Primary Malignant Brain Tumor Trends in Southern Iran, 2001- 2017: An Alarming increase in Glioblastoma
Article Information
Ahmad Soltani1, Iman Ahrari1*, Meisam Eqbal2, Seyed Hossein Owji3, Amir Mousaie Amin1, Zahra Khosravizadegan4, Mahsa Ghavipisheh5, Abbas Rezaianzadeh6, Hadi Raeisi Shahraki7
1Department of Neurosurgery, Shiraz University of Medical Sciences, Shiraz Iran.
2Sinopec Medical Center, Department of QHSE, Sinopec International Petroleum E&P Corporation, Yadavaran Oil Field, Ahwaz, Iran.
3Department of Otolaryngology, Shiraz University of Medical Sciences, Shiraz, Iran.
4Vice chancellery for health, Shiraz University of Medical Sciences, Shiraz, Iran.
5Psychiatry Department, Shiraz University of Medical Sciences, Shiraz, Iran.
6Colorectal research center, Shiraz University of Medical Sciences, Shiraz, Iran.
7Department of Biostatics and Epidemiology, Shaherkord University of Medical Sciences, Iran
*Corresponding Author: Iman Ahrari M.D., Department of Neurosurgery, Shiraz University of Medical Sciences, Shiraz Iran.
Received: 30 April 2022; Accepted: 09 May 2022; Published: 18 May 2022
Citation: Ahmad Soltani, Iman Ahrari, Meisam Eqbal, Seyed Hossein Owji, Amir Mousaie Amin, Zahra Khosravizadegan, Mahsa Ghavipisheh, Abbas Rezaianzadeh, Hadi Raeisi Shahraki. Primary Malignant Brain Tumor Trends in Southern Iran, 2001- 2017: An Alarming Increase In Glioblastoma. Journal of Surgery and Research 5 (2022): 284-295.
View / Download Pdf Share at FacebookAbstract
Introduction
Primary Brain tumors which include a 1.7 percent of all cancers among which glioblastomas are the most lethal and the most frequent malignant types. Ionizing radiation and some genetic factors have been reported as the etiology of such cancers. We are reporting the trends in the Brain tumors with a focus on malignant types and its outcome in the South of the Iran for the first time.
Methods
We selected all the patients with primary brain tumors who undergone brain surgery at teaching hospitals the Shiraz Medical School between 2001 and 2017. Data was obtained from Fars Population-based Cancer Registry. ICD-O-3 morphology coding system according to WHO 2007 classification of CNS tumors was used for grouping the tumors. Using SPSS, Total Growth Rate (TGR) and Incidence Rate (IR) were calculated to assess the changes overtime.
Results
A total number of 2130 (male: 890, 41.8% and female: 1240, 58.2%) brain tumor cases from 2001 to 2017 were included in this study. The highest Incidence Rate (IR) was found in ‘unspecified tumors of the brain’ (2.74 per 100000) between 2011 and 2015 followed by ‘Astrocytoma’ (1.34 per 100000) between 2006 and 2010) and ‘Glioblastoma’ (1.25 per 100000) between years 2011 and 2016. Additionally, the Glioblastoma showed the highest IR in those aged between 30 and 59 of years (0.42 per 100000).
Conclusion
An upward trend in the rate of malignant brain tumors in the Fars province could be an alarm sign for more studies to be done especially from the etiology point of view.
