Prevalence and Risk Factors of Anaemia at the First Antenatal Visit in Buea - Cameroon: A Cross-Sectional Study
Article Information
Ajong Brian Ngongheh1, Akateh Derek1, AgbornkwaiNyenty Agbor2, Calvin Besong Eta Oben2, Tambe Elvis Akem1, ChandiniAliyou Moustapha1, Mbarga EssimTheresse Nicole3, NdzoJudwin Alieh4, Longsti Scarlet Tabot Enanga1
1Ministry of Public Health Cameroon, Cameroon.
2Elisabeth Glaser Paediatric Aids Foundation (EGPAF) Cameroon
3International Medical Corps (IMC) Cameroon
4University Hospital Southampton NHS Foundation Trust (UHSFT)
*Corresponding author: Ajong Brian Ngongheh, Ministry of Public Health Cameroon, Cameroon
Received: 01 May 2021; Accepted: 10 May 2020; Published: 30 June 2020
Citation: Ajong Brian Ngongheh, Akateh Derek, AgbornkwaiNyenty Agbor, Calvin Besong Eta Oben, Tambe Elvis Akem, ChandiniAliyou Moustapha, MbargaEssimTheresse Nicole, NdzoJudwin Alieh, Longsti Scarlet Tabot Enanga. Prevalence and Risk Factors of Anaemia at the First Antenatal Visit in Buea - Cameroon: A Cross-Sectional Study. Fortune Journal of Health Sciences 4 (2021): 359-372.
View / Download Pdf Share at FacebookAbstract
Background: Anaemia in pregnancy is a risk factor for maternal and neonatal morbidity and mortality. Interventions to reduce its burden start from the first antenatal visit and continue throughout pregnancy. Previous studies report that anaemia in pregnancy is a public health concern as early as the first antenatal visit. This study sought to measure the prevalence and identify risk factors of anaemia among pregnant women attending their first antenatal visit.
Methods: A cross-sectional study was conducted at Buea Regional Hospital. Questionnaires were administered to collect socio-demographic data and risk factors of anaemia in pregnancy. Blood was used to measure haemoglobin concentration, malaria parasitaemia and HIV serology. Risk factors for anaemia in pregnancy were identified using univariable and multivariable analysis in logistic regression. P–values <0.05 were considered statistically significant.
Results: Among 250 pregnant women, 171 (68.4%) were anaemic. In multivariable analysis, malaria infection and gravidity were significantly associated with anaemia in pregnancy (AOR=9.47, p<0.001 and AOR=1.98, p=0.044respectively). There was a strong negative correlation between malaria parasitaemia and haemoglobin concentration (r= -0.5816, p<0.001). Early anti-malaria therapy during the current pregnancy was associated with a lower risk of anaemia in pregnancy among primigravida (AOR=0.378, p=0.013).
Conclusions: High prevalence of anaemia in pregnancy in this study demonstrates its public health importance in the first antenatal visit. Malaria infection and parity are strong modifiable and non-modifiable risk factors respectively. Prompt anti-malaria therapy in primigravida is critical in reducing anaemia in pregnancy.
Keywords
Anaemia; Antenatal
Sectional Study articles, Anaemia articles Anaemia Research articles Anaemia review articles Anaemia PubMed articles Anaemia PubMed Central articles Anaemia 2023 articles Anaemia 2024 articles Anaemia Scopus articles Anaemia impact factor journals Anaemia Scopus journals Anaemia PubMed journals Anaemia medical journals Anaemia free journals Anaemia best journals Anaemia top journals Anaemia free medical journals Anaemia famous journals Anaemia Google Scholar indexed journals Antenatal articles Antenatal Research articles Antenatal review articles Antenatal PubMed articles Antenatal PubMed Central articles Antenatal 2023 articles Antenatal 2024 articles Antenatal Scopus articles Antenatal impact factor journals Antenatal Scopus journals Antenatal PubMed journals Antenatal medical journals Antenatal free journals Antenatal best journals Antenatal top journals Antenatal free medical journals Antenatal famous journals Antenatal Google Scholar indexed journals Buea Health District articles Buea Health District Research articles Buea Health District review articles Buea Health District PubMed articles Buea Health District PubMed Central articles Buea Health District 2023 articles Buea Health District 2024 articles Buea Health District Scopus articles Buea Health District impact factor journals Buea Health District Scopus journals Buea Health District PubMed journals Buea Health District medical journals Buea Health District free journals Buea Health District best journals Buea Health District top journals Buea Health District free medical journals Buea Health District famous journals Buea Health District Google Scholar indexed journals white blood cells articles white blood cells Research articles white blood cells review articles white blood cells PubMed articles white blood cells PubMed Central articles white blood cells 2023 articles white blood cells 2024 articles white blood cells Scopus articles white blood cells impact factor journals white blood cells Scopus journals white blood cells