Prevalence of Intestinal Tuberculosis in cases of acute abdomen-A study of 100 cases
Article Information
Md. Nashir Uddin1*, Tariq Akhtar Khan2, Probin Kumar Mahato3, Tarik Alam Ony4, Mehfujul Hasan5, Mohammad Haroon Or-Rashid6, Mahmud Zaman Chowdhury7, Fahim Hossain8, Anjuman Sultana9
1Department of Surgery, Mugda Medical College, Hospital, Dhaka, Bangladesh.
2Department of Colorectal Surgery, Mugda Medical, College, Dhaka, Bangladesh.
3Department of Surgery, Shaheed M Monsur Ali, Medical College Hospital, Sirajganj, Bangladesh.
4Department of Surgery, Mackay Base Hospital, Mackay, Queensland, Australia.
5Department of Surgery, Dhaka Medical College, Hospital, Dhaka, Bangladesh.
6Department of Surgery, Dhaka Medical College, Hospital, Dhaka, Bangladesh.
7Department of Surgery, Mugda Medical College, Hospital, Dhaka, Bangladesh.
8Department of Orthopedics, Mugda Medical, College Hospital, Dhaka, Bangladesh.
9Department of Obstetrics and Gynaecology, Mugda, Medical College Hospital, Dhaka, Bangladesh.
*Corresponding Author: Md. Nashir Uddin, Department of Surgery, Mugda Medical College Hospital, Dhaka, Bangladesh.
Received: 29 January 2025; Accepted: 03 February 2025; Published: 11 February 2025
Citation: Md. Nashir Uddin, Tariq Akhtar Khan, Probin Kumar Mahato, Tarik Alam Ony, Mehfujul Hasan, Mohammad Haroon Or-Rashid, Mahmud Zaman Chowdhury, Fahim Hossain, Anjuman Sultana. Prevalence of Intestinal Tuberculosis in cases of acute abdomen-A study of 100 cases. Journal of Surgery and Research. 8 (2025): 65-71.
View / Download Pdf Share at FacebookAbstract
Background: Intestinal tuberculosis (TB) is a form of extrapulmonary TB presenting as acute abdomen, caused by Mycobacterium tuberculosis infecting the gastrointestinal tract. It often leads to complications like perforation or obstruction, requiring surgical intervention. Diagnosis is challenging due to nonspecific symptoms, causing delays and increased morbidity. Awareness of intestinal TB in acute abdomen cases is crucial for timely diagnosis and management, improving outcomes.
Objectives: To determine the prevalence of Intestinal Tuberculosis in cases of acute abdomen with its various clinical presentation and treatment modalities.
Materials and methods: This cross-sectional observational study was conducted in the surgery in-patient department of Dhaka Medical College Hospital from January to June 2014. A total of 100 patients aged 11 to 80 years, of both sexes, were included. Patients with a history of trauma or children were excluded. Data on presentation, operative findings, procedures, outcomes, and histopathology were recorded and analyzed.
Results: Amongst the 100 patients with acute abdomen due to intestinal cause, 16 patients (16%) had intestinal tuberculosis on the basis of operative findings and histopathological reports. Age of the patients ranged between 16 to 80 years. Majority (70%) of the patients were seen between 20 to 40 years. Male female ratio of intestinal tuberculosis is 1:0.45. Six patients (37.5%) had evidence of pulmonary tuberculosis as well on chest X- ray and history. The commonest operative findings were ileal perforation in 50% patients, stricture constitute 25%. The common operation performed was loop ileostomy in about 56.25% patients. Patients presented with acute abdomen due to intestinal cause, post operative complications developed 37.5% in tubercular patients in contrast to non-TB patients and which is 25%. The overall mortality rate of acute abdomen was in my study is 6% but in cases of tubercular patients it was 0%.
Conclusion: Intestinal Tuberculosis is a common problem presenting to general surgical unit in the developing countries, often in an acute form. A high index of suspicion, proper evaluation and therapeutic trial in suspected patients is essential for an early diagnosis, in order to minimize complications.
Keywords
Intestinal Tuberculosis, Acute Abdomen, Intestinal Obstruction, Peritonitis
Article Details
Introduction
Tuberculosis is a global disease and is associated with deprivation, poverty, overcrowding, illiteracy and limited access to healthcare facilities. Tuberculosis can involve the entire gastrointestinal tract including peritoneum, pancreaticobillary system, mesenteric lymph nodes and spleen and abdomen is one of the common sites of involvement after lung [1,2].