Keywords
Primary brain tumor, Malignant, Incidence rate, Trend, Glioma
Primary brain tumor articles; Malignant articles; Incidence rate articles; Trend articles; Glioma articles
Primary brain tumor articles Primary brain tumor Research articles Primary brain tumor review articles Primary brain tumor PubMed articles Primary brain tumor PubMed Central articles Primary brain tumor 2023 articles Primary brain tumor 2024 articles Primary brain tumor Scopus articles Primary brain tumor impact factor journals Primary brain tumor Scopus journals Primary brain tumor PubMed journals Primary brain tumor medical journals Primary brain tumor free journals Primary brain tumor best journals Primary brain tumor top journals Primary brain tumor free medical journals Primary brain tumor famous journals Primary brain tumor Google Scholar indexed journals malignant brain neoplasms articles malignant brain neoplasms Research articles malignant brain neoplasms review articles malignant brain neoplasms PubMed articles malignant brain neoplasms PubMed Central articles malignant brain neoplasms 2023 articles malignant brain neoplasms 2024 articles malignant brain neoplasms Scopus articles malignant brain neoplasms impact factor journals malignant brain neoplasms Scopus journals malignant brain neoplasms PubMed journals malignant brain neoplasms medical journals malignant brain neoplasms free journals malignant brain neoplasms best journals malignant brain neoplasms top journals malignant brain neoplasms free medical journals malignant brain neoplasms famous journals malignant brain neoplasms Google Scholar indexed journals Incidence rate articles Incidence rate Research articles Incidence rate review articles Incidence rate PubMed articles Incidence rate PubMed Central articles Incidence rate 2023 articles Incidence rate 2024 articles Incidence rate Scopus articles Incidence rate impact factor journals Incidence rate Scopus journals Incidence rate PubMed journals Incidence rate medical journals Incidence rate free journals Incidence rate best journals Incidence rate top journals Incidence rate free medical journals Incidence rate famous journals Incidence rate Google Scholar indexed journals Glioma articles Glioma Research articles Glioma review articles Glioma PubMed articles Glioma PubMed Central articles Glioma 2023 articles Glioma 2024 articles Glioma Scopus articles Glioma impact factor journals Glioma Scopus journals Glioma PubMed journals Glioma medical journals Glioma free journals Glioma best journals Glioma top journals Glioma free medical journals Glioma famous journals Glioma Google Scholar indexed journals orphology coding system articles orphology coding system Research articles orphology coding system review articles orphology coding system PubMed articles orphology coding system PubMed Central articles orphology coding system 2023 articles orphology coding system 2024 articles orphology coding system Scopus articles orphology coding system impact factor journals orphology coding system Scopus journals orphology coding system PubMed journals orphology coding system medical journals orphology coding system free journals orphology coding system best journals orphology coding system top journals orphology coding system free medical journals orphology coding system famous journals orphology coding system Google Scholar indexed journals CNS tumors articles CNS tumors Research articles CNS tumors review articles CNS tumors PubMed articles CNS tumors PubMed Central articles CNS tumors 2023 articles CNS tumors 2024 articles CNS tumors Scopus articles CNS tumors impact factor journals CNS tumors Scopus journals CNS tumors PubMed journals CNS tumors medical journals CNS tumors free journals CNS tumors best journals CNS tumors top journals CNS tumors free medical journals CNS tumors famous journals CNS tumors Google Scholar indexed journals morphology coding system articles morphology coding system Research articles morphology coding system review articles morphology coding system PubMed articles morphology coding system PubMed Central articles morphology coding system 2023 articles morphology coding system 2024 articles morphology coding system Scopus articles morphology coding system impact factor journals morphology coding system Scopus journals morphology coding system PubMed journals morphology coding system medical journals morphology coding system free journals morphology coding system best journals morphology coding system top journals morphology coding system free medical journals morphology coding system famous journals morphology coding system Google Scholar indexed journals malignant gliomas articles malignant gliomas Research articles malignant gliomas review articles malignant gliomas PubMed articles malignant gliomas PubMed Central articles malignant gliomas 2023 articles malignant gliomas 2024 articles malignant gliomas Scopus articles malignant gliomas impact factor journals malignant gliomas Scopus journals malignant gliomas PubMed journals malignant gliomas medical journals malignant gliomas free journals malignant gliomas best journals malignant gliomas top journals malignant gliomas free medical journals malignant gliomas famous journals malignant gliomas Google Scholar indexed journals radiofrequency noises articles radiofrequency noises Research articles radiofrequency noises review articles radiofrequency noises PubMed articles radiofrequency noises PubMed Central articles radiofrequency noises 2023 articles radiofrequency noises 2024 articles radiofrequency noises Scopus articles radiofrequency noises impact factor journals radiofrequency noises Scopus journals radiofrequency noises PubMed journals radiofrequency noises medical journals radiofrequency noises free journals radiofrequency noises best journals radiofrequency noises top journals radiofrequency noises free medical journals radiofrequency noises famous journals radiofrequency noises Google Scholar indexed journals
