Prognostic of Sepsis in a Congolese Pediatric Emergency Service Using PSOFA Score: A Prospective Study
Article Information
Jacques Balekelayi wa Balekelayi1*, Valérie Bolingo Bola2, Stéphanie Mikalo Mbambi3, Joseph Mabiala Bodi1, Victoire Audray Bikoumou4, Ariane Mankiele Keto1, Mamy-gloire Manzi Monkoti1, Thideline Mankanga Mabela1, Agathe Maku Fwani1, Karem Efombola Itokua1, Jennifer Misengabu Lembalemba1, Célestin Ndosimao Nsibu1
1Department of Pediatrics, University Clinics of Kinshasa, Kinshasa, Democratic Republic of Congo
2Department of Pediatrics, Saint Joseph Hospital, Hospital in Kinshasa, Democratic Republic of the Congo
3Faculty of Medicine, Protestant University of Congo, University in Kinshasa, Democratic Republic of the Congo
4Department of Radiology and Medical Imaging, University Clinics of Kinshasa, Hospital in Kinshasa, Democratic Republic of the Congo
*Corresponding Author: Jacques Balekelayi wa Balekelayi, Department of Pediatrics, University Clinics of Kinshasa, Kinshasa, Democratic Republic of Congo.
Received: 28 May 2023; Accepted: 24 August 2023; Published: 12 September 2023
Citation:
Jacques Balekelayi wa Balekelayi, Valérie Bolingo Bola, Stéphanie Mikalo Mbambi, Joseph Mabiala Bodi, Victoire Audray Bikoumou, Ariane Mankiele Keto, Mamy-gloire Manzi Monkoti, Thideline Mankanga Mabela, Agathe Maku Fwani, Karem Efombola Itokua, Jennifer Misengabu Lembalemba, Célestin Ndosimao Nsibu. Prognostic of Sepsis in a Congolese Pediatric Emergency Service Using PSofa Score: A Prospective Study. Journal of Pediatrics, Perinatology and Child Health. 7 (2023): 184-189.
View / Download Pdf Share at FacebookAbstract
Background: The pediatric emergency service represents a very important link in the care of sick children and children with serious medical conditions, such as sepsis. In the Democratic Republic of Congo (DRC), mortality from sepsis in children is still very high and no study has analyzed the influence of the pSOFA score on vital prognosis in the emergency service.
Methodology: Prospective observational cross-sectional study from April 1 to September 30, 2022. We included all children aged 1 to 15 suspected of sepsis according to SIRS criteria in the Emergency Room of Pediatrics at Saint-Joseph Hospital in Kinshasa, Democratic Republic of Congo. The pSOFA score was calculated for all patients within 24 hours after infection was first suspected in the emergency department and was correlated with their evolution within 7 days. The usual statistics were used.
Results: Of 92 patients collected in the study, 10 patients had died within 7 days of suspicion of sepsis, including 9 with a pSOFA score ≥ 2 and 1 with a pSOFA score < 2. Respiratory distress, coma, convulsions, oliguria, shock and hypothermia were significantly found in patients with a pSOFA score ≥ 2. In univariate analysis, we noted that the pSOFA score ≥2 and the admission time ≥ 6 days were significantly associated with mortality within 7 days with a risk multiplied by 18 and 9 respectively.
Conclusion: Beyond diagnosing sepsis, the pSOFA score may be a good predictor of its mortality.
Keywords
Sepsis; Pediatric Emergency; DRC
Sepsis articles; Pediatric Emergency articles; DRC articles
Article Details
1. Introduction
1.1 Sepsis and Pediatric Emergency Room
The reception room for pediatric emergencies represents a very important link in the care of sick children and it has a very high attendance rate [1]. Pediatric emergencies constitute all the morbid states which, in a more or less short term, threaten the life of the child and require rapid and adequate care [2]. Medical personnel performing emergency department triage may encounter serious medical conditions in the patient, such as sepsis. It corresponds to the suspected or proven presence of an infection accompanied by systemic manifestations of the body [3]. Sepsis is one of the oldest and most elusive syndromes in medicine [4].
