Prevalence of Bone Edema-like Lesions in Patients with Knee Osteoarthritis
Article Information
David A Kolin1, Antonio Madrazo-Ibarra1*, Hersh Patel1, Arda Dalkir1, Amoli Vad1, Nikhil Vad1, Kaitlin M Carroll1, Douglas N Mintz1, Vijay Vad1
Hospital for Special Surgery, Weill Cornell Medical College, New York, NY, USA
*Corresponding Author: Antonio Madrazo-Ibarra, Hospital for Special Surgery, Weill Cornell Medical College, New York, NY, USA.
Received: 03 March 2023; Accepted: 06 March 2023; Published: 14 March 2023
Citation:
David A Kolin, Antonio Madrazo-Ibarra, Hersh Patel, Arda Dalkir, Amoli Vad, Nikhil Vad, Kaitlin M Carroll, Douglas N Mintz, Vijay Vad. Prevalence of Bone Edema-like Lesions in Patients with Knee Osteoarthritis. Journal of Orthopedics and Sports Medicine. 5 (2023): 139-144.
View / Download Pdf Share at FacebookAbstract
Context: The presence of subchondral Bone Edema-Like Lesions (BELs) in patients with Knee Osteoarthritis (OA) is associated with increased pain and a faster progression of OA. However, the exact prevalence of BELs is controversial due to contradicting findings reported in previous studies.
Aim: To evaluate the prevalence of BELs by Magnetic Resonance Imaging (MRI), in patients with adjacent full-thickness cartilage loss of the knee. Settings and Design: Single center cross-sectional study.
Methods: We evaluated 100 consecutive MRI studies of patients with Kellgren and Lawrence grade IV knee osteoarthritis from April 2019 to May 2019. The primary outcome of the study was to evaluate the prevalence of BELs. The secondary outcome was to evaluate the association of BELs with the demographic characteristics of patients including age, sex, body mass index, presence of osteophytes, and previous diagnosis of osteoporosis or osteopenia.
Results: All patients had pain at the time of MRI evaluation. The average age was 66.5 ± 10.1 years and the average body mass index was 27.3 ± 5.1 kg/m². A total of 86 patients (86%) had BELs on the evaluated MRI, with both male and female patients being equally affected (P=0.405). No demographic characteristic showed a significant association with the presence of BELs. However, while not statistically significant, male patients, patients with obesity, and patients with osteophytes had an increased risk of having BELs.
Conclusion: The majority of patients with symptomatic grade IV knee osteoarthritis have BELs on MRI evaluation. No demographic characteristic was associated with a greater risk of presenting BELs.
Keywords
Bone Edema-Like Lesions; Bone Marrow Edema; Knee; Magnetic Resonance Imaging; Osteoarthritis
Knee osteoarthritis articles Knee osteoarthritis Research articles Knee osteoarthritis review articles Knee osteoarthritis PubMed articles Knee osteoarthritis PubMed Central articles Knee osteoarthritis 2023 articles Knee osteoarthritis 2024 articles Knee osteoarthritis Scopus articles Knee osteoarthritis impact factor journals Knee osteoarthritis Scopus journals Knee osteoarthritis PubMed journals Knee osteoarthritis medical journals Knee osteoarthritis free journals Knee osteoarthritis best journals Knee osteoarthritis top journals Knee osteoarthritis free medical journals Knee osteoarthritis famous journals Knee osteoarthritis Google Scholar indexed journals Articular cartilage articles Articular cartilage Research articles Articular cartilage review articles Articular cartilage PubMed articles Articular cartilage PubMed Central articles Articular cartilage 2023 articles Articular cartilage 2024 articles Articular cartilage Scopus articles Articular cartilage impact factor journals Articular cartilage Scopus journals Articular cartilage PubMed journals Articular cartilage medical journals Articular cartilage free journals Articular cartilage best journals Articular cartilage top journals Articular cartilage free medical journals Articular cartilage famous journals Articular cartilage Google Scholar indexed journals Musculoskeletal diseases articles Musculoskeletal diseases Research articles Musculoskeletal diseases review articles Musculoskeletal diseases PubMed articles Musculoskeletal diseases PubMed Central articles Musculoskeletal diseases 2023 articles Musculoskeletal diseases 2024 articles Musculoskeletal diseases Scopus articles Musculoskeletal diseases impact factor journals Musculoskeletal diseases Scopus journals Musculoskeletal diseases PubMed journals Musculoskeletal diseases medical journals Musculoskeletal diseases free journals Musculoskeletal diseases best journals Musculoskeletal diseases top journals Musculoskeletal diseases free medical journals Musculoskeletal diseases famous journals Musculoskeletal diseases Google Scholar indexed journals Osteoarthritis articles Osteoarthritis Research articles Osteoarthritis review articles Osteoarthritis PubMed articles Osteoarthritis PubMed Central articles Osteoarthritis 2023 articles Osteoarthritis 2024 articles Osteoarthritis Scopus articles Osteoarthritis impact factor journals Osteoarthritis Scopus journals Osteoarthritis PubMed journals Osteoarthritis medical journals Osteoarthritis free journals Osteoarthritis best journals Osteoarthritis top journals Osteoarthritis free medical journals Osteoarthritis famous journals Osteoarthritis Google Scholar indexed journals Body Mass Index articles Body Mass Index Research articles Body Mass Index review