Prognostic Factors Trauma and Epidemiologic Related in Surgically Treated Extradural Hematoma
Article Information
Leandro Pelegrini de Almeida*, Mateus Carvalho Casarin, Luiz Pedro Williman Rogério, Guilherme Finger, Samir Cezimbra dos Santos, Felipe Lourenzon Schiavo
Department of Neurosurgery, Cristo Redentor Hospital, Porto Alegre, Brazil
*Corresponding Author: Leandro Pelegrini de Almeida, Department of Neurosurgery, Cristo Redentor Hospital, Rio Grande do Sul, Porto Alegre, Brazil
Received: 26 July 2019; Accepted: 09 August 2019; Published: 14 August 2019
Citation: Leandro Pelegrini de Almeida, Mateus Carvalho Casarin, Luiz Pedro Williman Rogério, Guilherme Finger, Samir Cezimbra dos Santos, Felipe Lourenzon Schiavo. Prognostic Factors Trauma and Epidemiologic Related in Surgically Treated Extradural Hematoma. Journal of Surgery and Research 2 (2019): 105-115.
View / Download Pdf Share at FacebookAbstract
Background: Extradural hematoma (EDH) represents an important intracranial lesion in patients with traumatic brain injury, since the mortality rate can be high. The outcome from surgical treatment is directly related to patient’s preoperative neurological condition, but there is no specific trauma and epidemiologic prognostic factors that contribute to analyze the patient’s follow-up.
Objective: Establish prognostics factors based on the characteristics of the trauma that can contribute to the management.
Methods: Retrospective study performed from January 2005 to January 2016. The inclusion criteria were patients with EDH surgically treated. The exclusion criteria were patients with other types of traumatic brain lesions also with criteria for surgery. Data about the neurological status (GCS), epidemiological and radiological analysis were compared to post-surgical outcome follow-up.
Results: The sample was composed of 250 patients, commonly males (84.8%) and aged between 10 and 19 years. Motorcycle and car accidents were associated with worst GCS (p=0.001) and outcome (p=0.002). Frontal location was correlated with better GCS and parietal with worst (p=0.0024). GCS was directly correlated with hospitalization time (p=0.003) and outcome (p<0.001). Female subgroup presented better outcome (p=0.019).
Conclusion: Prognostic conditions must be considered to allow physicians and their team to be prepared to special care and to give better prognostic information to the patient’s relatives. Patients affected by motorcycle and car accidents, with parietal EDH tend to have a worse neurological condition than female patients, with frontal location. Th
Keywords
Brain trauma, Extradural hematoma, Prognostic factors, Trauma epidemiology
Brain trauma articles, Extradural hematoma articles, Prognostic factors articles, Trauma epidemiology articles
Extradural hematoma articles Extradural hematoma Research articles Extradural hematoma review articles Extradural hematoma PubMed articles Extradural hematoma PubMed Central articles Extradural hematoma 2023 articles Extradural hematoma 2024 articles Extradural hematoma Scopus articles Extradural hematoma impact factor journals Extradural hematoma Scopus journals Extradural hematoma PubMed journals Extradural hematoma medical journals Extradural hematoma free journals Extradural hematoma best journals Extradural hematoma top journals Extradural hematoma free medical journals Extradural hematoma famous journals Extradural hematoma Google Scholar indexed journals Brain trauma articles Brain trauma Research articles Brain trauma review articles Brain trauma PubMed articles Brain trauma PubMed Central articles Brain trauma 2023 articles Brain trauma 2024 articles Brain trauma Scopus articles Brain trauma impact factor journals Brain trauma Scopus journals Brain trauma PubMed journals Brain trauma medical journals Brain trauma free journals Brain trauma best journals Brain trauma top journals Brain trauma free medical journals Brain trauma famous journals Brain trauma Google Scholar indexed journals Trauma epidemiology articles Trauma epidemiology Research articles Trauma epidemiology review articles Trauma epidemiology PubMed articles Trauma epidemiology PubMed Central articles Trauma epidemiology 2023 articles Trauma epidemiology 2024 articles Trauma epidemiology Scopus articles Trauma epidemiology impact factor journals Trauma epidemiology Scopus journals Trauma epidemiology PubMed journals Trauma epidemiology medical journals Trauma epidemiology free journals Trauma epidemiology best journals Trauma epidemiology top journals Trauma epidemiology free medical journals Trauma epidemiology famous journals Trauma epidemiology Google Scholar indexed journals Prognostic factors articles Prognostic factors Research articles Prognostic factors review articles Prognostic factors PubMed articles Prognostic factors PubMed Central articles Prognostic factors 2023 articles Prognostic factors 2024 articles Prognostic factors Scopus articles Prognostic factors impact factor journals Prognostic factors Scopus journals Prognostic factors PubMed