Article Details
1. Introduction
Primary Brain tumors which include a 1.7 percent of all cancers [1] are a heterogeneous group of diseases that their entity could be categorized based on the biological behavior, histopathological pattern as well as morphology, anatomical location and age [2,3]. Although the precise etiology of brain tumors have not been identified yet, several studies have reported risk factors such as Ionizing radiation and some genetic factors for both benign and malignant brain neoplasms [4-6]. The clinical manifestations of such tumor usually originates from the anatomic location of the tumor and the part of the brain which is involved, however, the tumor most prevalent clinical presentation include seizure, headache, fatigue and cognitive dysfunction [7]. Based on tumor type and anatomical location, malignancy potential, and the patient's age, treatment strategy could be different for each patients and usually includes a combination of surgery in addition to radiotherapy, and chemotherapy. Additionally, imaging has been always the most common method for diagnosis if such tumors [7,8]. From the prevalence point of view, among these intracranial tumors, Meningiomas, representing 36 percent of all, are the most frequent type. On the other hand, Gliomas are the most frequent malignant type which consist of 75 percent of cases presenting with malignant brain tumors [1]. Several studies have reported the trend of the intracranial tumors in different countries (9-17). The incidence rate of tumors are controversial especially regarding malignant tumors. Most of these studies have reported an increase in the incidence of malignant and non-malignant brain tumors in elderly and also adolescents [11,14]. However there are reports from some countries which did not showed any overall increase trend in incidence of malignant tumors [13]. Some studies have reported a plateaued or even decreasing trend in the incidence of the CNS tumors in general [18]. On the other hand, some of these papers have reported difference between incidence of CNS tumors in males and females [15].
In Iran, Araghi et al have reported an increase trend of brain and CNS tumors for all ages in Golestan Province located in the South East littoral of the Caspian Sea in Northern Iran. They have also reported a higher incidence rate in men than in women [9]. In this current study, we are reporting the trends in the Brain tumor and its outcome in the South and Southwest of the Iran for the first time.
2. Methods
2.1 Data resources
The current data is collected from Cancer registry center (CRC) belonging to Shiraz University of Medical Sciences which was established in (1995). Fars province is located in the southwest of the Iran and its capital is Shiraz city. This province has a population of 4.85 million according to the latest census in 2016 representing about six percent of total Iranian population.. Shiraz University of Medical Sciences, one the oldest medical schools nationwide, has four main general teaching hospitals (Namazi, Chamran, Rajae and Sa’di) and have been hosting patients from the most of the south and west part of the Iran. For current study, we selected all the patients with primary brain tumors who undergone brain surgery from 2001 to 2017. Demographic data of patients including gender, age at diagnosis, calendar year of diagnosis and history of previous malignancy were obtained. Tumor characteristics including tumor location, type and tumor size were also considered. ICD-O-3 morphology coding system according to WHO 2007 classification of CNS tumors was used for grouping the tumors (Table 1) [13]. The primary malignant barin tumors (ICD-O-3 morphology codes 9380–9451) and other unspecified primary brain tumors (ICD-O-3 morphology code 8000) were included. Additionally, based on data on cancer registery form the tumor location was reclassified according to ICD-O-3.
|
Glioma subtype |
Morphology code |
|
Astrocytic tumors |
|
|
Astrocytoma |
9400, 9411, 9420 |
|
Anaplastic astrocytoma |
9401 |
|
Glioblastoma |
9440–9442 |
|
Oligodendroglial tumors |
|
|
Oligodendroglioma |
9450 |
|
Anaplastic oligodendroglioma |
9451 |
|
Oligoastrocytic tumors |
|
|
Oligoastrocytoma grade II and III |
9382 |
|
Ependymal tumors |
|
|
Ependymoma |
9391, 9393 |
|
Anaplastic ependymoma |
9392 |
|
Unspecified malignant glioma |
9380 |
|
Other malignant tumors |
|
|
Other specified tumors of the brain |
9381, 9390, 9424, 9430, 9470, |
|
Unspecified tumors of the brain |
8000 |
Table 1: malignant primary brain tumors based on ICD-O-3
All the patients who have undergone surgery for brain tumor and their data were registered in Tumor Registry Center got involved in this study. There was no age or sex limitation. The patients whom their birth place were out of Fars provenance or where living out of this provenance were excluded. All the patient who had a second surgery due to recurrence were also excluded. Incidence rate was calculated with 95% confidence intervals (CI) for all tumors divided based on age group, histological type, year of diagnosis and gender. The average annual percent change (APC) was estimated using the following formula: (Numbers at 2016- Numbers at the first year of diagnosis)/(Numbers at the first year of diagnosis*duration). All the calculation were performed in SPSS Version 21.0.
