Prevention of Unplanned Extubation in PICU: Nurse-led Quality Improvement project
Article Information
Hazel Lyn Obina RN1, Kathyrine Tayag RN2, Hammad Almohileb RRT3, Hakem Alomani MD4*
1PICU staff nurse, Maternity and children hospital, Qassim, Saudi Arabia
2PICU head nurse, Maternity and children hospital, Qassim, Saudi Arabia
3Head of respiratory department Maternity and children hospital, Qassim, Saudi Arabia
4Pediatric critical care consultant, King Faisal Specialized Hospital and Research Center (KFSHRC), Medina, Saudi Arabia
*Corresponding Author: Hakem Alomani, Pediatric critical care consultant, King Faisal Specialized Hospital and Research Center (KFSHRC), Medina, Saudi Arabia.
Received: 19 April 2023; Accepted: 25 April 2023; Published: 28 April 2023
Citation:
Hazel Lyn Obina, Kathyrine Tayag, Hammad Almohileb, Hakem Alomani. Prevention of Unplanned Extubation in PICU: Nurse-led Quality Improvement project. Journal of Pediatrics, Perinatology and Child Health. 7 (2023): 63-73.
View / Download Pdf Share at FacebookAbstract
Introduction: Unplanned extubation is a well-recognized health problem and frequent morbidity in PICU.
Method: Our SMART aim is to reduce the UPE rate to less than 1 per 100 ventilator days and sustain it for at least six months within 12 months. We chose the rate of UPE as an outcome measure. We chose Percentage of PICU staff who attended UPE training, Percentage of compliance to nurse assignment based on RAS, percentage of adherence to safety tag, Percentage of adherence to ETT fixation and completion of UPE case analysis form as process measures. We used PDSA as the main strategy to test the changes and implement multiple interventions.
Result: Over 32 months of the entire project period, we recorded 10 UPEs events. 80% of patients were one year old or less. 60% of UPEs were with uncuffed ETT, and 80% happened in the early morning between 00:00 and 12:00. 50% needed reintubation, and 80% were discharged. However, 20% died in PICU (2 patients). 3 PDSAs were rolled out during the project, and the rate of UPE decreased from 0.4 per 100 ventilation days in the year 2019 to 0.1 per 100 ventilation days in the year 2021 and was sustained for more than six months.
Conclusion: UPE can cause significant morbidity and/or mortality in PICU, and we can identify high-risk patients and the factors that contribute to such morbidity. The quality improvement project is an effective tool to decrease or prevent UPE events in PICU.
Keywords
PICU; Unplanned extubation; Accidental extubation; Patient safety; Quality improvement project; Pediatric extubation
PICU articles; Unplanned extubation articles; Accidental extubation articles; Patient safety articles; Quality improvement project articles; Pediatric extubation articles
Article Details
Abbreviations:
UPE: Unplanned Extubation; S-UPE: Self-Extubation, A-UPE: Accidental-Extubation; QIP: Quality Improvement Project; OVR: Occurrence-Variant Report System; RRT: Registered Respiratory Therapist; RN: Registered Nurse; ETT: Endotracheal Tube; PICU: Pediatric Intensive Care Unit; NICU: Neonatal Intensive Care Unit; RAS: Risk Assessment Tool; PDSA: Plan, Do, Study, Act
1. Introduction
Unplanned Extubation (UPE) is defined as unplanned removal of an Endotracheal Tube (ETT) from the patient’s trachea [1]. However, UPE can be further classified based on the underlying etiology into Self-Extubation (S-UPE) or Accidental Extubation (A-UPE), where Self-extubation means the patient's own action results in the displacement of ETT from the trachea, i.e. the patient reached the ETT and pull it out by his/her own hand. In contrast, accidental extubation means unintentional health care provider intervention that results in the displacement of ETT from the trachea without the patient's active participation, i.e. transferring the patient from bed to bed without securing or stabilizing the ETT that is resulting in extubation. It might be important to distinguish between these two types of UPE, given that each type has a different set of triggers and different solutions for root-cause analysis in each event.
In general, UPEs are considered a significant health problem and common morbidity in a Pediatric Care Unit (PICU) and Neonatal Critical Care Unit (NICU), with incidence reported from 0.14 to 6.6 per 100 ventilator days [1-3]. A large recent prospective multicenter case-control study in PICU reported a lower incidence rate with an overall incidence rate of 0.74 of unplanned extubations/100 endotracheal days; (95% CI, 0.64–0.85), however; it is worth mentioning that there was a high inter-site variation in reporting the incidence rate of UPE where rates ranged by the site from 0.3 to 2.1 unplanned extubations/100 endotracheal days [4].