The most common site for intestinal tuberculosis is seen in ileocecal segment3 and more commonly between 25-45 years of age. Associated colonic involvement is frequent and isolated colonic involvement is not uncommon. Colonic TB may be focal or multifocal and malabsorption syndrome may be seen in ileocecal TB. This disease can mimic various gastrointestinal disorder, particularly inflammatory bowel disease, colonic malignancy or other gastrointestinal infection. Tuberculosis of the appendix is rare and patient may present as acute appendicitis [3].
Intestinal tuberculosis is still highly prevalent in developing countries. The diagnosis of intestinal tuberculosis still passes through some confusing protocol due to several reasons- vague and non-specific clinical features or low yield of mycobacterium culture or smear. Moreover, surgery is often required if the diagnosis is uncertain and for obtaining tissue for histopathological examination or culture [4,5].
Abdominal tuberculosis has also become pertinent at this stage in order to determine the role of a number of newer diagnostic techniques which is now supplement of the traditional methods. Endoscopic visualization, imaging techniques using sonography, CT or MRI and advances in bacteriology and immunology have resulted in profound changes in the management of abdominal tuberculosis. Diagnosis is usually made laparoscopically or exploration of abdomen. Despite advances in drug therapy and diagnostic facilities, tuberculosis remains a major health problem in developing countries. Investigations like Imaging (ultrasound, barium X-Rays, CT scan) and Mantoux test have only supportive value. The Gene Xpert system has sensitivity 67% specificity 98% but not easily available [6]. Therefore, diagnosis of abdominal tuberculosis is an ongoing challenge to the physicians, especially with limited resources. The aim of this study was to examines the prevalence and clinical significance of tuberculosis in patients presenting with acute abdomen due to intestinal causes.
Objectives
The objective of this study was to determine the prevalence of TB in patients presenting with acute abdomen due to intestinal causes.
Methodology and Materials
This cross-sectional observational study was conducted in the Department of Surgery at Dhaka Medical College and Hospital, Dhaka, Bangladesh, from January 2014 to June 2014.
Inclusion criteria:
- • All those patients who were clinically suspected to have acute abdominal condition due to acute intestinal cause.
- • Patients who were interested to participate in the study
Exclusion criteria
- • Children will be excluded (less than 16 years)
- • Acute abdomen other than intestinal cause.
- • Patients who were not interested to participate in the study
A total of 100 patients admitted in the surgery in-patient department with clinical diagnosis of acute abdomen. Patients were mostly admitted through emergency department and outdoor. Some of the patients were referred and shifted from other units and hospital. All patients were initially resuscitated by: correction of fluid and electrolytes imbalance, insertion of nasogastric tube, broad spectrum antibiotics and analgesics and patients presenting in a critical condition were managed accordingly. After initial optimization and anesthetist’s opinion, the patients were operated. Final diagnosis and post operative treatment were dependent on the operative findings and histopathological confirmation. Some patients were improved on conservative treatment and went for definitive treatment after proper investigations. Those found to be tuberculous were started on anti-tuberculosis therapy.
Statistical Analysis: All data were recorded systematically in preformed data collection form and quantitative data was expressed as mean and standard deviation and qualitative data was expressed as frequency distribution and percentage. Statistical analysis was carried out by using Statistical analysis was done by using SPSS (Statistical Package for Social Science) Version 22 for windows 10. Ethical approval regarding the study was obtained from the institutional ethical review committee.
Result
|
Characteristics |
Number |
Percentage % |
|
Age Group |
||
|
16-20 years |
10 |
10 |
|
21-30 years |
35 |
35 |
|
31-40 years |
22 |
22 |
|
41-50 years |
18 |
18 |
|
51-60 years |
10 |
10 |
|
61-70 years |
4 |
4 |
|
>70 years |
1 |
1 |
|
Sex |
||
|
Male |
64 |
64 |
|
Female |
36 |
36 |
Table 1: Demographic characteristics of patients with Acute Abdomen
Table 1 shows their ages ranged from 16 to 80 years. Majority of the patient were seen between 21 to 40 years of age and it is about 57%. About 10% patient is found between the age of 51-60 years. Males comprised the majority of participants (64%), while females accounted for 36% and the male to female sex ratio being 1:0.56.