articles Body Mass Index PubMed articles Body Mass Index PubMed Central articles Body Mass Index 2023 articles Body Mass Index 2024 articles Body Mass Index Scopus articles Body Mass Index impact factor journals Body Mass Index Scopus journals Body Mass Index PubMed journals Body Mass Index medical journals Body Mass Index free journals Body Mass Index best journals Body Mass Index top journals Body Mass Index free medical journals Body Mass Index famous journals Body Mass Index Google Scholar indexed journals Osteoporosis articles Osteoporosis Research articles Osteoporosis review articles Osteoporosis PubMed articles Osteoporosis PubMed Central articles Osteoporosis 2023 articles Osteoporosis 2024 articles Osteoporosis Scopus articles Osteoporosis impact factor journals Osteoporosis Scopus journals Osteoporosis PubMed journals Osteoporosis medical journals Osteoporosis free journals Osteoporosis best journals Osteoporosis top journals Osteoporosis free medical journals Osteoporosis famous journals Osteoporosis Google Scholar indexed journals Subchondral bone articles Subchondral bone Research articles Subchondral bone review articles Subchondral bone PubMed articles Subchondral bone PubMed Central articles Subchondral bone 2023 articles Subchondral bone 2024 articles Subchondral bone Scopus articles Subchondral bone impact factor journals Subchondral bone Scopus journals Subchondral bone PubMed journals Subchondral bone medical journals Subchondral bone free journals Subchondral bone best journals Subchondral bone top journals Subchondral bone free medical journals Subchondral bone famous journals Subchondral bone Google Scholar indexed journals Femur articles Femur Research articles Femur review articles Femur PubMed articles Femur PubMed Central articles Femur 2023 articles Femur 2024 articles Femur Scopus articles Femur impact factor journals Femur Scopus journals Femur PubMed journals Femur medical journals Femur free journals Femur best journals Femur top journals Femur free medical journals Femur famous journals Femur Google Scholar indexed journals Tibia articles Tibia Research articles Tibia review articles Tibia PubMed articles Tibia PubMed Central articles Tibia 2023 articles Tibia 2024 articles Tibia Scopus articles Tibia impact factor journals Tibia Scopus journals Tibia PubMed journals Tibia medical journals Tibia free journals Tibia best journals Tibia top journals Tibia free medical journals Tibia famous journals Tibia Google Scholar indexed journals Cartilage articles Cartilage Research articles Cartilage review articles Cartilage PubMed articles Cartilage PubMed Central articles Cartilage 2023 articles Cartilage 2024 articles Cartilage Scopus articles Cartilage impact factor journals Cartilage Scopus journals Cartilage PubMed journals Cartilage medical journals Cartilage free journals Cartilage best journals Cartilage top journals Cartilage free medical journals Cartilage famous journals Cartilage Google Scholar indexed journals
Article Details
1. Introduction
The presence of subchondral Bone Edema-Like Lesions (BELs) in patients with Knee Osteoarthritis (OA) is associated with increased pain and a faster progression of OA [1-4]. Despite being non-specific for knee OA, BELs are a common finding in patients with symptomatic knee OA, especially in areas with greater cartilage loss [3]. The exact prevalence of BELs is controversial due to contradicting findings reported in previous studies [1, 3-11]. A good understanding of the relationship between BELs, symptoms, and the severity of OA would be important while keeping an eye on available therapeutic interventions and their global impact on knee OA. The osteochondral unit as a whole (including the subchondral bone, bone cartilage interface, and articular cartilage) has been suggested as the primary responsible for OA [12-14]. Its three components are highly interconnected and whenever one of them is affected, the others also are. BELs are an imaging finding, observed as an area of increased signal of intensity in fluid sensitive magnetic resonance imaging (MRI). BELs are not well understood even though it is commonly identified in different musculoskeletal pathologies. Felson et al. [2] were the first to describe the important relationship of BELs with knee OA, revealing a poorer prognosis of OA when BELs were present. Since that discovery, this relationship has been extensively studied reporting greater pain and a faster progression to total knee replacement when present, reinforcing the idea that future OA therapies could target BELs [1,4-11,15,16]. In order to propose BELs as a treatment target, we first need to understand it better. Previous studies have reported BELs are present in 13.7% to 82% of patients with knee OA, especially in male, overweight, and older patients [1,3,5-7,9,10]. But other studies have stated there is no association between demographic characteristics and the presence of BELs [5,11,17]. Due to the broad range of prevalence reported and the controversial associations with demographic characteristics, we conducted a study to better understand the relationship between BELs and knee OA. The purpose of this cross-sectional study was to evaluate the prevalence of BELs in 100 patients with symptomatic knee OA and describe the association of BELs with patient demographic characteristics.
