findings. These insights support the consensus that functional outcomes like social integration and interpersonal competence are core targets in managing schizophrenia and related disorders. Future research should prioritize high-quality longitudinal trials with standardized measures to optimize implementation and achieve meaningful recovery beyond symptom reduction.
References
- McNally RJ. What is mental illness? Harvard University Press (2012).
- Knapp M, Wong G. Economics and mental health: the current scenario. World Psychiatry 19 (2020): 3-14.
- Thornicroft G. European mental health policy: the key issue is social inclusion. The European Journal of Public Health 21 (2011): 548-549.
- Killaspy H, Harvey C, Brasier C, et al. Community-based social interventions for people with severe mental illness: a systematic review and narrative synthesis of recent evidence. World Psychiatry 21 (2022): 96-123.
- Gonzales L, Kois LE, Chen C, et al. Reliability of the term “serious mental illness”: A systematic review. Psychiatric services 73 (2022): 1255-1262.
- Schinnar AP, Rothbard AB, Kanter R, et al. An empirical literature review of definitions of severe and persistent mental illness. The American journal of psychiatry. Published Online First (1990).
- Brissos S, Balanzá-Martinez V, Dias VV, et al. Is personal and social functioning associated with subjective quality of life in schizophrenia patients living in the community? Eur Arch Psychiatry Clin Neurosci 261 (2011): 509-517.
- Bjornestad J, Hegelstad WTV, Berg H, et al. Social Media and Social Functioning in Psychosis: A Systematic Review. J Med Internet Res 21 (2019): e13957.
- Stanislaus S, Faurholt-Jepsen M, Vinberg M, et al. Mood instability in patients with newly diagnosed bipolar disorder, unaffected relatives, and healthy control individuals measured daily using smartphones. J Affect Disord 271 (2020): 336-344.
- Gershon A, Eidelman P. Inter-episode affective intensity and instability: predictors of depression and functional impairment in bipolar disorder. Journal of Behavior Therapy and Experimental Psychiatry 46 (2015): 14-18.
- Hofmann SG, Doan SN. Introduction. In: The social foundations of emotion: Developmental, cultural, and clinical dimensions. American Psychological Association: Washington (2018): 3-9.
- Van Rheenen TE, Rossell SL. Objective and subjective psychosocial functioning in bipolar disorder: an investigation of the relative importance of neurocognition, social cognition and emotion regulation. Journal of Affective Disorders 162 (2014): 134-141.
- Van Rheenen TE, Rossell SL. Phenomenological predictors of psychosocial function in bipolar disorder: is there evidence that social cognitive and emotion regulation abnormalities contribute? Australian & New Zealand Journal of Psychiatry 48 (2014): 26-35.
- Bighelli I, Rodolico A, García-Mieres H, et al. Psychosocial and psychological interventions for relapse prevention in schizophrenia: a systematic review and network meta-analysis. The Lancet Psychiatry 8 (2021): 969-980.
- Marshall M, Lockwood A, Cochrane Schizophrenia Group. Assertive community treatment for people with severe mental disorders. Cochrane database of systematic reviews (2010).
- Marshall M, Gray A, Lockwood A, et al. Case management for people with severe mental disorders. Cochrane Database of Systematic Reviews (2010).
- Keyes CL, Dhingra SS, Simoes EJ. Change in level of positive mental health as a predictor of future risk of mental illness. American journal of public health 100 (2010): 2366-2371.
- Wood AM, Joseph S. The absence of positive psychological (eudemonic) well-being as a risk factor for depression: A ten-year cohort study. Journal of Affective Disorders 122 (2010): 213-217.
- Iasiello M, van Agteren J, Keyes CL, et al. Positive mental health as a predictor of recovery from mental illness. Journal of Affective Disorders 251 (2019): 227-230.
- Schotanus-Dijkstra M, Keyes CL, de Graaf R, et al. Recovery from mood and anxiety disorders: The influence of positive mental health. Journal of Affective Disorders 252 (2019): 107-113.
- Iasiello M, Van Agteren J. Mental health and/or mental illness: A scoping review of the evidence and implications of the dual-continua model of mental health. Evidence Base: A journal of evidence reviews in key policy areas (2020): 1-45.
- Van Agteren J, Iasiello M, Lo L, et al. A systematic review and meta-analysis of psychological interventions to improve mental wellbeing. Nature and human behaviour 5 (2021): 631-652.
- Li J, Huang Y-G, Ran M-S, et al. Community-based comprehensive intervention for people with schizophrenia in Guangzhou, China: Effects on clinical symptoms, social functioning, internalized stigma and discrimination. Asian Journal of Psychiatry 34 (2018): 21-30.