3. Results
A total number of 2130 (male: 890, 41.8% and female: 1240, 58.2%) brain tumors were reported to the FPCR during 2001 to 2017. Divided by the age-groups, in total, the number of the cases were mostly aged between 50-60 (n=390, 18.3 %) followed by 30-40 years old (n=328, 15.4%). Additionally, the number of cases in those between 20-30 years of age was less than in other age groups (Table 2).
|
Variable |
Subgroup |
Frequency |
|
|
Number |
% |
||
|
Gender |
Female |
890 |
41.8 |
|
Male |
1240 |
58.2 |
|
|
Age Group |
<20 |
267 |
12.5 |
|
20-30 |
237 |
11.1 |
|
|
30-40 |
328 |
15.4 |
|
|
40-50 |
320 |
15 |
|
|
50-60 |
390 |
18.3 |
|
|
60-70 |
301 |
14.1 |
|
|
>70 |
287 |
13.5 |
|
Table 2: The frequency of malignant brain tumors based on gender and age groups
The Total Growth Rate (TGR) of the tumors in males and females was almost equal (62 and 61.5 % respectively). However, this growth in various subgroups was quite different. TGR showed a 160 % increase in those older than 70 years old followed by 100 % increase in those younger than 20 years old. The least increase was also in those with 20-30 years old of age (5.6%) (Table 3).
|
Variable |
Subgroup |
Total growth rate (%) |
|
Gender |
Female |
61.5 |
|
Male |
62 |
|
|
Age Group |
<20 |
100 |
|
20-30 |
5.6 |
|
|
30-40 |
43.3 |
|
|
40-50 |
48.9 |
|
|
50-60 |
36.7 |
|
|
60-70 |
38.7 |
|
|
>70 |
160 |
Table 3: The TGR of malignant brain tumors based on gender and age groups
Among all the tumor types diagnosed based on the histopathological features, the maximum TGR was found in Glioblastoma (+360 %) followed by Anaplastic Astrocytoma (+33.3 %). However, those categorized as ‘Unspecified tumors of the braain’ showed a +323.2 % of TGR. On the other hand, Ependymoma showed a 0 % of TGR. Additionally, the overall TGR of the brain tumors was found as +61.8 5 during these years (Table 4). Additionally, figure 1 shows the trend of various types of malignant brain tumors based on the number of the patients between years 2001 to 2016.
|
Tumor |
Subgroup |
Frequency |
Total growth rate (%) |
|
|
Number |
% |
|||
|
Astrocytic tumors |
Astrocytoma |
505 |
23.7 |
12.7 |
|
Anaplastic astrocytoma |
128 |
6 |
33.3 |
|
|
Glioblastoma |
388 |
18.2 |
306.7 |
|
|
Oligodendroglial tumors |
Oligodendroglioma |
81 |
3.8 |
28.6 |
|
Anaplastic oligodendroglioma |
57 |
2.7 |
27.3 |
|
|
Oligoastrocytic tumors |
Oligoastrocytoma grade II and III |
34 |
1.6 |
7.7 |
|
Ependymal tumors |
Ependymoma |
51 |
2.4 |
0 |
|
Anaplastic ependymoma |
9 |
0.4 |
25 |
|
|
Unspecified malignant glioma |
46 |
2.2 |
2.2 |
|
|
Other malignant tumors |
Other specified tumors of the brain |
210 |
9.9 |
12.4 |
|
Unspecified tumors of the brain |
621 |
29.2 |
323.2 |
|
|
Total |
2130 |
100 |
61.8 |
|
Table 4: The TGR of various kind of brain tumors.
For the five most important tumors of the brain from this study’s point of view, the trend is shown in the figure 1. Almost all the tumors showed an increase trend from 2001 to 2010 and after that, stabilized. However an outbreak in the number of the unspecified tumors of the brain was found from 2012 to 2016.