PubMed journals white blood cells medical journals white blood cells free journals white blood cells best journals white blood cells top journals white blood cells free medical journals white blood cells famous journals white blood cells Google Scholar indexed journals Human Diagnostic articles Human Diagnostic Research articles Human Diagnostic review articles Human Diagnostic PubMed articles Human Diagnostic PubMed Central articles Human Diagnostic 2023 articles Human Diagnostic 2024 articles Human Diagnostic Scopus articles Human Diagnostic impact factor journals Human Diagnostic Scopus journals Human Diagnostic PubMed journals Human Diagnostic medical journals Human Diagnostic free journals Human Diagnostic best journals Human Diagnostic top journals Human Diagnostic free medical journals Human Diagnostic famous journals Human Diagnostic Google Scholar indexed journals HIV articles HIV Research articles HIV review articles HIV PubMed articles HIV PubMed Central articles HIV 2023 articles HIV 2024 articles HIV Scopus articles HIV impact factor journals HIV Scopus journals HIV PubMed journals HIV medical journals HIV free journals HIV best journals HIV top journals HIV free medical journals HIV famous journals HIV Google Scholar indexed journals
Article Details
1. Introduction
Anaemia is a global problem affecting people of all age groups in both low-income and high-income countries [1,2]. Nevertheless, it is more prevalent in low-income countries among pregnant women and children [1,3]. The World Health Organisation (WHO) estimates that more than half of the pregnant women worldwide have a haemoglobin concentration less than 11.0gl/dl which is diagnostic of anaemia in pregnancy [4]. It is reported that, women in developing countries account for 95% of all anaemic pregnancies in the world [5]. Despite this high burden of anaemia in low-income countries, it is usually neglected both by individual patients and clinicians.
The aetiology of anaemia in pregnancy is multifactorial. Some identified causes include: micro-nutrient deficiencies for example folic acid and iron deficiency; infections and infestations by parasites for example hookworm, schistosomiasis, malaria, HIV; haemoglobinopathies for example thalassaemia and sickle cell disease [6]; and physiological haemodilution in pregnancy which is maximum in the second trimester [7].
Anaemia in pregnancy has adverse effects on both the mother and the foetus. It contributes to over 20% of maternal deaths in Africa [8]. Furthermore, severe anaemia in pregnancy leads to a reduction in the blood flow to the foetus predisposing to foetal hypoxia which can lead to intra-uterine growth retardation, and neonatal death [8].
A national survey of anaemia in pregnancy in Cameroon reported a prevalence of 50.9% [2]. According to WHO classification a prevalence of anaemia greater than 40% is a severe problem of public health significance [2]. This clearly demonstrates that anaemia in pregnancy is a severe problem of public health significance. Despite relentless efforts to curb down the incidence and prevalence of anaemia in pregnancy, it still remains a severe public health problem in Cameroon [2]. Interventions to reduce anaemia in pregnancy usually start from the first antenatal visit and continue throughout pregnancy. The first antenatal visit during pregnancy is critical because it is the moment when most pregnant women have their first contact with the health system during their current pregnancy. Nevertheless, Current evidence suggests that anaemia in pregnancy is an established serious public health problem as early as the first antenatal visit. It is important to understand the burden and risk factors of anaemia in pregnancy, especially during the first antenatal visit in view of improving public health programs on how to target anaemia in early pregnancy which is currently a public health problem. Furthermore, reducing the burden of anaemia in pregnancy requires good locally generated data of its prevalence and associated risk factor which is not readily available in Buea. Thus, this study sought to measure the prevalence and identify risk factors of anaemia among pregnant women attending their first antenatal visit at the Buea Regional Hospital.
2. Methods
2.1 Study design and study setting
The cross sectional design was used and the study involved pregnant women attending their first antenatal visit at the Buea Regional Hospital from June 2013 to October 2013. Buea is a town situated at the foot of Mount Cameroon and has an estimated population of 90,088 inhabitants according to the last census in 2005 [unpublished data]. The Buea Regional Hospital is a 3rd category (or 2nd referral level hospital) and receives patients from Buea Health District.
2.2 Participant eligibility
Consenting pregnant women attending their first antenatal visit at the Buea Regional Hospital during the study period were included in the study.