However, sepsis is difficult to identify and distinguish from other pathologies. It represents a major adversary [5], since its clinical manifestations are very variable. They depend on several factors such as the site of initial infection, the causative organism and the patient's underlying health condition [4]. In addition, the clinical signs of a septic syndrome are frequently confused with other non-infectious causes. The uncertainty caused by these confusing similarities can lead to a delay in diagnosis and treatment, thus causing a rapid deterioration in the patient's state of health that can lead to death [6]. Around the world, about 6 million children die of sepsis every year. A recent study published in England finds that 15% of child deaths are due to infection and that of severe sepsis in children has increased from 0.56 to 0.89 cases per 1000 children, in all age groups. In low-resource countries, septic states are just as burdened with heavy morbidity and mortality. In 2015, infectious diseases were the cause of more than 50% of deaths of children under five, particularly in South Asia and sub-Saharan Africa [7]. Mortality related to sepsis in the emergency room is high: it is 26.1% in the pediatric department of the C.H.U Gabriel TOURE in Mali [2]. A study carried out in Senegal in 2005 concerning the epidemiological, bacteriological and evolutionary profile of pediatric sepsis recorded a lethality of 15.6% [8].
1.2 pSOFA score and prognosis
In May 2017, the United Nations World Health Assembly and the World Health Organization adopted as a global health priority the need to improve the recognition, management and prevention of sepsis and, among other key points, recognized the heavy toll of sepsis on children's health [9,10]. Globally, professional medical societies and sepsis advocacy organizations have played an important role in developing innovative approaches to improve sepsis care for adults and children [11]. A current study has developed a pediatric version of SOFA called pSOFA by including age-adjusted cutoffs for cardiovascular and renal variables and adding the PaO2/FiO2 or SpO2/FiO2 ratio as a noninvasive surrogate for lung injury. Like the SOFA, the total pSOFA score varies between 0 and 24 [12]. Since then, several studies around the world have attempted to adapt the SOFA score to pediatric patients (pSOFA) to measure the extent of pediatric sepsis and to assess its prognostic accuracy relative to other organ dysfunction scores. In the USA in 2017, a study conducted on the adaptation and validation of the pSOFA score in sick children found that this score had excellent discrimination in in-hospital mortality [12]. In Australia (2018), the study investigating the relationship between mortality and sepsis definition score in 2594 patients admitted to pediatrics with infection showed that an increase of ≥ 2 points in the individual score was associated with a gross increase mortality from 3.1 to 6.8% for SIRS and from 1.9 to 7.6% for age-appropriate SOFA (pSOFA) [13]. In Saudi Arabia, the study by Mohamed O. et al. in 2021 on the epidemiology of pediatric sepsis in the pediatric intensive care unit found that an increase in pSOFA score > 4 was significantly associated with increased mortality, with calculated ORs of 3.6 (95% CI: 1.30–9.93; p = 0.013) [14].
1.3 Rationale for the study
In Africa [15] and specifically in the Democratic Republic of Congo (DRC) [16,17], mortality from sepsis in children is still very high and no study has analyzed the influence of the pSOFA score on vital prognosis in the emergency room.
This work will identify the prognostic aspects of sepsis in a pediatric emergency in the DRC. The aim of the study is to contribute to the improvement of the management of infantile sepsis in order to reduce its mortality in our country.