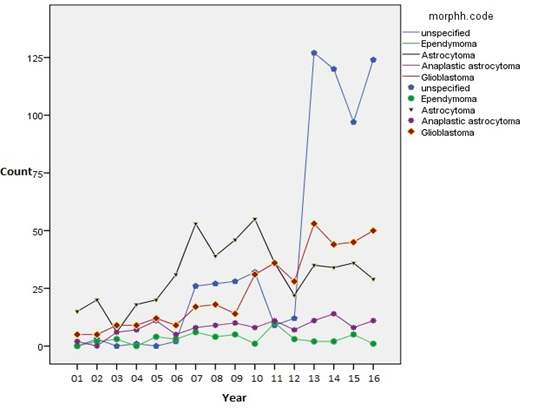
Figure 1: Trends of the tumors of the brain based on the number of the each tumor from 2001 to 2016.
In term of anatomical location of the tumors, the most prevalent location of malignant brain tumors was reported as unspecified, these consist of cases that the exact tumor location was not mentioned (n=1198, 56.2%). However, in those which location was exactly reported, the most prevalent one was the frontal lobe (n=275, 12.9%) followed by the parietal lobe (n=208, 9.8%). Interestingly, although the number of the malignant neoplasms of the ‘overlapping sites of the brain’ was not quite a lot, the TGR of the tumors in this group was the highest among the various tumors anatomical locations (Table 5).
|
Anatomical location |
Frequency |
Numbers at the first year of diagnosis |
Numbers in 2016 |
Total growth rate (%) |
|
|
Number |
% |
||||
|
C71.0 |
27 |
1.3 |
1 |
3 |
16.7 |
|
C71.1 |
275 |
12.9 |
4 |
27 |
38.3 |
|
C71.2 |
208 |
9.8 |
2 |
13 |
36.7 |
|
C71.3 |
100 |
4.7 |
1 |
5 |
30.8 |
|
C71.4 |
43 |
2 |
1 |
4 |
27.3 |
|
C71.5 |
29 |
1.4 |
1 |
2 |
7.7 |
|
C71.6 |
107 |
5 |
5 |
13 |
10.7 |
|
C71.7 |
22 |
1 |
1 |
3 |
13.3 |
|
C71.8 |
121 |
5.7 |
1 |
18 |
113.3 |
|
C71.9 |
1198 |
56.2 |
9 |
138 |
95.6 |
|
Total |
2130 |
100 |
22 |
226 |
61.8 |
Table 5: Frequency and TGR of the malignant brain tumors categorized based on their anatomical location (C71.0: malignant neoplasm of cerebrum, except lobes and ventricles, C71.1: malignant neoplasm of frontal lobe, C71.2: malignant neoplasm of temporal lobe, C71.3: malignant neoplasm of parietal lobe, C71.4: malignant neoplasm of occipital lobe, C71.5: malignant neoplasm of cerebral ventricle, C71.6: malignant neoplasm of cerebellum, C71.7: malignant neoplasm of brain stem, C71.8: malignant neoplasm of overlapping sites of brain, C71.9: malignant neoplasm of brain unspecified).
The Incidence Rate (IR) per 100,000 population of various brain tumors is represented in Table 6. The highest IR was found in ‘unspecified tumors of the brain’ (2.74 per 100000) between 2011 and 2015 followed by ‘Astrocytoma’ (1.34 per 100000) between 2006 and 2010) and ‘Glioblastoma’ (1.25 per 100000) between years 2011 and 2016.
|
Tumor |
Subgroup |
Time period |
||
|
2001-2005 |
2006-2010 |
2011-2016 |
||
|
Astrocytic tumors |
Astrocytoma |
0.66 |
1.34 |
0.89 |
|
Anaplastic astrocytoma |
0.18 |
0.27 |
0.29 |
|
|
Glioblastoma |
0.29 |
0.68 |
1.25 |
|
|
Oligodendroglial tumors |
Oligodendroglioma |
0.09 |
0.19 |
0.18 |
|
Anaplastic oligodendroglioma |
0.01 |
0.09 |
0.21 |
|
|
Oligoastrocytic tumors |
Oligoastrocytoma grade II and III |
0.01 |
0.01 |
0.16 |
|
Ependymal tumors |
Ependymoma |
0.07 |
0.15 |
0.07 |
|
Anaplastic ependymoma |
0.006 |
0.02 |
0.01 |
|
|
Unspecified malignant glioma |
0 |
0.05 |
0.21 |
|
|
Other malignant tumors |
Other specified tumors of the brain |
0.27 |
0.23 |
0.31 |
|
Unspecified tumors of the brain |
0.03 |
0.71 |
2.74 |
|
Table 6: The Incidence Rate of various brain tumors in different time periods.