2.4 Sample size calculation
Based on sample size calculations, a minimum of 229 participants were required to measure the prevalence of anaemia among pregnant women at their first antenatal visit with a precision of 6% and a confidence level of 95%. It was hypothesized that the prevalence of anaemia among pregnant women attending their first antenatal visit will be 68.9% as reported in previous studies [9]. A precision of 6% was chosen to reduce the minimum required sample size due to limited resources.
2.5 Participant Selection
After routine health talks during regular antenatal visits, study participants were counselled by the study assistant on the aim of the study. Written informed consent was sought from all participants.
2.6 Data collection
An interviewer administered questionnaire was designed from a comprehensive review of previous literature on risk factors of anaemia in pregnancy. This was used to collect information on socio demographic characteristics and risk factors for anaemia in pregnancy. The study assistants were trained on data collection and questionnaire completion.
Maternal capillary blood was obtained by a finger prick of the fourth digit. A drop of capillary blood was placed on the test card of a portable STAT-site haemoglobin meter (Stan bio Laboratory, Boerne, Texas U.S.A, serial number: 00024315) and the haemoglobin (HB) value was read off.
Capillary blood was used to prepare thick and thin blood films for observation of malaria parasites. The blood films were air-dried. The thin blood film was fixed with 100% methanol and then allowed to air-dry again. Both blood films were stained by flooding the slides with 10% Giemsa for 15 minutes, after which the stain was washed off and the slides allowed to air-dry. The slides were examined by a certified laboratory technician under a light microscope using the oil immersion objective (x100 objective) for malaria parasites in the parasitology laboratory of the Faculty of Health Sciences. Malaria parasites were counted against 200 white blood cells (WBC) and the parasite density was calculated in trophozoites/µl of blood using the formula below [10].
Where Malaria parasite density = number of parasites per μl of blood, calculated in trophozoites/µl of blood;
n = Number of malaria parasites counted against 200 WBCs:
N = Number of WBCs counted (We counted parasites against 200 WBCs);
WBC count =white blood cell count of participants was not measured and was assumed to be 8000 cell/μl which is a universally accepted standard [10]. A slide was considered as negative after examining 100 fields that showed no parasites.
After pre-test counselling, 5ml of venous blood was collected into an EDTA tube which was labelled with the participant’s study number. The blood was centrifuged at 1000 cycles per minute and the Determine rapid test (Alere DetermineTM HIV-1/2 rapid test kits [Alere Medical Co., Japan]) performed on the plasma. Samples which tested positive for HIV were tested again with the second line Hexagon (Human Diagnostic, Germany) test kit. If positive with Hexagon, the sample was considered seropositive for HIV. After counselling, the results of the haemoglobin concentration, malaria parasitaemia and HIV status were issued to the participants and they were provided with appropriate advice on care.
2.7 Quality control
For quality control, 20% of the negative samples and 20% of the positive samples were randomly selected and re-examined by another laboratory technician. The laboratory technicians who examined the slides for malaria parasites, conducted haemoglobin measurement and HIV status were blinded to the response of the participant questionnaire. The initial questionnaire was piloted on 10 participants and the questions were adapted as necessary.
2.8 Data entry and analysis
The data obtained was entered into Microsoft Excel version 7. The excel spread sheet was imported to STATA 14 for analysis. Descriptive statistics on the socio demographic characteristics and the distribution of risk factors among participants was computed. A logistic regression model for each exposure variable was computed in the univariable analysis for their association with anaemia and all p-values were obtained from likelihood ratio tests. Exposure variables that were significantly associated with anaemia in univariable analysis were included in a multivariable logistic regression model and likelihood ratio tests were conducted for each of the exposure variables in the final model. A linear regression was conducted between the haemoglobin measurement and the malaria parasitaemia among the study participants. All P-values less than 0.05 were considered statistically significant.
2.9 Operationalisation of variables
Anaemia in pregnancy was defined by a haemoglobin Concentration <11 g/dl [11]. The severity of anaemia was classified into three classes according to the WHO cut-off for the severity of anaemia at sea level [11]. Mild anaemia: haemoglobin of 10-10.9 g/dl; Moderate anaemia: haemoglobin of 7-9.9 g/dl; Severe anaemia: haemoglobin of <7 g/dl [11]. The gestational age was expressed in weeks and was divided into trimesters as follows [7]: First trimester: gestational age < 14 weeks; Second trimester: gestational age 14 - 28 weeks; Third trimester gestational age > 28 weeks. Fever was defined as an axillary temperature above 37.5oC. Clinical malaria was defined as malaria parasitaemia plus fever [12].