2. Materials and Methods
This cross-sectional study was conducted at a single institution. A trained radiologist in musculoskeletal diseases evaluated consecutive knee MRIs of patients 50 years old or older, with a previous diagnosis of osteoarthritis grade IV Kellgren and Lawrence, starting in April 2019. The first 100 MRIs with full thickness cartilage loss either on the femur or the tibia, were included in the study. All MRIs with a total knee replacement were excluded. MRIs were collected at the Hospital for Special Surgery, a musculoskeletal specialized referral hospital in New York City. The starting point was arbitrarily selected in order to obtain an unbiased sample of patients. Demographic data including age, sex, Body Mass Index (BMI), and history of osteoporosis was collected from the electronic medical record of patients included in the study. The study was performed according to the Good Clinical Practice guidelines and the Declaration of Helsinki. The study was approved by the internal ethics committee and the internal review board of the Hospital for Special Surgery with the following registration number #2019-0818-AM1.
2.1 Magnetic Resonance Imaging Evaluation
BELs were defined as an area of increased signal of intensity located in the subchondral bone on Short Tau Inversion Recovery (STIR) images (Figure 1) [18]. BELs had to be located in the subchondral bone adjacent to the full-thickness cartilage loss to be considered related to OA. MRIs were also evaluated for the presence or absence of osteophytes defined as a focal bony outgrowth extending from a cortical surface in the knee joint. All MRI studies were analyzed by a fellowship-trained radiologist in musculoskeletal diseases, as well as a research fellow for the presence of BELs in any of the femoral condyles or tibial plateau. MRIs were performed using a 1.5-T or 3.0-T superconducting magnet (GE Medical Systems; Milwaukee, WI) using a standardized protocol. MRI was performed using 2-dimensional fast-spin echo images acquired along 3 anatomic planes (sagittal, coronal, axial) (time of repetition/time of echo [TR/TE], 4000 to 6000/25 to 30 ms; echo train length, 8 to 16; bandwidth, 32 to 62.5kHz over entire frequency range; acquisition matrix, 512 x 256-416; 1 or 2 number of excitations (NEX); field of view, 15 to 16 cm; slice thickness, 3.5 mm with no gap). Additional sagittal and coronals inversion recovery sequences were obtained (TR/TE, 5000 to 8000/18; echo train length, 8 to 16; time of inversion, 150 to 180; bandwidth 32 to 62.5; 256 x192, 1 or 2 NEX; field of view, 16 to 18 cm; slice thickness, 3.5 to 4.0 cm).
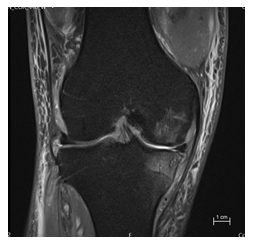
Figure 1: Magnetic resonance imaging of a 59-year-old male patient with knee osteoarthritis. This coronal STIR image demonstrates focal subchondral bone edema-like lesion in the medial femoral condyle and tibia.
2.2 Statistical Analysis
Continuous data with a normal distribution were expressed in terms of means and standard deviations, categorical data as frequencies and percentages. We calculated univariate Prevalence Odds Ratios (POR) and Prevalence Ratios (PR) to assess the association of BELs and demographic characteristics of the patients. If the proportion of cases was greater than 10%, PR was chosen over POR to prevent overestimation [19]. Two-tailed tests were used for all statistical analyses, with a P-value set to <0.05 to indicate statistical significance. Statistical analysis was performed using RStudio 2021.09.01 (PBC).