The IR of the five most important primary brain tumor from the perspective of our study was calculated for different age groups in the entire sixteen years of the study which is reported in the Table 7. In this regard, the highest IR was found in ‘Unspecified malignant glioma’ (0.55) in those aged more than sixty years old followed by Astrocytoma in those aged 3-59 years (0.52). Additionally, the Glioblastoma showed the highest IR in those aged between 30 and 59 of years (0.42). (Figure 2)
|
Tumor |
Subgroup |
Age groups |
||
|
<30 yrs |
30-59 yrs |
>60 yrs |
||
|
Astrocytic tumors |
Astrocytoma |
0.31 |
0.52 |
0.12 |
|
Anaplastic astrocytoma |
0.04 |
0.17 |
0.03 |
|
|
Glioblastoma |
0.11 |
0.42 |
0.21 |
|
|
Ependymal tumors |
Ependymoma |
0.05 |
0.02 |
0.01 |
|
Unspecified malignant glioma |
0.14 |
0.48 |
0.55 |
|
Table 7: The IR of the five most important brain tumors from the perspective of this study in different age groups for the entire 16 years.
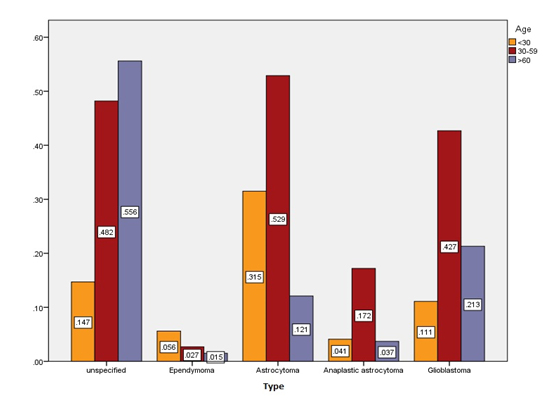
Figure 2: The incidence rate of five different tumors based on age groups.
3. Discussion
In this descriptive study, we found an upward trend in the rate of malignant brain tumors in the Fars province which is located in south part of Iran between 2001 and 2016. The most common types of such tumors were unspecified glioma, Astrocytoma and Glioblastoma. This finding is compatible with the previous reports in Iran [19,20]. In term of incidence rate trend, Araghi et al have reported a stabilization in the trends after 2008 [9]; in our study in the most subgroups based on the histopathological features, it shows such a stabilization. However, an upward trend was found in malignant subgroups such as Glioblastoma and anaplastic astrocytoma. Yet, the difference between our study and Araghi et al. study is the duration of our study. They reported data from 2004 to 2013 while we are reporting data from 2001 to 2016 which may affect the reliability of our data. However, the geographical location for the studies has also been reported as an important factor in recent studies both from Iran and worldwide [21] which could affect the result of each study. Besides, an important result of our study showed a dramatic increase in the TGR of malignant brain tumors in age group less than 20 years (a 100% increase in TGR), in addition to a considerable increase in TGR of Glioblastoma which showed a +306.7 percent increase during these years. Additionally, in those aged between 30 and 59 years of age, the IR of the most important primary malignant brain tumors showed the highest level which is not reported before in Iran. On the other hand, in a recent study published by Salimi et al in 2020, they also have reported an increasing trend of overall CNS tumors [21]. However they have reported of all kind of the CNS tumors while we are reporting of just the malignant brain tumors. The stabilization in the incidence trend of malignant tumors are reported in different studies in Europe, although they reported an increase in incidence rate of overall benign tumors but malignant glioma of brain remained in a plateau [13,23]. Such important results need to be accurately followed in the future to fully understand whether an outbreak of malignant brain tumors is happening in special group of people in the Iranian society or not. There are several reports of trends in brain tumors incidence worldwide both in adults and children [10, 11, 13-17, 22, 23]. Some of these studies have reported a stable increase rate with no departure from linearity [13]. On the other hand, some has reported an increase in annual incidence rate of benign tumors only and has reported the malignant ones stable [23]. In our study, we found a quite upward trend in malignant brain tumors incidence rate such as Glioblastoma, Oligodendroglioma, Astrocytoma (2001 to 2010) and a stability in some other tumors such as Ependymoma. On the other hand, the same study [13] has reported an increase in only those older than 80 years of age. While in our study, we found the highest incidence rate in those aged between 30 to 59 years. In term of TGR, on the other hand, almost all the age groups showed an increase during the entire sixteen years of which the least TGR was found in those with 20 to 30 years of age. Additionally, there are reports consistent with our findings