journals Prognostic factors medical journals Prognostic factors free journals Prognostic factors best journals Prognostic factors top journals Prognostic factors free medical journals Prognostic factors famous journals Prognostic factors Google Scholar indexed journals ipsilateral mydriasis articles ipsilateral mydriasis Research articles ipsilateral mydriasis review articles ipsilateral mydriasis PubMed articles ipsilateral mydriasis PubMed Central articles ipsilateral mydriasis 2023 articles ipsilateral mydriasis 2024 articles ipsilateral mydriasis Scopus articles ipsilateral mydriasis impact factor journals ipsilateral mydriasis Scopus journals ipsilateral mydriasis PubMed journals ipsilateral mydriasis medical journals ipsilateral mydriasis free journals ipsilateral mydriasis best journals ipsilateral mydriasis top journals ipsilateral mydriasis free medical journals ipsilateral mydriasis famous journals ipsilateral mydriasis Google Scholar indexed journals skull fracture articles skull fracture Research articles skull fracture review articles skull fracture PubMed articles skull fracture PubMed Central articles skull fracture 2023 articles skull fracture 2024 articles skull fracture Scopus articles skull fracture impact factor journals skull fracture Scopus journals skull fracture PubMed journals skull fracture medical journals skull fracture free journals skull fracture best journals skull fracture top journals skull fracture free medical journals skull fracture famous journals skull fracture Google Scholar indexed journals phonoaudiology articles phonoaudiology Research articles phonoaudiology review articles phonoaudiology PubMed articles phonoaudiology PubMed Central articles phonoaudiology 2023 articles phonoaudiology 2024 articles phonoaudiology Scopus articles phonoaudiology impact factor journals phonoaudiology Scopus journals phonoaudiology PubMed journals phonoaudiology medical journals phonoaudiology free journals phonoaudiology best journals phonoaudiology top journals phonoaudiology free medical journals phonoaudiology famous journals phonoaudiology Google Scholar indexed journals high-energy traumas articles high-energy traumas Research articles high-energy traumas review articles high-energy traumas PubMed articles high-energy traumas PubMed Central articles high-energy traumas 2023 articles high-energy traumas 2024 articles high-energy traumas Scopus articles high-energy traumas impact factor journals high-energy traumas Scopus journals high-energy traumas PubMed journals high-energy traumas medical journals high-energy traumas free journals high-energy traumas best journals high-energy traumas top journals high-energy traumas free medical journals high-energy traumas famous journals high-energy traumas Google Scholar indexed journals
Article Details
1. Introduction
Extradural Hematoma occurs between 2.7 to 4% of cases of traumatic brain injury (TBI), [1-3] but counts for a significant proportion of fatal head injuries with mortality rates ranging from 1.2 to 33% [4]. Mortality is higher in patients with low Glasgow Coma Scale (GCS), pupillary alteration, elderly and/or prolonged time between clinical deterioration and surgery [3]. The aging range of affected patients varies from 2 to 60 years, with a mean age of 20 to 30 years and less frequently embracing extremes of age [1, 3]. EDHs are a traumatic accumulation of blood between the inner table of the skull and the stripped-off dural membrane and most of them develop due to arterial damage, forming a biconvex hematoma in the cerebral convexity [5, 6]. The classic clinical presentation is loss of consciousness immediately after the trauma, followed by a lucid interval in which there is recovery of the level of consciousness during some hours and a later deterioration, with symptoms such as obnubilation, contralateral hemiparesis and ipsilateral mydriasis [3].
The treatment of EDH is usually surgical, although there are some cases that can be managed conservatively [7]. Patients who meet all the following criteria may be treated conservatively, provided there is rigid clinical follow-up and control imaging: hematoma volume less than 30 cm3, thickness less than 15 mm, midline deviation less than 5 mm, GCS greater than 8, and no focal neurological deficit [3]. Several treatment guidelines on various aspects of TBI are available from the Brain Trauma Foundation [8]. EDH with a volume greater than 30 cm3 should be evacuated regardless of patient’s GCS. The expeditious surgical evacuation of EDHs is associated with an excellent prognosis and such procedures are considered among the most cost-effective operations performed by neurosurgeons, [9] especially because the underlying brain has usually been minimally injured [6]. However, despite the knowledge that outcome from surgical decompression and repair is related directly to patients preoperative neurological condition, there is no specific trauma and epidemiologic prognostic factors related that can contribute to the patient’s follow-up analysis.