3. Results
3.1 Characteristics of the Population
Out of the 100 MRI studies included, more than half (54%) were female patients (Table 1). Even though all patients presented full-thickness cartilage loss, only 20% of patients had generalized OA affecting both the medial and lateral compartments of the knee. The medial compartment of the knee alone was the most commonly affected with OA. All patients (100%) presented knee pain at the time of the MRI evaluation, and 28% of patients had a history of diagnosed osteoporosis.
|
Characteristic |
All patients (N=100) |
Bone edema-like lesion (n=86) |
No bone edema-like lesion (n=14) |
P-value* |
|
Sex, n (%) |
0.405 |
|||
|
Male |
46 (46) |
41 (47.7) |
5 (35.7) |
|
|
Female |
54 (54) |
45 (52.3) |
9 (64.3) |
|
|
Age, years |
66.5 ± 10.1 |
67.0 ± 10.2 |
63.4 ± 9.5 |
0.213 |
|
BMI, kg/m² |
27.3 ± 5.1 |
27.6 ± 5.2 |
25.4 ± 3.5 |
0.063 |
|
OA Location, n (%) |
0.611 |
|||
|
Medial |
46 (46) |
41 (47.7) |
5 (35.7) |
|
|
Lateral |
34 (34) |
29 (33.7) |
5 (35.7) |
|
|
Both |
20 (20) |
16 (18.6) |
4 (28.6) |
|
|
Osteoporosis, n (%) |
28 (28) |
24 (27.9) |
4 (28.6) |
0.959 |
|
Bone edema-like lesion, n(%) |
||||
|
Femur |
10 (10) |
|||
|
Tibia |
18 (18) |
|||
|
Both |
58 (58) |
|||
|
All data are expressed as mean ± SD unless otherwise specified. |
||||
Table 1: Demographic Characteristics (N=100).
3.2 Bone Edema-Like Lesions
A total of 86 patients (86%) had BELs on the evaluated MRI study, with both male and female patients being equally affected (male 41 vs. female 45, P=0.405) (Table 1). The BMI of patients who had BELs was slightly higher than the ones that did not have BELs. However, statistically significant differences were found in any of the demographic characteristics comparing both groups (BELs vs. no BELs). If BELs were present, patients most commonly presented with edema in both the tibia and the femur concomitantly in 67% of the cases, compared to the tibia alone (21%), and the femur alone (10%).
3.3 Factors Associated with Bone Edema-like Lesion
In the univariate analysis for association, no demographic characteristic showed statistically significant association with the presence of BELs (Table 2). Despite no statistical significance, male patients (prevalence ratio 1.07; 95% Confidence Interval [CI], 0.91 to 1.25), patients with obesity (BMI >30 kg/m²) (prevalence ratio, with normal BMI as reference, 1.18; 95% CI, 0.99 to 1.41), and patients with osteophytes on MRI (prevalence ratio 1.19; 95% CI, 0.95 to 1.48) had a greater risk of presenting BELs.
|
Characteristic |
Bone edema-like lesion(n=86) |
No Bone edema-like lesion(n=14) |
Odds Ratio(95% CI) |
PR(95% CI) |
P-value |
|
Sex, n |
0.405 |
||||
|
Female |
45 |
9 |
Reference |
Reference |
|
|
Male |
41 |
5 |
1.64 (0.51-5.30) |
1.07 (0.91-1.25) |
|
|
Age, years |
|||||
|
50-59 |
24 |
5 |
Reference |
Reference |
|
|
60-69 |
28 |
5 |
1.17 (0.30-4.52) |
1.03 (0.82-1.28) |
0.823 |
|
70-79 |
22 |
3 |
1.53 (0.33-7.15) |
1.06 (0.85-1.33) |
0.589 |
|
≥80 |
12 |
1 |
2.50 (0.26-23.86) |
1.12 (0.89-1.40) |
0.414 |
|
BMI kg/m² |
|||||
|
Normal |
27 |
6 |
Reference |
Reference |
|
|
Overweight |
24 |
6 |
0.89 (0.25-3.13) |
0.98 (0.77-1.24) |
0.854 |
|
Obese |
28 |
1 |
6.22 (0.70-55.15) |
1.18 (0.99-1.41) |
0.067 |
|
Osteoporosis, n (%) |
0.959 |
||||
|
No |
62 |
10 |
Reference |
Reference |
|
|
Yes |
24 |
4 |
0.97 (0.28-3.38) |
1.00 (0.83-1.19) |
|
|
Osteophytes, n (%) |
0.062 |
||||
|
No |
22 |
7 |
Reference |
Reference |
|
|
Yes |
64 |
7 |
2.91 (0.92-9.23) |
1.19 (0.95-1.48) |
|
|
All data are expressed as frequency (%) unless otherwise specified. |
|||||
Table 2: Factor Associated with Bone Edema-like Lesions.