|
Neurological: Glasgow Score |
15 |
13-14 |
45270 |
45175 |
<6 |
|
Respiratory: |
|||||
|
PaO2/FiO2 or |
≥400 |
300-399 |
200-299 |
100-199 |
<100 |
|
SpO2/FiO2 |
≥292 |
264-291 |
221-264 |
148-220 |
<148 |
|
Hemodynamics |
|||||
|
PAM in mmHg |
|||||
|
<1month |
≥46 |
<46 |
Drugs in μg/Kg/min: Dopamine ≤ 5 or Dobutamine |
Drugs in μg/Kg/min: |
Drugs in μg/Kg/min: |
|
[1 month – 1 year] |
≥55 |
<55 |
Dopamine 5-15 or Noradré* ≤0.1 or Adré** ≤ 0.1 |
Dopamine >15 or Noradré* >0.1 or Adré** >0.1 |
|
|
[1 year – 2 years] |
≥60 |
<60 |
|||
|
[2 years – 5 years] |
≥62 |
<62 |
|||
|
[5 years – 12 years] |
≥65 |
<65 |
|||
|
[12 years-18 years] |
≥67 |
<67 |
|||
|
≥ 18 years old |
≥70 |
<70 |
|||
|
Coagulation: Platelets/μL |
≥ 150 000 |
100 000-149000 |
50 000-99 000 |
20 000-49 000 |
<20 000 |
|
Hepatic: Bilirubin mg/dL |
<1.2 |
1.2-1.9 |
2.0-5.9 |
6.0-11.9 |
>12.0 |
|
Renal: Creatinine mg/l |
|||||
|
<1 month |
<8 |
8-9 |
10-11 |
12-15 |
³16 |
|
[1 month – 1 year] |
<3 |
3-4 |
5-7 |
8-11 |
³12 |
|
[1 year – 2 years] |
<4 |
4-5 |
6-10 |
11-14 |
³15 |
|
[2 years – 5 years] |
<6 |
6-8 |
9-15 |
16-12 |
³23 |
|
[5 years – 12 years |
<7 |
7-10 |
11-17 |
18-25 |
³26 |
|
[12 years – 18 years] |
<10 |
10-16 |
17-28 |
29-41 |
³42 |
|
£ 18 years old |
<12 |
12-19 |
20-34 |
35-49 |
³50 |
|
*: Noradrenaline **: Adrenaline |
|||||
Table 1: Paediatric sequential sepsis-related organ failure assessment (pSOFA) score translated and adapted [18].
2. Methods
2.1 Study design and participants
This study was carried out in the pediatric Emergency Service of Saint-Joseph Hospital in Kinshasa, Democratic Republic of Congo. This was a prospective observational cross-sectional study, over a period of six months, from April 1 to September 30, 2022. We included all children aged 1 to 15 suspected of sepsis according to the SIRS criteria and those whose parents had consented to have their child participate. Excluded were children whom we were unable to follow for a week (transferred outside the hospital, discharged against medical advice, etc.). The primary endpoint was mortality at 7 days from the date of onset of sepsis. The secondary endpoints were the prognosis of sepsis (pSOFA score) and the clinical condition on admission. In this study, the prognosis of sepsis was assessed using the Sepsis-3 definition. Sepsis-3 defines sepsis as life-threatening organ dysfunction due to a dysregulated host response to infection using the Pediatric Sequential Organ Assessment (pSOFA) score. This score evaluates six organ systems: respiratory, hematological, hepatic, cardiovascular, neurological and renal. A sub-score of 0 to 4 points is calculated for each component (Table1). The pSOFA score was calculated for all patients within 24 h after infection was first suspected in the emergency room and was correlated with their evolution within 7 days.
2.2 Data collection and analysis
The variables studied were: age, gender, clinical signs on admission, clinical and paraclinical parameters defining the sepsis (SIRS and pSOFA), future of the child within 7 days. The data collected on the medical files were first reported on the collection sheets and then recorded on an Excel sheet to constitute the database.
The database created using Excel software was then transcoded using SPSS for Windows software version 26.00 (IBM Corp., Armonk, NY, USA) for statistical analysis. Descriptive statistics were used. Pearson's Chi-Square or Fischer's Exact test was used for comparison of proportions, Student's T test for comparison of means and the non-parametric Mann-Whitney test for comparison of medians. The odds ratio (odds ratio: OR) with their 95% confidence intervals were used as a measure of association between the value of the pSOFA score (<2 or ≥2 points) and the vital outcome within 7 days. This ratio was considered significant if its 95% confidence interval (95% CI) does not contain the value 1, otherwise it is considered insignificant. For all tests, the p value < 0.05 was the statistical significance level.