The failure to comply with traffic laws and social living in an increasingly aggressive society, associated with an older population corroborates the increase in the number of cases. The knowledge of its epidemiology together with clinical and radiological follow-up contributes to diagnosis and treatment as well as to the promotion of public health measures. We believe that the establishment of prognostics factors based on the characteristics of the trauma can contribute to the management of such important disease, and this consideration deserves to be examined more closely.
2. Methods
2.1 Study design
Authors performed a retrospective study, including all surgical cases of EDH admitted in the Department of Neurosurgery from January 2005 through January 2016. All cases came from the same Department, allowing the inclusion and exclusion criteria to be equal and standardizing the samples.
2.2 Eligibility
All patients underwent clinical and neurological examination, laboratory evaluation and radiological exams (Computed Tomography-CT-scan) to assess the disease. The inclusion criteria were patients with EDH who underwent surgery and had clinical, neurological, and radiological information in the medical record. The exclusion criteria were patients who did not undergo surgery, patients with spontaneous extradural hematoma or other surgical pathology besides EDH and patients who were lost during follow-up period.
2.3 Surgical technique
Surgery was performed if the radiology was in line with the neurological presentation and there was one of the following features: patients with GCS score <9, anisocoria and those with a hematoma larger than 30 cm3 in size, regardless of the patient’s GCS score. Patients with an EDH smaller than 30 cm3, less than 15 mm in thickness, with less than 5mm of midline shift and a GCS score greater than 8, without focal deficits, were placed as candidates for nonsurgical management under close observation and serial CT scans [3]. The surgical planning was total removal of the HED.
2.4 Variables analyzed
The variables analyzed were age, gender, and neurological presentation before and after surgery, according to the GCS and Extended Glasgow Outcome Scale (GOS) respectively. Authors also analyzed trauma mechanism, period of hospitalization and tomographic finding on primary CT scan (associated intracranial pathologies, side of EDH and the presence of associated cranial bone fracture). Demographic data were compared with trauma mechanism. Trauma mechanism was analyzed according to the skull fracture, GCS, and GOS. GCS was compared with GOS and analyzed with the hospitalization time. GCS and GOS were studied according to the location and side of EDH and analyzed with hospitalization period. A female subgroup was also studied according to demographic data, trauma mechanism, GCS, and GOS.
2.5 Statistical analysis
Numerical results were presented in means and standard deviation, median and at the 25th and 75th percentile, minimal and maximal values. The categorical results were presented in absolute and relative frequency. The comparisons between more than two means were performed with one-way ANOVA. Post-hoc analyses were performed with the Bonferroni test. The correlation among the GCS, GOS, and hospitalization time were calculated using Spearman correlation test. Values of p<0.05 were considered significant. According to the retrospective analysis, patients were not submitted to a consent term, but the institution agreed with the study certain that the collection would not lead to patient exposure and would not affect the diagnosis or treatment.
3. Results
During the period from January 2005 to January 2016, 250 patients were evaluated by the Neurosurgical service with EDH and eligible for the study. All patients underwent craniectomy to evacuation of the EDH. The mean age was 31 years and 48.4% (121 patients) of diagnosed cases were younger than 29 years. The male gender was predominant (n=212, 84.8%). The most frequent initial neurological status, assessed by the GCS, was mild Traumatic Brain Injury (TBI) (n=164, 65.6%). The most frequent trauma mechanism was Fall (n=110, 44%), followed by Aggression (n=39, 15.6%), Motorcycle accident (n=31, 12.4%), Trampling (26, 10.4%), and Car accident (n=21, 8.4%). The demographic data of the studied population are summarized in Table 1.
|
Trauma mechanism |
Age |
Male gender |
Glasgow Coma Scale |
Total |
||||
|
≤ 29 |
30-49 |
≥ 50 |
3-8 |
9-12 |
13-15 |
|||
|
Fall |
56 |
31 |
23 |
91 |
14 |
12 |
84 |
110 |
|
Aggression |
17 |
20 |
2 |
36 |
5 |
11 |
23 |
39 |
|
Motorcycle |
12 |
15 |
4 |
25 |
11 |
4 |
16 |
31 |
|
Trampling |
12 |
10 |
4 |
23 |
4 |
5 |
17 |
26 |
|
Car |
11 |
7 |
3 |
17 |
7 |
3 |
11 |
21 |
|
Others |
13 |
7 |
3 |
20 |
3 |
7 |
13 |
23 |
|
Total |
121 |
90 |
39 |
212 |
44 |
42 |
164 |
250 |
Results are presented as number of patients.