4. Discussion
By evaluating 100 consecutive MRI studies of patients with OA of the knee, we were able to better understand the relationship between BELs and knee OA. The most important finding of this study was that up to 86% of patients with full thickness cartilage loss in the knee have BELs on MRI. In the majority of patients, BELs were observed in both femur and tibia concomitantly. No demographic characteristic showed a significant association with the presence of BELs. However, a tendency was observed showing male patients, patients with obesity, or patients with osteophytes had slightly more risk of presenting BELs. These findings help lay the basis for further prospective studies, reaffirming BELs are a common finding in knee OA. Previous studies evaluating the prevalence of BELs in patients with knee OA have reported a broad range of prevalence going from 13.7% to 82% [1,3-11,16,17]. This large variability is primarily due to the different characteristics of the populations being studied. As described by Felson et al. [1] in 2001, symptomatic patients with OA are more likely to have BELs on MRIs. The reported prevalence in symptomatic patients has ranged from 57-82% [1,3,7-9]. On the contrary, only 13.6-30% of asymptomatic patients have showed to have BELs [1,5]. In our study 86% of the symptomatic patients with full thickness cartilage loss had BELs. The higher prevalence was somewhat expected since all of our patients had knee pain at the time of MRI evaluation. This high prevalence in symptomatic patients suggests BELs may be an important cause of knee pain, and also reaffirms bone is something we should be aware of in patients with knee OA once treatment therapies for this condition are available. Information regarding the association of demographic characteristics and the presence of BELs in patients with knee OA is controversial. On the one hand, some studies report BELs are commonly associated with male sex, more severe OA, higher BMI, and older age. On the other hand, Davies-Tuck et al. [5], Zhao et al. [11], Zhu et al. [17], and Kornaat et al. [8] found age, gender, BMI, and severity of OA had no association with the presence or development of BELs. The findings of our study support the idea that demographic characteristics have no significant association with the presence or absence of BELs. However, despite no statistical significance, we did observe a tendency for BELs to be present in males, older (>80 years), obese, and patients that had osteophytes at the time of evaluation. Our study had several potential limitations. First of all the intrinsic characteristics of a cross-sectional study do not allow evaluating casualty. The study time point was randomly selected to avoid bias; however, it was taken from a single tertiary musculoskeletal referral institution where most patients have advanced pathologies and come for surgical treatment. The sample size might have not been powered to find significance in the association analyses, however, since it was a secondary outcome, the study was not specifically designed for that. Patients with knee OA do not routinely have MRI studies, so there might have been other acute traumas or pathologies causing BELs. But by only taking into consideration BELs that were adjacent to the areas of full-thickness cartilage loss, we avoided counting acute BELs as if they were related to OA. The diagnosis of knee OA has continued to increase in the last decade due to the aging population and the increasing obesity rates. As a result, knee OA has become one of the main contributors to the Disability Adjusted Life Years [20]. Knee OA costs around 1%-2.7% of the gross domestic product in the US, with most of the costs attributed to the total knee replacement surgery and monetary losses associated with incapacity [21]. If BELs cause knee pain and a rapid progression of OA, treating it would signify reducing symptoms and the progression of the disease. Preventing the progression of OA and alleviating the patient’s symptoms may enable patients to continue working, without requiring surgery in the near future. This study reinforces that musculoskeletal physicians should be aware that BELs is commonly present in patients with knee OA regardless of demographic characteristics ultimately emphasizing the need for effective treatments targeting BELs.
Acknowledgments
We would like to thank Christopher Gaeta, Christopher Babu, Milen Nelivigi, and Tyler Uppstrom for their assistance in reviewing our manuscript.
Conflict of Interest
DK, AMI, HP, AD, AV, KC, NV, DM, and VV declare that there is no conflict of interest.
Authors Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by DK, AMI, HP, AD, AV, NV. Magnetic resonance imaging evaluation was performed by DM and VV. The first draft of the manuscript was written by DK and AMI. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
References
- Felson DT, Chaisson CE, Hill CL, et al. The Association of Bone Marrow Lesions with Pain in Knee Osteoarthritis 9 (2001).