UPEs are not free from harm, where around 20% of children who developed UPE had a significant cardiovascular collapse and required CPR or inotropic support [1,4,5]. Not surprisingly, about two-thirds (62%) of the patients who developed UPEs in PICU will require re-intubation, while the remaining (48%) who didn’t require re-intubation should be considered as a missed opportunity for extubation rather than successful unplanned extubation. Moreover, all patients with UPE will have a longer stay in PICU regardless of whether they need re-intubation or not [4,6]. In addition to these significant adverse events and harm of UPE, UPEs have a significant economic burden where Roddy et al. [6] found in their unique case-control study that Pediatric patients with UPEs have an associated increase in hospital costs ($36,692/case) as compared with age and diagnosis-matched controls [6].
The etiology for UPE in PICU is usually multifactorial; however, there are some risk factors that have been identified like: age of less than six years, inadequate sedation, ETT fixation method, increased secretion, time of the day (morning shift Vs. night shift), type of ETT (cuffed Vs. uncuffed), nurse experience and nurse to patient ratio [1,4]. These risk factors varied in odds ratio in the logistic regression analysis with conflicting results. However, Interestingly, nasal intubation, nurse-to-patient ratio of 1:1, and use of neuromuscular blockage have a protective effect against UPE in one of the largest multicenter analyses for risk factors of UPE in PICU [1,4].
The benchmark for UPEs has been set as <1 per 100 ventilator days, and many authors used this benchmark as a target in their quality improvement project (QIP) [7-9]. The Method for calculating UPE is usually a function of the number of UPE per 100 intubation days [10].
Disclaimer: we utilized Institute for health improvement (IHI) open school courses as a resource for the authors, while we used SQUIRE 2.0 as a guide to reporting the project [11,12].
2. Method
2.1 Context
Maternity and Children Hospital (MCH) is a 500-bedded specialized regional referral hospital in the Qassim region in Saudi Arabia. The PICU department in MCH is 7-bedded (expanded to 10 beds during the project); it’s a closed system unit with an average annual admission rate of 500 medical and surgical patients. The occupancy rate in PICU is 85%, with a Length of Stay (LOS) of 4 days. The unit is covered 24/7 by a dedicated qualified team that includes staff nurses, RRT, PICU specialists and PICU consultants. The nurse-to-patient ratio is variable based on the severity of the patient; however, overall, it is determined to be 1:1 to 1:2, all qualified PICU nurses with occasional pullout from another critical care area during surges times. RN and RRT working hours are determined to be 12 hrs. shifts.
2.2 Interventions
(A) Design:
1. Formation of the task force:
Between 2018 and 2019, we noticed a steady increase in UPE events as it is usually reported as morbidity events in the PICU department, which was zero-event prior to the project. We formulated a multi-professional team to assess and review these events and chose a nurse staff as a project champion. The team comprised of a PICU registered Staff Nurse (RN), a PICU registered Respiratory Therapist (RRT), a PICU staff physician, and a quality coordinator. We reviewed a short analysis of these events/cases (Table 1, First 5 cases).
Table 1: Analysis of patients with UPE in our unit.
In addition, all team members registered in Institute for Health Improvement (IHI) open-school free courses and completed the introductory QI courses (101, 102, 103, and 104) to equip themselves with the necessary knowledge and skills prior to starting the project.
The team answered the three questions of the model for improvement:
Aim: to decrease the UPE rate to less than 1 per 100 ventilator days and to sustain it for six months
Measures: outcome measures, process measures and balancing measures (Table 2)