Figure 1 shows out of 100 cases, 40 patients had Acute Intestinal Obstruction and 60 patients presented with diffuse or localized Peritonitis, on the basis of clinical examination and radiological findings.
|
Cause |
No. |
Percentage (%) |
|
Ileal perforation |
18 |
18% |
|
Appendicular perforation/acute appendicitis |
17 |
17% |
|
Duodenal perforation |
12 |
12% |
|
Gastric perforation |
6 |
6% |
|
Post operative adhesions |
8 |
8% |
|
Obstructed inguinal hernia |
8 |
8% |
|
Colorectal growth |
5 |
5% |
|
Ileocecal mass |
5 |
5% |
|
Intestinal stricture |
4 |
4% |
|
Plastic peritonitis |
0 |
0% |
|
Sigmoid volvulus |
9 |
9% |
|
Miscellaneous |
8 |
8% |
Table 2: Causes of Acute Abdomen based on operative findings and investigations.
Table 2 shows that 18 patients (18%) were found were ileal perforation, 12 patients (12%) were DU ulcer perforation, 17 patients (17%) were acute appendicitis or appendicular perforation of burst appendix, 9 patients (9%) were sigmoid volvolus only 5 patients (5%) had illeocaecal mass and only 4 patients (4%) had intestinal stricture single or multiple. Other operative findings include –colorectal growth, post operative adhesions, obstructed inguinal hernia, bands and adhesions etc. Duodenal and gastric perforations followed by adhesions were also common.
Figure 2 shows amongst all the cases of acute abdomen, 16 patients had intestinal tuberculosis on the basis of operative findings and histopathological reports. Majority belonged to the poor socioeconomic status.
|
Variables |
Number of cases |
Percentage (%) |
|
Operative finding |
||
|
Ileocecal TB/Mass |
3 |
18.75 |
|
Single ileal perforation |
6 |
37.5 |
|
Multiple ileal perforation |
2 |
12.5 |
|
Single stricture |
2 |
12.5 |
|
Multiple stricture |
2 |
12.5 |
|
Frozen abdomen |
0 |
0 |
|
Tubercular peritonitis |
1 |
6.25 |
|
Surgical procedures |
||
|
Ileostomy |
9 |
56.25 |
|
Small bowel resection |
4 |
25 |
|
Right hemicolectomy |
2 |
12.5 |
|
Stricturoplasty |
0 |
0 |
|
Laparoscopy and biopsy |
1 |
6.25 |
Table 3: Operative finding and Surgical procedures of intestinal TB cases (n=16).
Table 3 shows that operative finding and Surgical procedures of intestinal TB cases. Operative findings revealed that single ileal perforation was the most common, observed in 6 patients (37.50%) had single ileal perforation. 3 patients (18.75%) had illeocaecal tuberculosis. The frequency of multiple ileal perforation, single and multiple strictures were equal and that is 12.50%. One patient found with tubercular peritonitis. No patient of Frozen abdomen found in this series. Regarding surgical procedures, ileostomy was the most performed intervention, conducted in 9 patients (56.25%). Small bowel resection was required in 4 cases (25%), while right hemicolectomy was carried out in 2 patients (12.5%). Stricturoplasty was not performed in any case, as resection and anastomosis with ileostomy were preferred. Laparoscopy, biopsy, and partial adhesiolysis were performed in 1 patient (6.25%).
|
Complications |
Number of cases |
Percentage (%) |
|
Complications of all patients |
||
|
Leakage with wound sepsis |
10 |
11.90% |
|
Wound dehiscence |
2 |
2.38% |
|
Intra-abdominal abscess |
2 |
2.38% |
|
Septicemia |
3 |
3.57% |
|
Chest complication |
4 |
4.76% |
|
Non complication |
63 |
75 |
|
Complication in TB patients (n=16) |
||
|
Leakage with wound sepsis |
3 |
18.75% |
|
Intra-abdominal abscess |
0 |
0% |
|
Septicemia |
0 |
0% |
|
Chest complication |
3 |
18.75% |
Table 4: Overall complications (n=84).
Table 4 shows that overall complications. Among all patients, complications were observed in 25% of cases, with leakage and wound sepsis being the most frequent, affecting 10 patients (11.9%). Other complications included chest issues in 4 patients (4.76%), septicemia in 3 patients (3.57%), wound dehiscence and intra-abdominal abscess in 2 patients each (2.38%). However, 63 patients (75%) had no complications. In the subset of 16 tuberculosis (TB) patients, complications were more pronounced, with leakage and wound sepsis, as well as chest complications, each occurring in 3 cases (18.75%). Notably, intra-abdominal abscess and septicemia were not reported among TB patients, reflecting variations in complication patterns between the general and TB-specific groups.