- Felson DT, McLaughlin S, Goggins J, et al. Bone Marrow Edema and Its Relation to Progression of Knee Osteoarthritis. Ann Intern Med 139 (2003): 330.
- Hunter DJ, Zhang Y, Niu J, et al. Increase in bone marrow lesions associated with cartilage loss: a longitudinal magnetic resonance imaging study of knee osteoarthritis. Arthritis Rheum 54 (2006): 1529-1535.
- Roemer F, Guermazi A, Javaid M, et al. Change in MRI-detected subchondral bone marrow lesions is associated with cartilage loss: the MOST Study. A longitudinal multicentre study of knee osteoarthritis. Ann Rheum Dis 68 (2009): 1461-1465.
- Davies-Tuck ML, Wluka AE, Wang Y, et al. The natural history of bone marrow lesions in community-based adults with no clinical knee osteoarthritis. Annals of the Rheumatic Diseases 68 (2009): 904-908.
- Dore D, Quinn S, Ding C, et al. Natural history and clinical significance of MRI-detected bone marrow lesions at the knee: a prospective study in community dwelling older adults. Arthritis Res Ther 12 (2010): R223.
- Garnero P, Peterfy C, Zaim S, et al. Bone marrow abnormalities on magnetic resonance imaging are associated with type II collagen degradation in knee osteoarthritis: A three-month longitudinal study. Arthritis Rheum 52 (2005): 2822-2829.
- Kornaat PR, Kloppenburg M, Sharma R, et al. Bone marrow edema-like lesions change in volume in the majority of patients with osteoarthritis; associations with clinical features. Eur Radiol 17 (2007): 3073-3078.
- Tanamas SK, Wluka AE, Pelletier JP, et al. Bone marrow lesions in people with knee osteoarthritis predict progression of disease and joint replacement: a longitudinal study. Rheumatology 49 (2010): 2413-2419.
- Zhai G, Stankovich J, Cicuttini F, et al. Familial, structural, and environmental correlates of MRI-defined bone marrow lesions: a sibpair study. Arthritis Res Ther 8 (2006): R137.
- Zhao J, Li X, Bolbos RI, et al. Longitudinal assessment of bone marrow edema-like lesions and cartilage degeneration in osteoarthritis using 3 T MR T1rho quantification. Skeletal Radiol 39 (2010): 523-531.
- Findlay DM, Kuliwaba JS. Bone–cartilage crosstalk: a conversation for understanding osteoarthritis. Bone Res 4 (2016): 16028.
- Hoemann C, Lafantaisie-Favreau CH, Lascau-Coman V, et al. The Cartilage-Bone Interface. J Knee Surg 25 (2012): 085-098.
- Imhof H, Sulzbacher I, Grampp S, et al. Subchondral bone and cartilage disease: a rediscovered functional unit. Invest Radiol 35 (2000): 581-588.
- Boegård TL, Rudling O, Petersson IF, et al. Magnetic resonance imaging of the knee in chronic knee pain. A 2-year follow-up. Osteoarthritis and Cartilage 9 (2001): 473-480.
- Wang J, Antony B, Zhu Z, et al. Association of patellar bone marrow lesions with knee pain, patellar cartilage defect and patellar cartilage volume loss in older adults: a cohort study. Osteoarthritis and Cartilage 23 (2015): 1330-1336.
- Zhu Z, Ding C, Jin X, et al. Patellofemoral Bone Marrow Lesions: Natural History and Associations With Pain and Structure: Natural History of PF Joint BMLs. Arthritis Care & Research 68 (2016):1647-1654.
- McAlindon TE, Watt I, McCrae F, et al. Magnetic resonance imaging in osteoarthritis of the knee: correlation with radiographic and scintigraphic findings. Ann Rheum Dis 50 (1991):14-19.
- Tamhane AR, Westfall AO, Burkholder GA, et al. Prevalence Odds Ratio versus Prevalence Ratio: Choice Comes with Consequences. Stat Med 35 (2016): 5730-5735.
- Prince MJ, Wu F, Guo Y, et al. The burden of disease in older people and implications for health policy and practice. Lancet 385 (2015): 549-562.
- United States Bone and Joint Initiative: The Burden of Musculoskeletal Diseases in the United States (BMUS). In: BMUS: The Burden of Musculoskeletal Diseases in the United States (2014).