regarding an increase in the burden of primary CNS tumors for a period of 60 years but a steady rate of that from early 2010 [14]. Although we are reporting the primary malignant brain tumors only, while they have reported the overall CNS tumors and also benign brain tumors such as meningioma. Regarding the reason why such increase in trends and incidence rates of the tumors have occurred, some research suggest the advances in diagnosis and risk factor augmentation [15, 21]. We believe that since at least 20 years ago, Computed Tomography which is quite capable of diagnosing brain tumors has been always available at our center, Shiraz University of Medical Sciences as the referral center for the southwest part of the Iran; so, that could not be the reason underlying the upward trend of such tumors. On the other hand, risk factor which have been suggested as the underlying etiology of these tumors such as environmental factors including radiation, in addition to genetics, would be the main reason which needs more investigation as more studies are reporting the importance of the genetic factors related to the incidence of the brain tumors [4, 24-26]. It is important to be mentioned that, in this study we have reported the malignant brain tumors only and we have investigate the incidence rate and trend of such tumors. Investigating all the brain tumors including benign ones such as meningioma and also all the brain tumors such as metastatic in addition to primary ones may lead to a report different from what we are reporting which of course need of such an investigation is sensible. What we are reporting, is showing an alarm and bringing up a serious question whether an outbreak in malignant brain tumors especially glioblastoma as the most lethal one is happening or not? Additionally there are reports and evidence that non-ionizing radiofrequency radiation could lead to brain tumors such as Schwannomas and malignant gliomas [27, 28]. Recently the exposure to this type of radiation has increased considering the more use of mobile phones and expansion of telecommunication towers. Also the radiofrequency radiation used to noise in TV networks should not also be forgotten. So the question is, acting as a radiofrequency non-ionizing radiation, and based on the amount of the radiation applied, could it such these noises applied to International TY networks, be a possible reason for such an increase in the brain tumors in Fars province of Iran? Another important factor is the regional environmental changes that have affected the climate in southern Iran and Iraq such as air prolusion, warming and increased use of toxins in food industry. Answering such questions needs further investigation on malignant brain tumor trends in other provenance of Iran and also in neighboring contraries. Also access to the accurate information regarding the level of these radiofrequency noises can be helpful.
References
- Reynoso-Noverón N, Mohar-Betancourt A, Ortiz-Rafael J. Epidemiology of Brain Tumors. In: Monroy-Sosa A, Chakravarthi SS, de la Garza-Salazar JG, Meneses Garcia A, Kassam AB, editors. Principles of Neuro-Oncology: Brain & Skull Base. Cham: Springer International Publishing 12 (2021): 15-25.
- Louis DN, Ohgaki H, Wiestler OD, et al. The 2007 WHO classification of tumours of the central nervous system. Acta neuropathologica 114 (2007): 97-109.
- Nakazato Y. [Revised WHO classification of brain tumours]. Brain and nerve = Shinkei kenkyu no shinpo. 60 (2008): 59-77.
- Wiemels J, Wrensch M, Claus EB. Epidemiology and etiology of meningioma. J Neurooncol 99 (2010): 307-314.
- Ostrom QT, Adel Fahmideh M, Cote DJ, et al. Risk factors for childhood and adult primary brain tumors. Neuro-oncology 21 (2019): 1357-1375.
- Soomro SH, Ting LR, Qing YY, et al. Molecular biology of glioblastoma: Classification and mutational locations. JPMA The Journal of the Pakistan Medical Association 67 (2017): 1410-1414.
- Butowski NA. Epidemiology and diagnosis of brain tumors. Continuum (Minneapolis, Minn) 21 (2015): 301-313.
- Perkins A, Liu G. Primary Brain Tumors in Adults: Diagnosis and Treatment. American family physician 93 (2016): 211-217.
- Araghi M, Roshandel G, Hasanpour-Heidari S, et al. Incidence of Malignant Brain and Central Nervous System Tumors in Golestan, Iran, 2004-2013. Archives of Iranian medicine 23 (2020): 1-6.