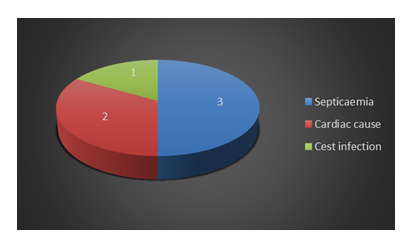
Figure 3 shows that Cause of death in cases of acute abdomen due to intestinal cause. Six patients (6%) died in this series out of 100 cases and the mortality rate is 6%. Out of this, three patients died of septicaemia because of late presentation with perforation with peritonitis and faecal contamination (two in this group died within 48 hours postoperatively), two of them died of the cardiac problem, and one due to severe chest infection.
Discussion
Tuberculosis intestinal tuberculosis affects elsewhere in the body and young people at the peak of their productive life, this fact has serious impacts on the national economy and production, as working and productive class of community is replaced by sick and ill individuals. Seventy percentages (70%) of the patients in my study were below 40 years and 48 of the were between 20-40 years and mean age is 33.40 with14.86 standard deviation., This is agreed with the result of other studies [5-10]. The male and female ratio in cases of acute abdomen due to intestinal cause is 1:0.56 which is more or less same as the study carried by Muhammad Saleem Shaikh et al. and Gamal G Shimy at al. [7,8] but opposed by the study by F. M. Sanai et al which is 1:1.8 [10]. Amongst 100 cases 18 cases (18%) presented with ileal perforation. 17 cases (17%) presented with appendicular perforation. 12 cases (12%) were duodenal perforation and 6 cases (6%) were gastric ulcer perforation. Another most important cause of acute abdomen is sigmoid volvulus of which nine cases (9%) were found in cases of acute abdomen. Other common cause include- post operative adhesions, colorectal growth, Ileocecal mass, intestinal mass. This corresponds most of the studies. Another study carried by Muhammad Saleem Shaikh et. al. [7] shows cause of acute abdomen-18.5% cases were illeal perforation, 17% cases were appendicular perforation, 12.5% cases were duodenal perforation, 6.5% cases were gastric perforation. Other common findings include- post operative adhesions, sigmoid volvulus, colorectal growth, intestinal strictures, ileocecal mass. Amongst 16 patients, six (37.5%) were associated with pulmonary tuberculosis on X-ray chest. Boukthir S et al. [11] shows association of abdominal tuberculosis with pulmonary tuberculosis is 37%. This incidence is showed 23% in Bangladesh by SM Hossain et. al. [12] and 21% by Tariq et. al. [13] and other authors quote figures of 7% and 40% in this regard [12,14]. 89% of total patients of acute abdomen were admitted through emergency and rest were referred from another unit. More than 90% of patient belongs to poor socio-economic conditions which corresponds most of the studies. In this study, the presenting symptoms included- all of the patients presented with abdominal pain (100%), eighty-one (81%) patients presented with abdominal distension, 66% patients presented with constipation and 56% patients with vomiting. This corresponds to the study by Muhammad Sal et. al, Gamal G. Shimy et al. and SM Hossain et. al and other studies as well [7,8,12]. Other manifestations which is variable in patients as weight loss (21%), fever (55%), diarrhea (16%), anorexia etc. On clinical examination all of the patients had abdominal tenderness on superficial palpation. Eighty-one patients had abdominal distension, fifty patients (50%) had muscle guarding and rigidity, thirty-nine patients (39%) had ascites. 51% patients had no bowel sound, only 4 patients (4%) presented with abdominal mass in this series. This is agreed in most of the studies. In our study, out of 100 cases of acute abdomen, the prevalence of intestinal tuberculosis is in 16 cases and percentage is 16% which is more or less equal to the study carried by Muhammad Sal et al. 12 In October 2013 a study carried at Al-Azhar University by Gamal G. Shimy et al [8] in which the incidence of intestinal tuberculosis in cases of acute abdomen is 15.5%. In Bangladesh one study was carried out by Hamida Khanom et al. at Shyamoli Chest Clinic in 2012. There she showed the incidence of extra pulmonary TB in Bangladesh is 25.51% and the incidence in case of intestinal tuberculosis is 12% [15]. Another study by Muhammad Tariq Abdullah et al done at Pakistan in 2011 there he showed prevalence of abdominal tuberculosis in cases of acute abdomen is 8% [13]. The male female ratio of intestinal tuberculosis in this study is 1:0.45, which is same as study carried by Muhammad Saleem Shaikh et al. [7] and seems to be same with Gamal G Shimy et al. and S.M. Hossain et. al which is 1:0.8 and 