Changes: a bundle of interventions (known to decrease UPE in other PICUs)
2. Process of choosing changes (interventions):
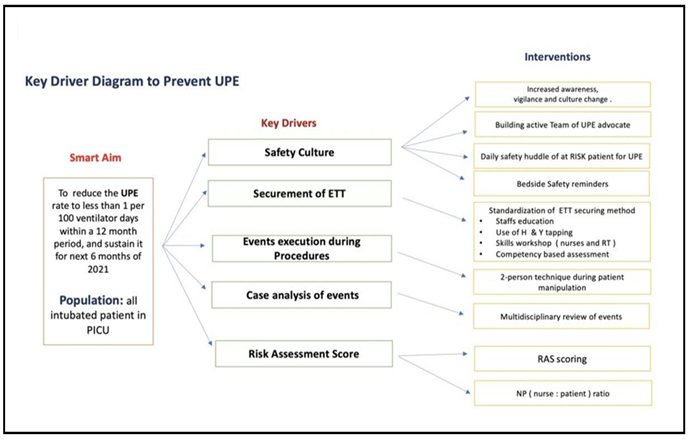
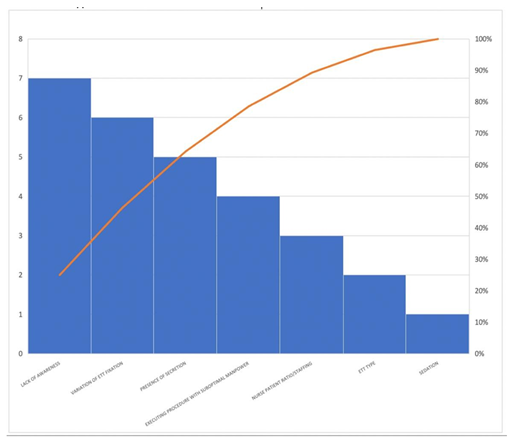
Changes (interventions) can be selected in many ways, such as process mapping, benchmarking, or creative thinking. We brainstormed and limited literature review for similar projects and devised a bundle of interventions. (Figure 1: key drivers and interventions) (Figure 4: Pareto chart for Risk factors for UPE)
|
Measure name |
Measure Type |
Nominator |
Dominator |
|
UPE rate |
outcome |
UPE events |
100 ventilator days |
|
Percentage of PICU staff attended UPE training /education |
process |
Number of staff attended UPE training/education |
Number of all PICU staff |
|
Percentage of patient assigned RAS |
process |
Number of patients with RAS score documented in chart |
Number of intubated patients |
|
Percentage of compliance to nurse assignment based on RAS |
process |
Number of correct nurse assignment |
Number of intubated patients with RAS score |
|
Percentage of compliance to ETT fixation |
process |
Number of intubated patients with correct fixation |
Number of all intubated patients |
|
UPE case analysis |
process |
Number of UPE cases with completed form filled |
Number of UPE all UPE cases |
Table 2: Measures in UPE.
3. Measures: (see Table 2)
3.1 Outcome measure:
UPE rate: we chose the rate of UPE as the outcome measure given it is the measurable aim of the study. The unit reports the UPE rate monthly as a required KPI in PICU and reportable morbidity events. However, to ensure we report all events, we incorporate UPE rate in our daily safety huddle in PICU. Our safety huddle occurs daily at 10 am with all key persons (consultant on-call, resident on call, head nurse, charge nurse and our quality coordinator who have the records) inside PICU daily.
3.2 Process measures:
- Percentage of PICU staff who attended UPE training /education: given that our initial review showed a lack of awareness contributed to the UPE events, we chose staff education and increased awareness as an intervention and we chose this measure to study the efficiency of our teaching. We conducted regular didactic lectures and workshops around the UPE (incidence, etiology, impact on patient outcomes, prevention measures) and we collected attendance for these educational activities.
- Percentage of patients assigned the Risk Assessment Score (RAS): we identified that lack of an objective risk assessment tool contributed to UPE events where we found some high-risk patients for UPE given to a novice nurse or given to experienced staff but higher patient: nurse ratio i.e. 1:3 . in order to counteract this , we adopted a known tool called RAS (see intervention description below for details) and to assess the compliance to this new risk score we planned random rounds to check all intubated patient for the presence of this score in the patient chart.
- Percentage of compliance to nurse assignment based on RAS: one of the objectives of the RAS tool is to help us link the right nurse to the right patient in the right ratio. Where patient: nurse ratio is based on the risk of UPE. For example patients with high score of RAS, will be assigned to an experienced nurse with a 1:1 ratio and low risk can be assigned 1:2 when needed. In order to monitor the compliance with this important intervention, we conducted random rounds and checked if the patient: nurse ratio for intubated patients was aligned with the RAS recommendation (see Table 3 for details for RAS recommendation)
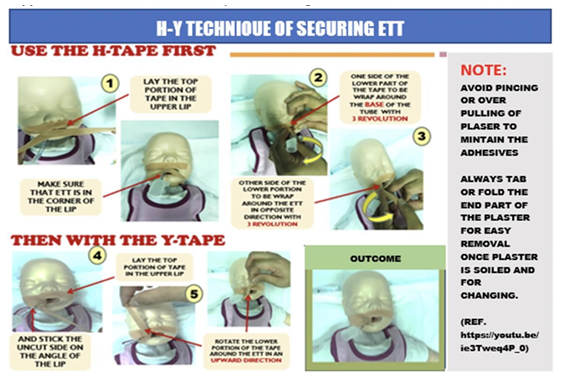
- Percentage of compliance to ETT fixation (H-Y technique): we found in our review that the variation of ETT fixation is one of the major factors that contributed to UPE events; hence we created a standard fixation method. After multiple training secessions and bedside demonstrations by our senior RT, we conduct random rounds on intubated patients and check the technique of ETT fixation to see if it’s consistent with the standard.