2.3 Ethical considerations
The protocol for this work was submitted to the biomedical research ethics committee of the School of Public Health and obtained its approval under number ESP/CE/38/2023. This work was carried out in strict compliance with the fundamental principles of ethics. Informed consent was sought from the parents or carers of the patients, first verbally and then in writing using a form.
3. Results
During our study, we were able to collect 92 patients fulfilling the inclusion criteria. The average age of our study population was 5.9 years. The age group under 5 years predominated at 52%. Boys (53.3%) outnumbered girls (46.7%) (Table 2). A total of 10 patients, or 10.9%, died within 7 days of suspicion of sepsis, including 9 with a pSOFA score greater than or equal to 2 points and 1 with a pSOFA score less than 2 points (Figure 1); this difference was statistically significant (p<0.001) (Table 2). Respiratory distress, coma, convulsions, oliguria, shock and hypothermia were significantly found in patients with a pSOFA score ≥ 2 points (p<0.05). Regarding biology, we noted that the hemoglobin and hematocrit levels were significantly low, that of blood creatinine and bilirubin was significantly high in these patients (pSOFA score ≥ 2 points), (p<0.05) (Table 3). The majority of deceased patients had a pSOFA score greater than or equal to 2 points, an admission delay greater than or equal to 6 days and a hospital stay less than 7 days with a statistically significant difference (p<0.05). In univariate analysis, we noted that the pSOFA score ≥2 and the admission time ≥ 6 days were significantly associated with mortality within 7 days with a risk multiplied by 18 respectively [OR=18.3; 95% CI (1.4-95); p=0.006] and 9 [OR=9; 95% CI (1.1-74.3); p=0.016] (Table 2).
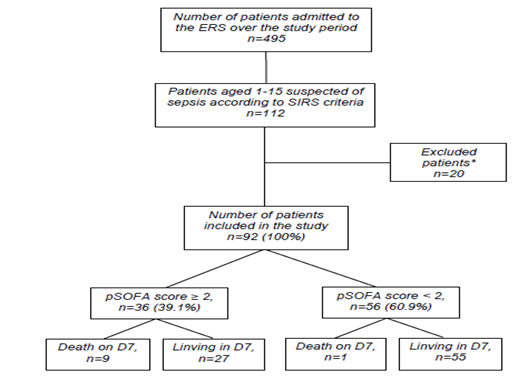
Figure 1: Flow diagram, ERS: emergency reception service; pSOFA: Sequential sepsis-related organ failure assessment pediatric; *: refusal of consent (n=8), inability to follow up until D7 (n=12).
|
Global Population (n=92) |
Died at 7 days (n=10) |
Alivr at 7 days (n=82) |
OR [IC95%] |
p-value |
|
|
Middle age (years) |
5.9 |
4.1 |
6.2 |
0.178 |
|
|
Age groups (year) |
0.196 |
||||
|
<5 |
48(52.2) |
7(70) |
41(50) |
1 |
|
|
≥5 |
44(47.8) |
3(30) |
41(50) |
0.4[0.1-1.7] |
|
|
Sex |
0.456 |
||||
|
Girls |
43(46.7) |
4(40) |
39(47.6) |
1 |
|
|
Boys |
49(53.3) |
6(60) |
43(52.4) |
1.3[0.3-5.1] |
|
|
pSOFA score |
<0.001 |
||||
|
<2 |
56(60.9) |
1(10) |
55(65.8) |
1 |
|
|
≥2 |
36(39.1) |
9(90) |
27(34.2) |
18.3[1.4-95] |
|
|
Admission deadlines mean |
6 |
12.1 |
6.7 |
<0.001 |
|
|
Admission deadlines |
0.016 |
||||
|
<6days |
42(45.7) |
1(10) |
41(50) |
1 |
|
|
≥6days |
50(54.3) |
9(90) |
41(50) |
9[1.1-74.3] |
Table 2: General characteristics of the study population according to vital outcome at 7 days of follow-up.