1:0.62 respectively [8,12] and opposed to other series which report slight female predominance [1,16]. This is due to deficiency of nutrition, negligence and poor hygienic condition and variable to country to country. In Bangladesh it is seems to be of slight male predominance [15]. In cases of peritoneal tuberculosis F.M Sanai et. al shows male and female are equally affected.17 Diagnosis of intestinal tuberculosis is challenging even in highly endemic areas like this study, the accuracy of clinical presentation is only 50%. No investigation except histopathology can reliably diagnose this disease. Nonspecific clinical picture, radiology, laboratory, endoscopic investigation and operative findings can be misleading the diagnosis of tuberculosis as many diseases has the same picture as Ileo-cecal malignancy, Chron's disease or intestinal tumors like extra nodal MALT. As we agree with many other studies in that only sure diagnosis is histopathological examination to avoid the dilemma of clinical presentation and nonspecific investigation. Out of 16 cases of intestinal tuberculosis nine patients (56.25%) presented with peritonitis and seven patients (43.75%) presented with acute or subacute intestinal obstruction. This does not correspond with other studies. Muhammad Saleem Shaikh et. al showed percentage of intestinal obstruction is high and that is 68.75% and Gamal G Shimy et. al. showed incidence of peritonitis in cases of intestinal tuberculosis is 31.5% [7,8]. On the other hand Shabana Jamal et.al showed more or less same percentage (68.2%) patients presented with peritonitis [18]. In our study, the pathological findings in tuberculous patients are ileocecal tuberculosis with intestinal perforation- single ileal perforation six cases (37.5%) and multiple ileal perforation two cases (12.5%) thus constitute of 50% of total tuberculous cases. Other findings are ileocecal TB three (18.75%) cases single or multiple stricture 2 cases (12.5%) respectively. Thus, stricture constitutes 25% of total tuberculous cases. One case of tuberculous peritonitis found (6.25) and no case of frozen abdomen or plastic peritonitis found. So, in my study ileal perforation and stricture are the commonest findings. On the other hand, Muhammad Saleem Shaikh et. al showed Hyperplastic ileocecal tuberculosis followed by intestinal stricture was the commonest operative findings and that was 34.3% and single or multiple perforations was the second most common findings that is 25%. In that study 12.5% cases were frozen abdomen. This some extend differ to my study [7].. Another study by Gamal G Shimy et al showed 28.5% patient presented with intestinal obstruction and patients presented with single or multiple perforations constitute 28.8% this has to some extent similarity to my study. In that study 14.2% cases were found frozen abdomen [8].
Another study by Shabana Jamal et al showed 68.2% patients presented with intestinal perforation, 20% patients presented with intestinal strictures and 9.1% patients presented with ileocecal mass. This is more or less similar to my my study [18]. In my study the tuberculous abdomen managed by mostly ileostomy and through peritoneal toileting and it is 10 cases (62.50%) as most of the patients presented with single or multiple ileal perforation. Four patients (25%) are needed small bowel resection and end to end anastomosis due to their late presentation and right hemicolectomy was done in two patients (12.5%) as they had preoperative diagnosis and had presented with subacute intestinal obstruction. Laparoscopy and to some extend of adhesiolysis and biopsy was taken from one patient. Another study by Gamal G Shimy et al showed 28.5% cases were planned for small bowel resection, right hemicolectomy was done on 35.7% patients. Ileostomy done on only 21.4% patients and only in cases of 14.2% patients stricturoplasty was done but in my study none of the patients, stricturoplasty was done. In that cases resection and anastomosis was planned [8]. Another study by Shaikh et al. showed – various surgical procedures performed were right hemicolectomy in 31.25% patients, followed by segmental resection and anastomosis [7]. In Bangladesh S. M. Hossain et al. showed 25% patients underwent loop ileostomy, 12.5% patients underwent right hemicolectomy, 18.75% patients was planned for adhesiolysis and biopsy and closure of perforation was done on 18.75% of patients [12]. Another study done by Hadzi-Bojan et al in Serbia in 2008 showed incidence of laparotomy in intestinal tuberculosis is as high as 25-75% [16].