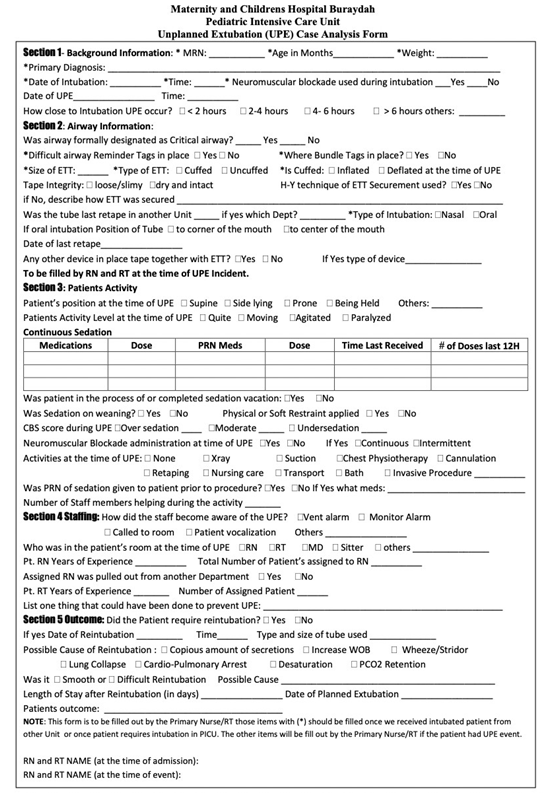
- UPE case-analysis form completion: given that there were multiple factors that contribute to UPE events and some units have different sets of factors, we created a form (see Supplement 1) to be filled by the bedside nurse immediately after the UPE event. This form captures the known factors and risks for UPE and will help us tailor our future effort to the most common factors in our unit. Furthermore, we chose this measure and conducted a review of all UPE events and reviewed the case analysis for compliance and completeness.
4. Analysis:
4.1 Figure 1: UPE Key driver diagram (KDD)
We used KDD to organize our ideas and discover various causes that contributed to UPE. The key driver breaks down the aim of our improvement project into primary and secondary drivers to help to measure and evaluate the impact of each driver:
Primary drivers are factors that are part of the system that directly impact the outcome or aim of our UPE QI effort.
Secondary drivers are opportunities to change (interventions) in our UPE QI effort. They directly impact the primary driver of our smart aim.
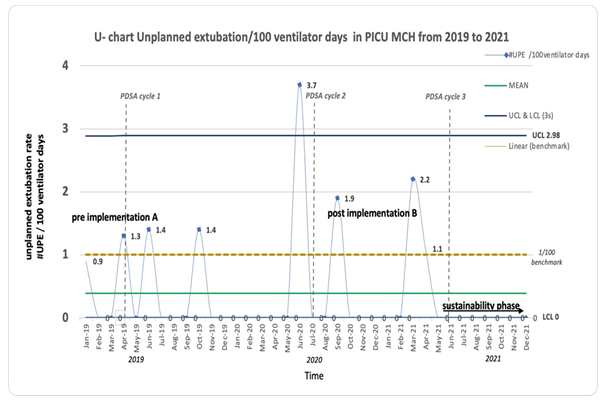
4.2 Figure 2: UPE rate on U-chart
We used the SPC statistical control chart for real-time monitoring of the unplanned extubation rate displayed on a U chart (number of unplanned extubation events per 100 ventilator days) from 1st six months 2019 baseline period until December 2021. The monthly UPE rate is depicted in a solid blue line; the Mean UPE rate is depicted in solid green color throughout 32-months study period. The blue line represents Upper and lower control limits (UCL 2.98 and LCL 0); 3 SD standard deviations above and below the mean were utilized respectively. 3 PDSA cycles were developed sequentially to sustain and achieve 0 UPE for eight months from May 2021 – December 2021. There was a relatively unequal sample size each month.
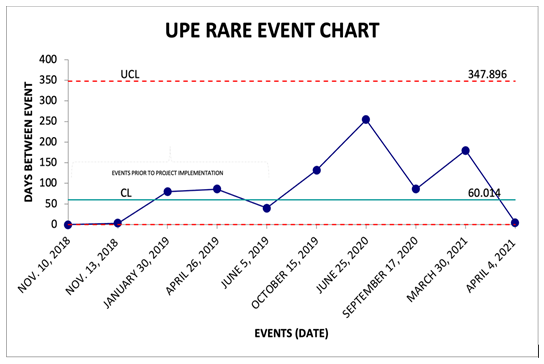
4.3 Figure 3: Days between UPE events G-Chart
We choose the G chart to represent the time between rare, occurring events as per the recommendation of a senior quality expert.
4.4 Figure 4: Pareto chart
We used the Pareto chart for a number of causes leading to unplanned extubation that occurred during the baseline period from 2018 to the first six months of 2019 (January – June) before QI project initiation. The number of UPEs is shown on the left vertical axis, and the cumulative percentage for each factor is depicted on the right axis. Lack of awareness /variation of securing ETT (patient activity at bedside, x-ray suctioning, retaping) NP ratio represents 80 % causes of UPE.