- Deltour I, Johansen C, Auvinen A, et al. Time trends in brain tumor incidence rates in Denmark, Finland, Norway, and Sweden, 1974-2003. Journal of the National Cancer Institute 101 (2009): 1721-1724.
- Gittleman HR, Ostrom QT, Rouse CD, et al. Trends in central nervous system tumor incidence relative to other common cancers in adults, adolescents, and children in the United States, 2000 to 2010. Cancer 121 (2015): 102-112.
- Kalamatianos T, Kalyvas A, Komaitis S, et al. Trends in hospital stay and outcome of CNS tumor patients in Greece during the socioeconomic crisis period (2010-2018): The case of the academic neurosurgical department at Evangelismos Hospital. Surg Neurol Int 12 (2021): 211.
- Natukka T, Raitanen J, Haapasalo H, Auvinen A. Incidence trends of adult malignant brain tumors in Finland, 1990-2016. Acta oncologica (Stockholm, Sweden) 58 (2019): 990-996.
- Riano I, Bravo P, Bravo LE, et al. Incidence, Mortality, and Survival Trends of Primary CNS Tumors in Cali, Colombia, From 1962 to 2019. JCO global oncology 6 (2020): 1712-1720.
- Kucukyildiz HC. Trends on Central Nervous System Cancers in Turkey. Turkish neurosurgery 30 (2020): 527-531.
- Rosychuk RJ, Witol A, Wilson B, et al. Central nervous system (CNS) tumor trends in children in a western Canadian province: a population-based 22-year retrospective study. Journal of neurology 259 (2012): 1131-1136.
- Withrow DR, Berrington de Gonzalez A, Lam CJK, et al. Trends in Pediatric Central Nervous System Tumor Incidence in the United States, 1998-2013. Cancer epidemiology, biomarkers & prevention: A publication of the American Association for Cancer Research, cosponsored by the American Society of Preventive Oncology 28 (2019): 522-530.
- Arora RS, Alston RD, Eden TO, et al. Are reported increases in incidence of primary CNS tumours real? An analysis of longitudinal trends in England, 1979-2003. European journal of cancer (Oxford, England : 1990) 46 (2010): 1607-1616.
- Beygi S, Saadat S, Jazayeri SB, et al. Epidemiology of pediatric primary malignant central nervous system tumors in Iran: a 10 year report of National Cancer Registry. Cancer epidemiology 37 (2013): 396-401.
- Jazayeri SB, Rahimi-Movaghar V, Shokraneh F, et al. Epidemiology of primary CNS tumors in Iran: a systematic review. Asian Pacific journal of cancer prevention: APJCP 14 (2013): 3979-3985.
- Salimi A, Zali A, Seddighi AS, et al. Descriptive Epidemiology of Brain and Central Nervous System Tumours: Results from Iran National Cancer Registry, 2010-2014. J Cancer Epidemiol 12 (2020): 3534641.
- Ho VK, Reijneveld JC, Enting RH, et al. Changing incidence and improved survival of gliomas. European journal of cancer (Oxford, England: 1990) 50 (2014): 2309-2318.
- Caldarella A, Crocetti E, Paci E. Is the incidence of brain tumors really increasing? A population-based analysis from a cancer registry. Journal of Neuro-Oncology 104 (2011): 589-594.
- Reilly KM. Brain tumor susceptibility: the role of genetic factors and u ses of mouse models to unravel risk. Brain Pathol 19 (2009): 121-131.
- Schwartzbaum JA, Fisher JL, Aldape KD, et al. Epidemiology and molecular pathology of glioma. Nature Clinical Practice Neurology 2 (2006): 494-503.
- Curry RN, Glasgow SM. The Role of Neurodevelopmental pathways in brain tumors. Front Cell Dev Biol 9 (2021): 659055.
- Miller AB, Sears ME, Morgan LL, et al. Risks to Health and Well-Being From Radio-Frequency Radiation Emitted by Cell Phones and Other Wireless Devices. Frontiers in public health 7 (2019): 223.
- Morgan LL, Miller AB, Sasco A, et al. Mobile phone radiation causes brain tumors and should be classified as a probable human carcinogen (2A) (review). International journal of oncology 46 (2015): 1865-1871.