Table 1: Demographic data of the study population.
In the preoperative period, most of patients with severe initial neurological status suffered Motorcycle and Car accident (n=18, 35%) (Table 2).
|
Trauma mechanism |
Glasgow Coma Scale |
Total (p<0.001) |
||
|
3-8 |
9-12 |
13-15 |
||
|
Motorcycle/Car |
18 (35%) |
7 (13%) |
27 (52%) |
52 (100%) |
|
Others |
26 (13%) |
35 (18%) |
137 (69%) |
198 (100%) |
|
Total |
44 (18%) |
42 (17%) |
164 (66%) |
250 (100%) |
Results are presented as number of patients.
Table 2: Initial neurological status according to the trauma mechanism.
In the postoperative period, the same mechanisms were responsible for the worst outcome (n=40, 40%) (Table 3).
|
Trauma mechanism |
Glasgow Outcome Scale |
Total (p<0.002) |
|
|
1-6 |
7-8 |
||
|
Motorcycle/Car |
21 (40%) |
31 (60%) |
52 (100%) |
|
Others |
27 (14%) |
171 (86%) |
198 (100%) |
|
Total |
48 (19%) |
202 (81%) |
250 (100%) |
Results are presented as number of patients.
Table 3: Outcome status according to the trauma mechanism.
The most commonly affected side was the left (n=132, 52.8%), but this fact did not represent difference between the groups according to the initial neurological status (p=0.994) and the outcome (p=0.850). The EDH was most often located in temporal (n=70, 28%), followed by frontal (n=58, 23.2%) and temporoparietal (n=44, 17.6%). In the preoperative period, the initial neurological status was affected by the location. The frontal location, for example, determined an initial GCS 13-15 in most cases (n=42, 72.4%). However, in the postoperative period, the outcome was not affected by the location (Table 4).
|
EDH location |
Glasgow Coma Scale (p=0.0024) |
Glasgow Outcome Scale (p=0.078) |
Total |
||||||
|
3-8 |
9-12 |
13-15 |
1 |
2 |
3-4 |
5-6 |
7-8 |
||
|
Temporal |
13 |
12 |
45 |
0 |
0 |
4 |
6 |
60 |
70 |
|
Frontal |
5 |
11 |
42 |
0 |
0 |
0 |
8 |
50 |
58 |
|
Temporoparietal |
8 |
5 |
31 |
2 |
0 |
0 |
5 |
37 |
44 |
|
Parietal |
11 |
1 |
13 |
0 |
1 |
3 |
5 |
16 |
25 |
|
Posterior fossa |
4 |
3 |
14 |
1 |
0 |
1 |
3 |
16 |
21 |
|
Frontotemporoparietal |
2 |
4 |
8 |
0 |
0 |
0 |
4 |
10 |
14 |
|
Parietooccipital |
1 |
3 |
6 |
0 |
0 |
0 |
4 |
6 |
10 |
|
Occipital |
0 |
3 |
5 |
0 |
0 |
0 |
1 |
7 |
8 |
|
Total |
44 |
42 |
164 |
3 |
1 |
8 |
36 |
202 |
250 |
Results are presented as number of patients.
Table 4: EDH location according to GCS and GOS.
Traumatic intracranial condition associated with EDH was present in 68 cases (27.2%). Contusion (n=44, 64.7%) was the most frequent, followed by traumatic Subarachnoid hemorrhage (n=15, 22%) and Subdural hemorrhage (n=9, 13.2%). However, those associations did not represent difference in initial neurological assessment (p=0.452) neither in the outcome (p=0.992). Also, traumatic intracranial pathology associated to EDH did not configure difference in the hospitalization time (p=0.533). Skull fracture occurred in 36.4% of the cases, 51% affecting the temporal bone. Patients remained hospitalized with an average length of 10 days. Those who had an initial neurological status with GCS (3-8) remained longer at hospital and those with better GCS (13-15) had a sooner hospital discharge (Table 5).
|
GCS |
N |
Hospitalization (days) |
p |
|
M |
|||
|
3-8 |
44 |
13.5 (9-23) |
0.003 |
|
9-12 |
42 |
11 (9-18) |
|
|
13-15 |
164 |
8 (7-11) |
N: Number of cases; M: Mean
Table 5: GCS classified by mean hospitalization time.