(B) Description of individual interventions:
1. Awareness and safety culture:
The team prepared a short presentation (didactic and interactive) that was conducted on several occasions for PICU staff as well as other pediatric departments through grand rounds and interdepartmental activities. The presentation focused on defining UPE as a major healthcare problem and preventable morbidity while explaining the possible system and individual factors contributing to such morbidity.
2. Standardization of ETT fixation:
We reviewed the practice of standard ETT fixation, and we adopted ( H-Y Method ) for the ETT fixation and securement (Figure 5). We conducted several hands-on workshops before implementation for all PICU staff.
3. Risk assessment system:
Based on our literature review, we identified age, low sedation level and excessive secretion, and others (Table 4) as risk factors. We adopted a risk score system (Table 3) that assigned a specific score for each intubated patient. This score resulted in a change in the nurse-to-patient ratio to mitigate the high-risk level for UPE in each patient.
|
Paediatric Intensive Care Unit UPE Risk Assessment Score Please circle the applicable point values and add to determine risk scores |
|
|
Anatomical Risk (difficult airway and facial deformity) |
6 |
|
CBS (1-deep, 2-moderate, 3-under sedation) |
1/2/3 |
|
Excessive secretion |
1 |
|
Multiple procedure & or transport |
1 |
|
Planned Extubation (extubation protocol in place) |
1 |
|
Patient in prone position |
1 |
|
Patient requires frequent retaping |
1 |
|
History of UPE |
1 |
|
Low Moderate High Extreme 2 3-4 5 >6 |
|
|
Source: Children’s Healthcare Atlanta |
|
Table 3: Risk score system (courtesy of children healthcare’s Atlanta).
|
1 |
Age less than 6 years old |
|
2 |
Inadequate sedation |
|
3 |
Excessive secretion |
|
4 |
Type of ETT (Uncuffed Tube) |
|
5 |
Variation in Method of ETT fixation |
|
6 |
Nurse-Patient Ratio |
|
7 |
Nurse pulled out from another department |
|
8 |
Bedside nurse years of experience |
Table 4: Common risk factors for UPE.
4. Bedside reminder:
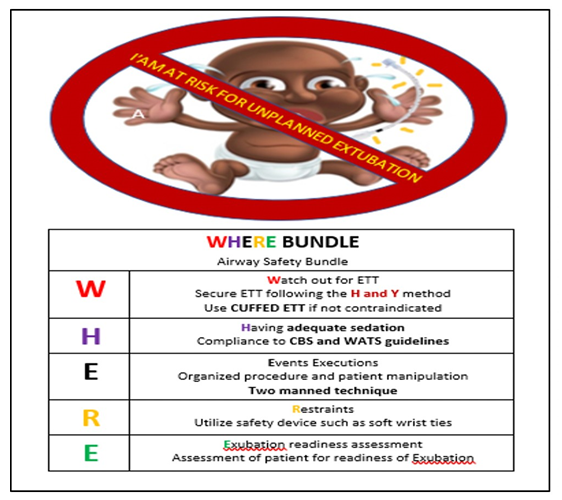
We included a visual reminder for all intubated patients called (where bundle) (Supplement 2).
5. Monitoring and reporting UPE:
We aligned our goal with the overarching goal of the quality and safety department and registered our initiative as QIP, and set it as a clinical indicator for PICU. To increase awareness and capture all events, we also utilized our event-reporting system called: Occurrence/Variance Report (OVR). We added a question about UPE in our daily safety huddle in PICU (do we have UPE in the last 24 hrs?); if yes, then two other inquiries: is it registered in the OVR system? Did we complete the UPE case analysis form?
We also added an auditing tool (to be filled randomly every month by the UPE team) to monitor the compliance of the components of the recommended initiatives to prevent UPE (see Supplement 3).
6. Database:
We established a database for UPE events with a form that was revised twice to capture the possible causes for UPE and to be filled in real-time by the bedside nurse for each UPE event and collected periodically for analysis to alert us about new trends or future areas of improvements.
7. Competency for ETT fixation:
We developed a form to test competency for ETT fixation conducted for all new staff and then every 2-3 months on intubated patients and/or mannequins to ensure competency and identify gaps in learning.
(C) Strategy to test changes (interventions):
PDSA (Plan-Do-Study-Act) methodology (total of three cycles):
PDSA-1:
(Plan): stating the question and making the prediction: will introducing the bundle decrease the UPE rate? Prediction: yes, with moderate resistance to change in culture.