|
Global Population (n=92) |
pSOFA ≥ 2 points (n=36) |
pSOFA < 2 points (n=56) |
p-value |
|
|
Clinical signs at ERS |
||||
|
Fever |
90(97.8) |
34(94.4) |
56(100) |
0.237 |
|
physical asthenia |
56(60.8) |
16(44,4) |
40(71.4) |
0.838 |
|
Hepatomegaly |
32 (34.8) |
16(44.4) |
16(28.6) |
0.119 |
|
Respiratory distress |
25(27.2) |
14(38.9) |
11(19.6) |
0.043 |
|
Coma |
25(27.2) |
20(55.5) |
5(8.9) |
<0.001 |
|
Jaundice |
17(18.5) |
10(27.8) |
7(12.5) |
0.065 |
|
Splenomegaly |
17(18.5) |
8(22.2) |
9(16.1) |
0.458 |
|
Convulsion |
16(17.4) |
12(33.3) |
4(7.1) |
0.001 |
|
Oliguria |
8(8.7) |
8(22,2) |
0(0) |
<0.001 |
|
Shock |
5(5.4) |
5(13,6) |
0(0) |
0.028 |
|
Urine coca cola |
4(4.3) |
2(5.5) |
2(3.6) |
0.649 |
|
Hypothermia |
2(2.2) |
2(5.5) |
0 |
<0.001 |
|
Bleeding |
2(2.2) |
1(2.7) |
1(1.7) |
0.75 |
|
Standard biology at ERS* |
||||
|
Haemoglobin (g/dl) |
8.9 |
8.3 |
9.3 |
0.043 |
|
Haematocrit (%) |
26.7 |
25 |
28 |
0.043 |
|
White blood cells (/mm3) |
15030 |
16350 |
14000 |
0.363 |
|
Platelets (/μL) |
178000 |
162000 |
179000 |
0.513 |
|
CRP (mg/dL) |
74.8 |
98 |
54.5 |
0.289 |
|
Creatinine (mg/L) |
8 |
10 |
8 |
<0.001 |
|
Total bilirubin (mg/dL) |
0.8 |
0.9 |
0.7 |
0.002 |
|
Died at 7 days |
10(10.9) |
8(80) |
2(20) |
0.005 |
Table 3: Characteristics of patients according to the value of the pSOFA score (greater or less than 2 points) collected in the emergency room.
4. Discussion
This prospective study underlines the relevance of using the pSOFA score upon admission to the pediatric Emergency Reception Service (ERS) to predict 7-day mortality in our hospital setting in the DR Congo.
In our study we found that 10.9% of patients died within 7 days. 89.1% of patients survived. Most of the deaths within 7 days, i.e. 90%, occurred in patients with sepsis according to pSOFA with a statistically significant difference (P<0.001). The reported pediatric sepsis mortality rate varies widely between studies, particularly between developed and developing countries. In Saudi Arabia in 2021, Mohamed et al. [14] noted in his study that the mortality rate was 10% at 7 days and 23.89% at 28 days. In Egypt, the sepsis mortality rate within 28 days was reported at 28.1 and 8.8% by Bekhit et al. and El-Mashad et al., respectively [19,20]. A study by the Italian Pediatric Sepsis Study Group in Italian PICUs reported a 28-day mortality rate of 17.8% for severe sepsis [21]. Xiao et al. conducted an epidemiological study in major PICU centers in southwest China, reporting a severe sepsis mortality rate of 18.8% at 28 days [22]. Unlike other studies mostly carried out in pediatric intensive care units, our study was limited to evaluating mortality within 7 days being carried out in an emergency department.