From patients who had a hospital discharge with better outcomes, GOS 7-8 (n=202, 82%), most of them remained hospitalized from 7 to 10 days (n=102, 50.5%). Patients who remained hospitalized for 14 days or more (n=64, 25.6%), presented the highest rate of worse outcomes at hospital discharge (n=30, 43%). Patients who presented lower rates of hospitalization time tended to have a hospital discharge with better outcomes. On the other hand, patients with the highest rates of hospitalization time tended to have a hospital discharge with the worst outcomes (Figure 1). Patients who initially presented mild (GCS 13-15) TBI (n=164, 65.6%), most of them frequently had a good outcome (GOS 7+8) at hospital discharge (n=153, 93.3%), letting them able to return to the original function (Figure 2). On the other hand, patients with severe (GCS 3-8) TBI (n=44, 17.6%) presented good outcome in the smallest number of cases (n=20, 45.5%). When the authors analyzed specifically patients with severe disability or worse outcome (GOS grade 1+2+3+4), totalizing 12 patients, 8 patients (66%) were initially manifested with severe TBI. Females represented only 15.2% (n=38) of the sample. The authors analyzed this subgroup of patients to find out possible differences with the general population. The mean age was 23 years and 68.4% (n=26) of cases were younger than 29 years when diagnosing.
The most frequent initial neurological status was mild TBI (n=29, 76.3%). The most frequent trauma mechanism was Fall (n=19, 50%), followed by Motorcycle accident (n=6, 15.8%) and Car accident (n=4, 10.5%). In the preoperative period, most of patients who presented severe initial neurological status suffered Motorcycle and Car accident (n=3, 30%). In the postoperative period, the same mechanisms were responsible for the worst outcome (n=3, 30%). Most patients (n=34, 89.5%) had a good outcome (GOS 7+8) at hospital discharge (p=0.019). The most frequent affected side by EDH was the left one, location was temporal, traumatic intracranial condition was Contusion and skull fracture was temporal bone, but these conditions did not configure difference in the hospitalization time, initial neurological assessment or outcome.
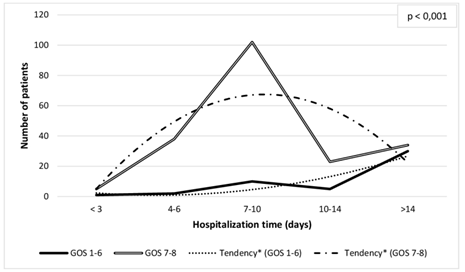
Figure 1: Glasgow Outcome Scale stratified by hospitalization time.
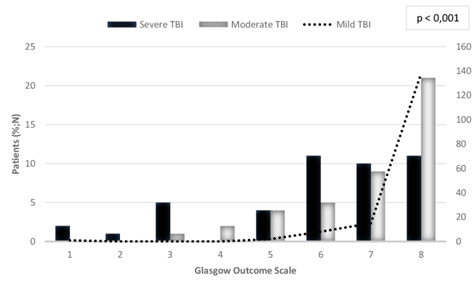
Figure 2: Relationship between TBI and GOS.
4. Discussion
Extradural hematoma occurs most frequently secondarily to laceration of meningeal vessels, diploic veins or dural sinuses in traumatic head injuries with skull fractures [10-12]. Blood overflows into the epidural space between the inner tabula of the skull and periosteal layer of dura mater. The dura mater is pulled away by the hematoma resulting in the characteristic biconvex shape. In only about 10% of cases, EDH occurs in the absence of a fracture. This low rate is often seen in children since the pediatric skull is more elastic and compliant than the adult skull [10]. However, in our study, skull fracture was presented in only 36.4% of the cases, most frequently in the temporal bone. This low rate gives an alert that even when no fracture can be seen in X-ray or CT scan, EDH may be present.