- Chien WT, Cheng HY, McMaster TW, et al. Effectiveness of a mindfulness-based psychoeducation group programme for early-stage schizophrenia: An 18-month randomised controlled trial. Schizophrenia Research 212 (2019): 140-149.
- Dubreucq J, Gabayet F, Ycart B, et al. Improving social function with real-world social-cognitive remediation in schizophrenia: Results from the RemedRugby quasi-experimental trial. European Psychiatry 63 (2020): 41.
- Dark F, Scott JG, Baker A, et al. Randomized controlled trial of social cognition and interaction training compared to befriending group. Br J Clin Psychol 59 (2020): 384-402.
- Berry C, Hodgekins J, French P, et al. Clinical and cost-effectiveness of social recovery therapy for the prevention and treatment of long-term social disability among young people with emerging severe mental illness (PRODIGY): randomised controlled trial. Br J Psychiatry 220 (2022): 154-162.
- O’Sullivan S, Schmaal L, D’Alfonso S, et al. Characterizing Use of a Multicomponent Digital Intervention to Predict Treatment Outcomes in First-Episode Psychosis: Cluster Analysis. JMIR Mental Health 9 (2022).
- Han M, Lee K, Kim M, et al. Effects of a Metacognitive Smartphone Intervention with Weekly Mentoring Sessions for Individuals With Schizophrenia: A Quasi-Experimental Study. J Psychosoc Nurs Ment Health Serv 61 (2023): 27-37.
- Silva MJD, Cooper S, Li HL, et al. Effect of psychosocial interventions on social functioning in depression and schizophrenia: meta-analysis. The British Journal of Psychiatry 202 (2013): 253-260.
- Li Z, Arthur D. Family education for people with schizophrenia in Beijing, China: randomised controlled trial. The British Journal of Psychiatry 187 (2005): 339-345.
- Pang Y. The effect of health education on compliance of patients with paranoid schizophrenia in their follow-up therapy. Chinese Mental Health Journal 16 (2002): 348-350.
- Sawyer C, McKeon G, Hassan L, et al. Digital health behaviour change interventions in severe mental illness: a systematic review. Psychological medicine 53 (2023): 6965-7005.
- Aschbrenner KA, Naslund JA, Shevenell M, et al. A pilot study of a peer-group lifestyle intervention enhanced with mHealth technology and social media for adults with serious mental illness. The Journal of nervous and mental disease 204 (2016): 483-486.
- Campos C, Mesquita F, Marques A, et al. Feasibility and acceptability of an exergame intervention for schizophrenia. Psychology of Sport and Exercise 19 (2015): 50-58.
- Olmos-Ochoa TT, Niv N, Hellemann G, et al. Barriers to participation in web-based and in-person weight management interventions for serious mental illness. Psychiatric rehabilitation journal 42 (2019): 220.
- Khoury B, Lecomte T, Gaudiano BA, et al. Mindfulness interventions for psychosis: a meta-analysis. Schizophrenia research 150 (2013): 176-184.
- Aust J, Bradshaw T. Mindfulness interventions for psychosis: a systematic review of the literature. Journal of psychiatric and mental health nursing 24 (2017): 69-83.
- Khoury B, Lecomte T, Fortin G, et al. Mindfulness-based therapy: a comprehensive meta-analysis. Clinical psychology review 33 (2013): 763-771.
- Cella M, Preti A, Edwards C, et al. Cognitive remediation for negative symptoms of schizophrenia: a network meta-analysis. Clinical psychology review 52 (2017): 43-51.
- Revell ER, Neill JC, Harte M, et al. A systematic review and meta-analysis of cognitive remediation in early schizophrenia. Schizophrenia research 168 (2015): 213-222.
- Tran T, Spilka MJ, Raugh IM, et al. Negative symptom trajectories in individuals at clinical high risk for psychosis: differences based on deficit syndrome, persistence, and transition status. Schizophrenia Bulletin open 4 (2023): 014.
- Devoe DJ, Liu L, Braun A, et al. Cognitive-Behavioural Social Skills Training: Mediation of Treatment Outcomes in a Randomized Controlled Trial for Youth at Risk of Psychosis: L’entraînement aux compétences sociales cognitivo-comportementales: variables médiatrices des résultats thérapeutiques dans le cadre d’un essai clinique randomisé pour les jeunes présentant un risque de psychose. Can J Psychiatry 70 (2025): 217-228.
- Cuijpers P, van Straten A, Bohlmeijer E, et al. The effects of psychotherapy for adult depression are overestimated: a meta-analysis of study quality and effect size. Psychological medicine 40 (2010): 211-223.
- Higgins JP, Altman DG, Gøtzsche PC, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. Bmj 343 (2011).
Journals List
© 2016-2025, Copyrights Fortune Journals. All Rights Reserved