Anti tubercular therapy was started was prescribed all of the patient post operatively. Post operative complications are related to the severity and extend of the disease, the most important factor is the perforation of the intestine and contamination of the peritoneal cavity. In my study thirty patients (30%) of 100 cases developed complication. Amongst 16 cases of intestinal tuberculosis 6 patients (37.5%) developed complications. So postoperative complications of tuberculous patients were high than general cases. Gamal G Shimy et al. showed 57.14% cases of intestinal tuberculosis developed post operative complication where as 32% of total cases of acute abdomen developed post operative complications [8]. More over Muhammad Saleem Shaikh et al showed 32% of postoperative complication over all cases of acute abdomen [7]. Another study done by Hadzi-Bojan et al in Serbia in 2008 showed After laparotomy a surgery is usually mandatory due to complication like intestinal occlusions in 15-60% of cases, perforation upwards from stenosis site found in 1-15% cases, abscess or fistula in present in 2-30% cases and hemorrhage found in 2% cases [16]. Another study by Shabana Jamal et al. showed 50% cases developed wound infection, 16% cases developed wound dehiscence, 13% cases developed chest infection.18 Gamal G Shimy et al. showed 14.2% cases developed wound sepsis, 14.2% cases developed chest infection, 14.2% cases developed septicemia, intra-abdominal abscess and enterocutaneous fistula developed in 14.2% cases [8]. Muhammad Saleem Shaikh et al. showed 13% patients developed wound infection and 6% patients developed chest complication [7]. In our study, six patients developed post operative complications. Out of sixteen patients three patients (18.75%) patients developed wound leakage with wound sepsis and three (18.75%) patients developed chest complication. So, this corresponds to above mentioned studies [7,8,18]. None of the patient developed wound sepsis, intra-abdominal abscess or septicemia. So most common post operative complications are- chest infection, enterocutaneous fistula, wound infection, wound sepsis, burst abdomen and septicemia. In my study 37.5% cases of intestinal tuberculosis developed post operative complication where as 28.75% cases of acute abdomen but non-TB cases developed post operative complication.
In my study six patients (6%) out of 100 cases died in this series so overall mortality rate is 6% in cases of acute abdomen which corresponds to Muhammad Saleem Shaikh et. al. [7] and Muhammad Tariq et al. [13] shows mortality rate of overall acute abdomen is 10%. Amongst of sixteen cases of intestinal tuberculosis no one died. So, mortality rate in my study is 0%. This corresponds to the study done by Baluck et al has zero mortality [19]. Khan MR et al. showed in case of abdominal tuberculosis mortality rate is 5.9%. CSJ Probert et al showed mortality rate is 4.67% [20]. In past emergency surgery in Bhansali's in 1977 experience carried 23% mortality [21] but in a recent experience, Sircar et al reported 11% of mortality rate [22]. In Bangladesh one study carried out by SM Hossain et al showed mortality rate is 15.38% [12]. Again in recent study by Shabana Jamal et al. and she showed mortality rate is 4% of abdominal tuberculosis [18]. Another study by Gamal G Shimy et al. showed mortality rate is 14.29% [8]. So different studies consider mortality rate associated with gut perforation ranging 11-45%. Patients, who are diagnosed and operated in time have a good outcome and response to anti tuberculous therapy is satisfactory. Effort has to be given on screening and identification of population at risk affected by this infectious but preventable disease.
Limitations of the study
Our study was a single centre study. The sample size was relatively small. Duration of the study was short. The long-term complications of the operative procedures could not be assessed. Only important post operative complications were observed. Only four operative procedures were used in the present study apart from the advanced procedure due to lack of technological support. Errors in histopathological reports and biopsy taking.
Conclusion
This study shows primary causes of acute abdomen identified through operative findings and investigations were ileal perforation, appendicular perforation/acute appendicitis, and duodenal perforation, indicating a diverse range of etiologies. In patients with abdominal tuberculosis, single ileal perforation was the most frequent operative finding, emphasizing the critical nature of this condition. Surgical interventions were primarily ileostomy and small bowel resection, reflecting the need for aggressive management of complex intestinal tuberculosis cases. The overall complication rate among all patients was significant, with wound sepsis being the most common complication. Notably, the complication rate was higher in patients with tuberculosis. Further study must be needed combining large sample size and more time need to determine the prevalence of this disease and long-term complications. Adequate financial support is also needed. The challenge could be the use of advanced procedure such as-Gene Xpert from ascitic fluid preoperatively collected and diagnosed, if advanced technological support is available then the result may be better. As the diagnosis of Intestinal tuberculosis in cases of acute abdomen is due to intestinal cause, solely depends on histopathological reports so all the errors regarding this should be corrected.