EDH may have an arterial or venous origin. Most arterial EDH occurs in the temporoparietal region, the location in which the middle meningeal artery is especially vulnerable, due to the close anatomic relation, thinness of temporal scales and greater exposure to external traumas [3]. Venous EDH is much less common and usually comes from laceration of dural venous sinus, or injury to meningeal or diploic veins. For this reason, venous EDH is often adjacent to a dural sinus. In our study, the most frequent location of EDH was the temporal region, followed by the frontal and temporoparietal regions, with 52.8% occurring on the left hemisphere. Other series of literature describe the temporoparietal and temporal regions as the most frequent [13]. The EDH location appears to be an important factor to establish the initial GCS. It has been checked that frontal location was proportionally associated with a better GCS, and on the other hand, the parietal location was the most associated with worst GCS, followed by temporoparietal region. However, location did not affect the outcome of patients in our series. At the same time, the most affected side was the left and this fact did not change GCS and outcome.
EDH is more common in adults than in children, except for posterior fossa EDH, which is more often seen in children than in adults and is usually a result of laceration of the dural sinuses [14]. The proportion between man and woman is around 4:1. We observed in our study population that EDH was most frequently in male young adult patients, between the first and third decades of life. In this age distribution, patients with active life are more frequently exposed to risk situations, such as motorcycle traffic accidents without wearing a helmet, driving without a seat belt, and thus being more vulnerable to TBI. In elderly patients, EDH is less frequent due to cinematic and anatomical reasons. Analyzing the cinematics of TBI in patients older than 65 years old, it is noticed that most have traumas secondary to Falls or mild TBI by different types of objects. The incidence of high-energy traumas is lower in this population. Besides, when analyzing anatomical factors, it is known that the strong adhesion of the dura mater to the skull makes it difficult to detach and accumulate blood. Besides, the bone thickness in elderly is larger, and therefore harder to be broken. In children, because there is no bone groove that houses the middle meningeal artery completely formed, the lesion of this artery is less frequent, and therefore hematoma formation is also more uncommon [5].
EDH usually results from trauma and is rare due to non-accidental injury. In our study, the main mechanism of trauma found was Fall, followed by Physical aggression. These mechanisms are justified by the pathogenesis of EDH, which is more associated with mild and moderate TBI, such as Falls of small heights, Physical aggressions and others, [1, 15] and varies according to the socioeconomic and demographic characteristics of each studied region. However, when we analyze which mechanism is more responsible concerning the neurological status, other mechanisms must be considered. The subgroup that was most correlated with worst initial neurological status and therefore had patients with worst outcome was represented by Motorcycle and Car accidents. These mechanisms correspond to higher-energy trauma and can be associated with the presence of others primary or secondary brain injury [16]. In our study, Contusion was the traumatic intracranial condition most frequently linked to EDH. This type of intracerebral hemorrhage leads to acute ischemia in the immediately adjacent brain, which in turn is surrounded by a penumbra of functionally impaired tissue, but potentially recoverable [16]. This physiopathology explains why the association between Contusion and EDH did not represent difference in initial GCS and outcome, and also in the hospitalization time of patients in our study.
Applying the GCS on admission, we observed a predominance of mild TBI (GCS between 13 and 15), confirming the low energy mechanism that most frequently leads to trauma, with little repercussion to the brain parenchyma. Patients with mild TBI had a good outcome and a sooner average hospital discharge than those with severe TBI, who presented a worse outcome and therefore remained hospitalized for longer periods. Patients with favorable outcome were able to follow their daily routine and labor activities. Among patients who presented severe TBI, 81% progressed to a moderate disability (GOS 5+6) or good recovery (GOS 7+8) outcome, attributed it to the surgery. Analyzing the patients who died (3 patients), 2 of them initially presented severe TBI and 1 mild TBI. All of these cases were secondary to Fall, representing a mechanism of trauma that, despite being related to lower energy mechanism, may provide a worse prognosis. Other series also found that the initial GCS score was an important factor affecting outcome [17]. This situation can be especially important to physician when globally conducting each case. A patient with worst initial GCS tends to spend more time at hospital and requires more interdisciplinary care, such as physiotherapy and phonoaudiology, because they will probably have a worst outcome. Also analyzing the initial GCS, physician can explain to the family about the possible time of hospital discharge and special care that should be required after hospital discharge.