We selected a bundle of 3 interventions; then we chose the Method of data collection, time frame and person responsible for data collection. WHO: the nurse educator with our RT will prepare material and equipment for staff education and training about the UPE prevention project; the project champion will collect and report the rate of UPE and training compliance. WHAT: project champion will collect the UPE rate monthly compliance/attendance of training sessions monthly. WHEN: start within one month and meet monthly to review and analyze the outcomes. (Do): We launched three interventions that included: 1- increasing awareness of UPE and promoting safety culture 2- standardized ETT fixation 3- creating bedside reminder called (where bundle). (Study): we are still having UPEs events (Figure 2), and based on the interviews with staff and observation at the bedside, we found insufficient understanding of the goals of the project among the staff as well as a lack of awareness of the available materials. (Act): to do RCA for these cases, re-educate the staff, and to adopt the previous interventions.
PDSA-2:
(Plan): stating the question and making the prediction: is the previous failure in the first PDSA is secondary to failure in change or failure in executing the change? We think it's due to suboptimal execution and suboptimal training and education. WHO: nurse educator will reinforce training education sessions, the team will create tracking sheet and form to fill by bedside nurse, WHAT: we will collect UPE rate and the detail in each event of UPE, WHEN: immediate implementation, collect UPE monthly and tracking sheet to be filled per event. (Do): RCA for events: the team interviewed the bedside nurse and reviewed possible causes in non-blame culture but with an appropriation of accountability. Nurse ratio and absence of risk classification were the most likely system factors contributing to UPE events' persistence. We started interventions which included 1- re-introduction of UPE awareness 2- incorporation of risk monitoring in nurse flow-sheet. (Study): rate of UPE remained unchanged and we had difficulty in data collection, shortage of nurses, and absence of shared understanding of high-risk patients based on the walk rounds and interviews with the staff. (Act): adopt previous interventions, revisit the literature review and introduce or modify some interventions.
PDSA-3:
(Plan)Stating the question and making the prediction: will adding an assessment risk tool and competency test decrease the rate of UPE? Prediction: yes. WHO: team will create a risk assessment tool and create competency test material. WHAT: airway risk assessment tool, competency test tool. WHEN: to implement ASAP, monitor monthly, and report to the monthly team meeting. (DO): 1-adoption of an established risk score (Table 3) and adjust patient-to-nurse ratio based on the risk assessment. 2- create a form for the UPE event to be filled by the bedside nurse in real-time for each event (replacing the tracking sheet database) (supplement 1) and 3- start competency for ETT fixation.
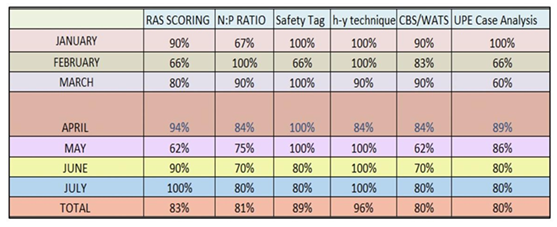
(Study): compliance of staff to (RAS scoring, H-Y taping technique, and filling the case analysis) were monitored with varying success (Figure 6 ), and the staff understanding improved based on walk rounds and interviews of bedside nurses by the taskforce members. UPE rate was zero for the last eight months (April 2021to the end of December 2021). (see Figure 2 and Figure 3: G-chart)
(Act): Adopt the interventions and implement them as a standard of care (to include them in the policy and procedure of the department)
5. Result:
We have observed 10 patients with Unplanned extubation (UPE) since we started to work on the project. Demographic data: 7 patients were one year old or less, two were > 1 year but < less than six-year, and only one was > than six years old. Regarding the type of ETT, six patients had uncuffed ETT, and the remaining cuffed ETT. In terms of the type of UPE (accidental vs. self-extubation), 6 UPEs were accidental (inappropriate handing by the staff during a procedure i.e. x-ray, changing from bed to bed post-transfer), and 4 UPEs were self-extubation (the patient themself pulled the tube out by their own hands). Regarding the need for re-intubation, five patients needed to be re-intubated while the remaining five did well on High flow O2 therapy. Regarding the time of UPEs, seven UPEs happened between 7 AM – 7 PM, and three UPEs were between 7 PM-7 AM.
Regarding the bedside nurse experience, 4 UPEs happened where the primary nurse experience was less than one year in PICU and Nurse patient ratio 1:2. In contrast, the remaining 6 happened with bedside nurse ratio of 1:1 having PICU experience > than one year. Regarding The outcome of the patients with UPEs, eight patients were discharged to their respective wards and two died in PICU (one of them was already DNR prior to the UPE event), and of note, both were accidental extubation (Table 2).