In our study we noted that the majority of deaths (90%) occurred in patients with a pSOFA score greater than or equal to 2 points. Thus, the pSOFA score ≥ 2 multiplied the risk of death by 18 associated with a delay in admission ≥ 6 days which multiplied this risk by 9. Our result is consistent with data from the literature. In Saudi Arabia, Mohamed et al. [14] had in his study noted that an increase in the pSOFA score > 4 was significantly associated with increased mortality, with calculated ORs of 3.6 (95% CI: 1.30–9.93; p = 0.013 ). As in other studies, an increase in pSOFA score > 4 points was independently associated with an increased risk of mortality. This indicates that a higher pSOFA score suggests increased organ dysfunction and thus a pSOFA score may be a useful predictor of mortality [12,23]. Therefore, Ouissal et al. [18] in a recent editorial of the Panafrican Medical Journal in 2021 proposed for low-resource countries that any child with a pediatric SOFA score ≥ 2 should be referred to pediatric intensive care and that the initial management of the child with sepsis should come from the recommendations of the sepsis survival campaign devoted to children and published in February 2020 [24].
5. Conclusion
Sepsis is a serious and deadly pathology in the pediatric emergency room of Saint-Joseph hospital in Kinshasa. The pSOFA score greater than or equal to two points multiplied the risk of death by twelve compared to the admission delay greater than or equal to six days which multiplied it by five. Indeed, quickly diagnosing infected patients at risk of getting worse improves the vital prognosis of patients [26]. Beyond diagnosing sepsis, the pSOFA score may be a good predictor of its mortality.
Limits of the study
The study was limited by its monocentric nature and the relatively small number of patients. The implementation of a national database will help to conduct large-scale studies in order to obtain more conclusive results, formulate recommendations, and, consequently, improve the results of pediatric sepsis in our country.
Declaration of conflicts of interest
The authors declare that they have no conflict of interest in relation to this manuscript.
Contribution of each author
Design, data collection, interpretation of results, manuscript writing: J Balekelayi; Manuscript design, writing, supervision and proofreading: J Bodi; interpretation of results, reading, correction and revision of the article: C Nsibu, V Bikoumou, A Keto, M Monkoti, T Mabela, A Fwani, J Lembalemba, V Bola. All authors have read and approved the final version of the manuscript.
References
- Dembélé A, Cissé ME, Diakité AA, et al. Epidemio-clinical study of referrals to pediatric emergencies at the C.H.U Gabriel Touré. MALI PUBLIC HEALTH (2020): 29-33.
- Abdou RO. Pediatric emergencies at the hospital center of Libreville. Black African Medicine 49 (2002): 475-480.
- Dellinger RP, Levy MM, Rhodes A, et al. Surviving Sepsis” campaign: International guide for the management of severe sepsis and septic shock. Critical Care Medicine 41 (2013): 580-637.
- Angus D, Van der Poll T. Severe sepsis and septic shock. The New England journal of medicine 369 (2013): 840-851.
- Poeze M, Ramsay G, Gerlach H, et al. An international sepsis survey: A study of doctors’ knowledge and perception about sepsis. Critical Care Medecine 8 (2004): 409-413.
- Tang B, Eslick GD, Craig JC, et al. Accuracy of procalcitonin for sepsis diagnosis in critically ill patients: Systematic review and meta-analysis. The lancet infectious disease 7(2007): 210-217.
- Singer M, Deutschman CS, Seymour CW et al. The third International consensus definitions for sepsis and septic shock (Sepsis-3). JAMA 2016; 315 (8):801–810.
- Mousavi SA, Mouvavi SJ. Surgical site infection in children a single center study. Research J Bio Sciences 3 (2008): 880-883.
- 70th World Health Assembly. Improve the prevention, diagnosis and clinical management of sepsis (2017). Available at: http://apps.who.int/gb/ebwha/pdf_files/WHA70/A70_R7-en.pdf?ua=1. Accessed January 24, 2019.