Case series represent the most important and frequent data to studies related to EDH. Meanwhile, they are not represented by checklist guidelines that ensure their quality and transparency, such as the Process Guidelines, [18] which consists of an eight item checklist that improves the quality of surgical case series. The female group analysis performed by authors is also not considered in previously series. We verified that some characteristics were the same as in the general population: the mean age of presentation (less than 29 years), the initial neurological status (mild TBI), the most frequent trauma mechanism (Fall), side affected (left), location (temporal), skull fracture (temporal) and associated trauma (Concussion). The worst trauma mechanisms (motorcycle and car accidents) were also responsible for the worst outcome. Female subgroup showed an important difference among the general group: most patients had a good outcome at hospital discharge even considering patients with worst initial neurological status.
5. Strengths and study limitations
The strengths of the study were the capacity to carry out the follow-up, the external applicability and the large number of patients. The limitation of the study was related to the retrospective design. The study group is ready to start a prospective and multicenter study to evaluate patients with traumatic EDH, and to accurately predict prognostic factors and outcomes.
6. Conclusion
There are some trauma and epidemiologic characteristics related to EDH that can qualify the decision-making to a surgically treated patient. We believe that some prognostic conditions must be considered to allow physicians and their team to be prepared for special care hospitalization time and to give better information outcome related to patient’s relatives. Patients affected by Motorcycle and Car accidents tend to present worst GCS and Outcome. In addition, parietal location is correlated with worst neurological status. However, frontal location corresponds to better GCS and female gender to better outcome. GCS and hospitalization time were directly associated with outcome, which tends to be worst in a long-term hospital discharge.
Acknowledgements
The authors would like to thank all staffs and professors of the Department of Neurosurgery of the Cristo Redentor Hospital for the encouragement to develop this important research. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- Bricolo A, Pasut L. Extradural hematoma: toward zero mortality. A prospective study. Neurosurgery 14 (1984): 8-12.
- Gupta S, Tandon S, Mohanty S, et al. Bilateral traumatic extradural haematomas: Report of 12 cases with a review of the literature. Clin Neurol Neurosurg 94 (1992): 127-131.
- Bullock MR, Chestnut R, Ghajar J, et al. Surgical management of acute epidural hematomas. Neurosurgery 58 (2006): 7-15.
- Ruff LM, Mendelow AD, Lecky FE. Improving mortality after extradural haematoma in England and Wales. Br J Neurosurg 27 (2013): 19-23.
- Greenberg MS. Handbook of Neurosurgery. Porto Alegre (RS): 7th Artmed (2013): 997-1000.
- Bir SC, Maiti TK, Ambekar S, et al. Incidence, hospital costs and in-hospital mortality rates of epidural hematoma in the United States. Clin Neurol Neurosurg 138 (2015): 99-103.
- Bullock R, Smith R, van Dellen JR. Nonoperative management of extradural hematoma. Neurosurgery 16 (1985): 602-606.
- Brain Trauma Foundation. Guidelines for the management of severe traumatic brain injury. (4th) (2016).
- Pickard JD, Bailey S, Sanderson H, et al. Steps towards costbenefit analysis of regional neurosurgical care. BMJ 301 (1990): 629-635.
- Gean AD. Extra-axial collections. In: Imaging of head trauma. New York: Raven press (1994): 107-124.
- Huisman TA. Intracranial hemorrhage: ultrasound, CT and MRI findings. Eur Radiol 15 (2005): 434-440.
- Katzman GL. Epidural hematoma. In: Osborne AG, editor. Diagnostic imaging-brain. Salt Lake City, Utah: Amirsys (2004).
- Pereira CU, Santos EAS, Cavalcante S, et al. Hematoma extradural intracraniano. Journal bras neurocir 16(2005): 25-34.
- Hamilton M, Wallace C. Nonoperative management of acute epidural hematoma diagnosed by CT: the neuroradiologist’s role. Am J Neuroradiol 13 (1992): 853-859.
- Luna F, Falndez ZB, Morales M, et al. Hematoma extradural: revisión de 100 casos operados. Rev chil neuro-psiquiatr 35 (1997): 229-232.
- Mendelow A, Bullock R. Intracranial haemorrhage induced at arterial pressure in the rat: Part 2. Short term changes in local cerebral blood flow measured by autoradiography. Neurology Research (1984): 189.
- Kuday C, Uzan M, Hanci M. Statistical analysis of the factors affecting the outcome of extradural haematomas: 115 cases. Acta Neurochir 131 (1994): 203-206.
- Agha RA, Fowler AJ, Rajmohan S, et al. PROCESS Group. Preferred reporting of case series in surgery; the PROCESS guidelines. Int J Surg 36 (2016): 319-323.