During the project and over 32 months (April-2019-December-2021), we had 20 meetings among the taskforce members. We conducted 11 formal lectures and workshops and frequent nonformal bedside discussions and reviews by the task force members. We agreed upon five measures (1 outcome and four processes) and rolled out 3 PDAs. The outcome measure was the rate of UPE and the remaining process measure were Percentage of PICU staff who attended UPE training /education, Percentage of the patient assigned RAS, Percentage of compliance to nurse assignment based on RAS, Percentage of compliance to ETT fixation. We created new forms and tools like the RAS H-Y taping technique, where Bundle and case analysis forms are to be filled with each new UPE.
The compliance to the process measures was checked randomly one or twice via an agreed-upon auditing tool. The results were averaged as follows: Percentage of PICU staff who attended UPE training /education, Percentage of the patient assigned RAS (83%), Percentage of compliance to nurse assignment based on RAS (81%), Percentage of compliance to ETT fixation (H-Y technique) was (96%) (Figure 6).
We noticed a gradual improvement in compliance with the standard of care and increased understanding and engagement of the staff for the importance of UPEs and the need to prevent them. This engagement and shared mental model resulted in the apparent decrease of the UPE rate to Zero in the last eight months of December (see Figure 2 and 3). This happened despite the expansion of beds (expanded from 7 to 10) and despite the high percentage of the new PICU staff (fresh graduate nurses joined PICU after passing the probational period) and they represent %24 of the total nurses in PICU during the project.
6. Discussion
In our project, although it took longer than expected and anticipated (32 months due to many logistic reasons as well as due to the law rate of UPEs) , we were able to decrease the UPE event rate and sustain it for six months as per our mission statement, using a bundle of interventions that included (1) education/raise awareness about UPE, (2) standardizing the ETT fixation practice, (3) utilizing risk assessment tool to identify high-risk patient/situations for UPE and (4) create monitoring and auditing system for UPE events.
Acknowledging the limitation in our study and the low number of events, the result generally points in the same direction as other large studies in terms of the risk factors and outcomes. where we found in our study the age group at risk is six years or less in age and most UPE events happened between 7 AM-7 PM, in addition most of them have uncuffed ETT [1,4]. The nurse-patient ratio and nurse experience were not apparent risk factors in our study compared with other reported risk factors. However, it might be the low event number in our study that precludes the appearance of this association [1,4].
Although it is not clearly reported in the literature around UPE in PICU, It might be prudent to differentiate between the two types of UPEs, The accidental UPE (A-UPE) vs. the Self-extubation UPE (S-UPE). The A-UPE means dislodgement of ETT caused by the health care provider’s inappropriate action during manipulation of the patient. In contrast, S-UPE means dislodgment of ETT by the action of the patient themself. Where we found that A-UPE is the most common in our study and carries the worst outcome (the two mortality in our study were A-UPE events).
We might be able to eliminate the A-UPE type with targeted strategies, but we might never be able to eliminate the S-UPE type given that the former is a result of an inappropriate process while the latter is an inevitable result of an appropriate process (weaning of sedation and active child). Examples of A-UPE in our study as well as in our short literature review included A-UPE events during the x-ray, bathing, procedure inside PICU or transporting the patient from their bed to another bed for procedure outside PICU i.e. Brain MRI. On the other hand, S-UPE -in our opinion- is an inevitable event of our progress toward liberating patients and keeping them spontaneously breathing on minimal chemical restrain, which is the current best practice.
We think that the key drivers and interventions that guided us to achieve our goal of reducing UPE rate are: the standardization of ETT fixation, using a risk assessment tool, using bedside reminders, and the focused review and analysis for each case (post-event analysis by a multi-professional team that enables us to tailor our effort to the local causes). Furthermore, this conclusion is also supported by other projects using QI methodology to reduce UPE, where they reach a similar conclusion [7].
7. Limitation:
Our study has many limitations that include a single center with few UPE events that preclude any significant statistical conclusion as well as lack of formal methods to assess the outcome of the education and the training where we used informal assessment and informal feedback from end users to produce some of the results.
8. Lesson Learned
- UPE is preventable morbidity with known risk factors (i.e. age less than one year, uncuffed ETT, variation of ETT fixation technique)
- No single intervention could reduce the UPE rate but it’s the power of bundle interventions that act collectively toward a common goal.
- UPE event that doesn’t result in reintubation is actually a missed extubation opportunity!
- The best chance for QIP to be successful is carefully choosing the champion from the frontline like nursing staff who is interested and capable otherwise imposing these excellent QIPs on uninterested or incapable staff is a setup for failure.
9. Declaration:
We declare that we collected the data via the standard process approved by our institution and all original data are available upon request. Given that this is a quality improvement project and all data used are routinely collected by our institution for all patients as well as no identifiers used, we waived the need for ethical approval or consent. No funding has been received and no competing interest is to be declared.