- Kissoon N, Reinhart K, Daniels R, et al. Sepsis in children: global implications of the World Health Assembly resolution on sepsis. Pediatrician Crit Care Med 18 (2017): e625-e627.
- Society of Critical Care Medicine. Survive Sepsis Campaign (2019). Available at: www.survivingsepsis.org/Pages/default.aspx. Accessed April 1, 2019.
- Matics TJ, Sanchez-Pinto LN. Adaptation and validation of a pediatric sequential organ failure assessment score and assessment of Sepsis-3 definitions in critically ill children. JAMA Pediatrician 171 (2017): e172352.
- Luregn J, Lahn S, Rinaldo B, et al. Prognostic accuracy of age-adapted SOFA, SIRS, PELOD-2 and qSOFA for in-hospital mortality among children with suspected infection admitted to the intensive care unit. Intensive Care Med 44 (2018): 179-188.
- Mohamed O, Mona A, Maher M. et al. Épidémiologie du sepsis pédiatrique dans l'unité de soins intensifs pédiatriques de la ville médicale du roi Abdulaziz, Djeddah. National library of Medecine (2021).
- Weiss S, Fitzgerald JC, Pappachan J, et al. Prévalence du sepsis, résultats et thérapies (SPROUT) Study Investigators and Pediatric Acute Lung Injury and Sepsis Investigators (PALISI) Network Épidémiologie mondiale du sepsis pédiatrique grave : étude sur la prévalence, les résultats et les thérapies du sepsis. Suis J Respir Crit Care Med 191 (2015): 1147-1157.
- Kambale M, Kasengi JB, Kivukuto JM, et al. Profil infectieux et mortalité des enfants âgés de 0 à 5 ans admis pour malnutrition aigue sévère: étude de cohorte rétrospective au Centre Nutritionnel et Thérapeutique de BUKAVU, RDC. The Pan African Médical Journal 23 (2016).
- Monkoti M. Co-infection sepsis et paludisme grave. Mémoire de spécialisation en pédiatrie. Faculté de Médecine, UNIKIN (2014) : 1-34.
- Ouissal Aissaoui, El-bouz M, Aziz Bousfiha Aet al. Sepsis chez l’enfant : protocole d’orientation rapide vers la réanimation pédiatrique. PAMJ 39 (2021): 1-4.
- Bekhit Oel S, Algameel AA, Eldash HH. Application de l'indice de mortalité pédiatrique version 2 : score en unité de soins intensifs pédiatriques dans un pays africain en développement. Pan Afrique Med J 17 (2014): 185.
- Mohamed El-Mashad G, Said El-Mekkawy M, Helmy Zayan M. Score d'évaluation séquentielle des défaillances d'organes (pSOFA) pédiatrique : un nouveau score de prédiction de la mortalité dans l'unité de soins intensifs pédiatriques. An Pédiatre (Barc) 92 (2020): 277-285.
- Wolfler A, Silvani P, Musicco M, et al. Étude italienne sur le sepsis pédiatrique g : incidence et mortalité dues au sepsis, au sepsis sévère et au choc septique dans les unités de soins intensifs pédiatriques italiennes : une enquête nationale prospective. Méd. de soins intensifs 34 (2008): 1690-1697.
- Xiao C, Wang S, Fang F, et al. Épidémiologie du sepsis pédiatrique sévère dans les principaux centres de soins intensifs du sud-ouest de la Chine. Pédiatre Crit Care Med 20 (2019): 1118-1125.
- Lalitha A, Satish J, Reddy M, et al. Le score d'évaluation séquentielle des défaillances organiques (SOFA) en tant que prédicteur de l'issue du sepsis en unité de soins intensifs pédiatriques. J Pediatr Soins Intensifs 10 (2021): 110-117.
- Weiss SL, Peters MJ, Alhazzani W, et al. Surviving sepsis campaign international guidelines for the management of septic shock and sepsis associated organ dysfunction in children. Pediatr Crit Care Med 21 (2020): e52-e106.