Acknowledgment
I would like to extend my heartfelt appreciation for the invaluable support and collaboration from the staff, participants, and my co-authors/colleagues who contributed to this study.
Financial support and sponsorship
No funding sources.
Conflicts of interest
There are no conflicts of interest.
References
- Khan MR, Khan IR, Pal KNM. Diagnostic issues in Abdominal Tuberculosis. J Pak Med Assoc 51 (2001): 138-140.
- Sharma MP, Bhatia V. Abdominal tuberculosis. Indian J Med Res 120 (2004): 305-315.
- Rita S. Diagnosis of Abdominal Tuberculosis, Role of Imaging. J Ind Acad Clin Med 2 (2001): 103-104.
- Gerard D. Current Diagnosis and Treatment-Surgery.13th ed. McGraw-Hill Lange (2010): 638.
- Gondal KM, Khan AFA. Changing Pattern of Abdominal Tuberculosis. Pak J Surg 11 (1995): 109-113.
- Steingart KR, Sohn H, Schiller I, et al. Xpert® MTB/RIF assay for pulmonary tuberculosis and rifampicin resistance in adults. Cochrane Database of Systematic Reviews (2013): CD009593.
- Shaikh MS, Kheo R Dholia, Muhammad AJ, et al. Prevalence of intestinal Tuberculosis in cases of acute abdomen. Pakistan Journal of Surgery 23 (2007): 52-56.
- Gamal G, Shimy, Marwan MB, et al. Incidence of Tuberculosis in Acute Abdomen in Endemic Area 10 (2013): 1-15.
- Muneef MA, Manish Z, et al. Tuberculosis in belly, a review of 46 cases. Scand J Gastroenterology 36 (2001): 528-32.
- Muhammad TA, Asma H. SH Waqar M, et al. Presentation and outcome of Abdominal Tuberculosis in a Tertiary Care Hospital Unit. Ann. Pak. Ints. Med. Sci 7 (2001): 337-141.
- Boukthir S, Murad SM, et al. Abdominal Tuberculosis in children. Acta Gastroenterol Belg 67 (2004): 245-249.
- SM Hossain, MM Rahman SA Hossain, et al. Mode of presentation of abdominal Tuberculosis. Bang Med J 45 (2012): 3-5.
- Tariq NA. Abdominal TB: The Surgical audit of its presentation. Pak J Surg 9 (1993): 82-86.
- Sultan M. Incidence of Intestinal Tuberculosis in patients presenting as acute emergency with sign of obstruction/ peritonitis. Journal of College of Physicians and Surgeons Pakistan 7 (1990): 38-44.
- Hamida K, Rumana S, Ripon Ch. Dhor. Diagnosis of Tuberculosis and Risk Factor Involved. Bangladesh J. Zool 40 (2012): 213-220.
- Hadzi-Bonjan Marjanovie. Abdominal Localization of TB and Role of Surgery. Medicine and Biology 15 (2008): 51-55.
- Sanai FM, Bzeiz KI. Tubercular Peritonitis- Presenting Feature, Diagnostic Strategies and Treatment. Aliment Pharmacol Therapy 22 (2005): 685-700.
- Shabana J, Zainab MK. Presentation and outcome of Abdominal Tuberculosis in a Tertiary Care Hospital Unit. Ann. Pak. Ints. Med. Sci 7 (2001): 33-36.
- Baluck N, Tufail M, Durani K, et al. Abdominal tuberculosis: A varied presentation. Pak J Surg 9 (1993): 8-12
- CSJ Probert, V Jayanthi, AC Wicks et al. Epidemiological study of Abdominal Tuberculosis among Indian Migrants and the Indigenous Population of Leicester 33 (1992): 1085-1088.
- Bhansali SK. Abdominal tuberculosis. Experience with 300 cases. Am J Gastroenterology 67 (1977): 324-337.
- Sircar S, Taneja VA, Kansra U. Epidemiology and clinical presentation of abdominal tuberculosis- a retrospective study. J Indian Med Assoc 94 (1996): 352-354.