Acknowledgments:
We would like to acknowledge Dr. Yasser Kazzaz (Pediatric critical care consultant, KASCH, Riyadh) for his guidance and suggestion on the project design. We would also like to extend the acknowledgment to all PICU staff in MCH, Buridah and Qassim for their commitment and support of this quality improvement project.
References
- Lucas da Silva PS, de Carvalho WB. Unplanned extubation in pediatric critically ill patients: a systematic review and best practice recommendations. Pediatr Crit Care Med 11 (2010): 287-294.
- Hu X, Zhang Y, Cao Y, et al. Prevention of neonatal unplanned extubations in the neonatal intensive care unit: a best practice implementation project. JBI Database System Rev Implement Rep 15 (2017): 2789-2798.
- Silva PS, Reis ME, Aguiar VE, et al. Unplanned extubation in the neonatal ICU: a systematic review, critical appraisal, and evidence based recommendations. Respir Care 58 (2013): 1237-1245.
- Fitzgerald RK, Davis AT, Hanson SJ; National Association of Children's Hospitals and Related Institution PICU Focus Group Investigators. Multicenter Analysis of the Factors Associated With Unplanned Extubation in the PICU. Pediatr Crit Care Med 16 (2015): e217-23.
- Klugman D, Berger JT, Spaeder MC, et al. Acute harm: unplanned extubations and cardiopulmonary resuscitation in children and neonates. Intensive Care Med 39 (2013): 1333-1334.
- Roddy DJ, Spaeder MC, Pastor W, et al. Unplanned extubations in children: impact on hospital cost and length of stay. Pediatr Crit Care Med 16 (2015): 572-575.
- Kandil SB, Emerson BL, Hooper M, et al. Reducing Unplanned Extubations Across a Children's Hospital Using Quality Improvement Methods. Pediatric quality and safety 3 ((2018)): e114.
- Mehta NM, Sharma S, Laussen PC. Unplanned extubation: securing the tool of our trade. Intensive Care Med 41 (2015): 1983-1985.
- Merkel L, Beers K, Lewis MM, et al. Reducing unplanned extubations in the NICU. Pediatrics 133 (2014): e1367-e1372.
- Little LA, Koenig JC Jr, Newth CJ: Factors affecting accidental extubations in neonatal and pediatric intensive care patients. CritCare Med 18 (1990): 163-165.
- http://www.ihi.org/education/IHIOpenSchool/overview/Pages/default.aspx
- Ogrinc G, Davies L, Goodman D, et al. SQUIRE 2.0 (Standards for QUality Improvement Reporting Excellence): revised publication guidelines from a detailed consensus processBMJ Quality and Safety 25 (2016): 986-992.
Supplementary Files:
Case Analysis Form:
2. WHERE Bundle Reminder:
Compliance Auditing Form:
The Auditing Tool to Monitor Compliance:
Auditing tool for QIP: prevention of UPE:
Name of auditing person:
Date of auditing:
Time of Auditing:
For a ventilated patient no.1:
Q1: is ETT being fixed as per protocol?
Q2: Dose the patient have an assigned RAS in the nurse flowsheet?
Q3: is there a reminder at bedside (where bundle) ?
Q4: if there was UPE event, dose the form filled out by the bedside nurse?
Q5: if there was UPE event and the form filled out by the bedside nurse, is it complete?
For a ventilated patient no.2:
Q1: is ETT being fixed as per protocol?
Q2: Dose the patient have an assigned RAS in the nurse flowsheet?
Q3: is there a reminder at bedside (where bundle ?
Q4: if there was UPE event, dose the form filled out by the bedside nurse?
Q5: if there was UPE event and the form filled out by the bedside nurse, is it complete?
For a ventilated patient no.3:
Q1: is ETT being fixed as per protocol?
Q2: Dose the patient have an assigned RAS in the nurse flowsheet?
Q3: is there a reminder at bedside (where bundle ?
Q4: if there was UPE event, dose the form filled out by the bedside nurse?
Q5: if there was UPE event and the form filled out by the bedside nurse, is it complete?
For a ventilated patient no.4:
Q1: is ETT being fixed as per protocol?
Q2: Dose the patient have an assigned RAS in the nurse flowsheet? Q3: is there a reminder at bedside (where bundle ?
Q4: if there was UPE event, dose the form filled out by the bedside nurse?
Q5: if there was UPE event and the form filled out by the bedside nurse, is it complete?
For a ventilated patient no.5:
Q1: is ETT being fixed as per protocol?
Q2: Dose the patient have an assigned RAS in the nurse flowsheet?
Q3: is there a reminder at bedside (where bundle?
Q4: if there was UPE event, dose the form filled out by the bedside nurse?
Q5: if there was UPE event and the form filled out by the bedside nurse, is it complete?