2.10 Ethical clearance and ethical considerations
Ethical clearance was obtained from the Institutional Review Board (IRB) of the Faculty of Health Sciences, University of Buea. Study participants signed an informed consent form, after counselling by the investigator. All data was stored and was only accessible to the principal investigator. Questionnaires and the sample bottles were anonymously labelled. Administrative clearance was obtained from the Buea Regional Hospital and the South-West Regional Delegation for Public Health.
3. Result
A total of 250 pregnant women were enrolled in the study. The age of the study participants ranged from 17 - 39 years, with a mean age of 26.1 ± 5.1 years. Most women n=234 (93.6%) were above 20 years of age (Table 1). shows the detailed summary of the socio demographic characteristics of the study participants. The gestational age among participants ranged from 10 - 37 weeks, with a mean gestational age of 20.6 ± 4.8 weeks. Most women 212 (86.9%) enrolled for the booking visit at the second trimester, meanwhile 22 (9%) enrolled in the first trimester, and the rest 10 (4.1%) enrolled in the third trimester. Information on the gestational age for 6 women was missing because they could neither remember the date of their last menstrual period nor the gestational age of their pregnancy. The gravidity of the study participants ranged from 1 to 6, with a median gravidity of 2. Most women 142 (56.8%) were multigravida. A total of 18 (7.2%) participants tested HIV seropositive. Most women were married 128 (51.2%). A total of 98 (39.2%) women had malaria parasites in their blood film. For those who the malaria parasite count varied from 40 to 36,600 parasites/µl (median = 2,600; IQR = 120 - 20,050). The geometric mean parasite count was 2,643. A total of 14 (5.6%) women were coinfected with malaria and HIV.
Table 1: Socio-demographic characteristics of the study participants
|
Characteristic |
Number |
Percentage (%) |
Mean ± SD |
|
Age |
26.8 ± 5.1 |
||
|
Less than 20 years |
16 |
6.4 |
- |
|
More than 20 years |
234 |
93.6 |
- |
|
Gestational age (weeks) |
- |
- |
20.6 ± 4.8 |
|
First trimester |
22 |
9 |
- |
|
Second trimester |
212 |
86.9 |
- |
|
Third trimester |
10 |
4.1 |
- |
|
Gravidity |
- |
- |
2.2 ± 1.3 |
|
Primigravida |
108 |
43.2 |
- |
|
Multigravida |
142 |
56.8 |
- |
|
Parity |
- |
- |
0.8 ± 1.2 |
|
Nulliparous |
150 |
60 |
- |
|
Primiparous |
35 |
14 |
- |
|
Multiparous |
65 |
26 |
- |
|
Educational level |
|||
|
Below university education |
148 |
59.2 |
- |
|
University education |
102 |
40.8 |
- |
|
Marital status |
|||
|
Single |
122 |
48.4 |
- |
|
Married |
128 |
51.2 |
- |
|
Malaria parasite |
|||
|
Negative |
152 |
60.8 |
- |
|
Positive |
98 |
39.2 |
- |
3.1 Haemoglobin and anaemia
The HB ranged from 5 to 14 g/dl with a mean of 10.2 ± 1.6 g/dl. The prevalence of anaemia in pregnancy was 68.4% (n=171, CI: 0.60 - 0.72). Two (0.8%) women were severely anaemic, while most 113 (45.2%) were moderately anaemic and 51 (20.4%) were mildly anaemic.
3.2 Univariable analysis between anaemia and exposure variables
In univariate analysis, young age (defined by <20years), parity, gravidity, ownership of mosquito bed net and the administration of an antimalarial drug during the current pregnancy before the first ANC visit were significantly associated with anaemia (Table 2). Shows the odds ratios obtained from the univariate analysis. Relative to women without malaria, those with malaria parasitaemia were 11 times more likely to have anaemia in pregnancy (OR = 11.25; CI 5.11 - 24.79, p <0.001). Furthermore, women under 20 years of age were8.24 times more likely of having anaemia relative to those who were above 20 years of age (OR = 8.24; CI 1.07 - 63.53, p<0.001). Women who owned bednets were less likely of being anaemic relative to those who did not own bednets (OR = 0.56: CI 0.33 - 0.95, p = 0.03). Relative to multigravida women, primigravida had three times the odds of being anaemic (OR =3.61; CI 0.15 - 0.50, p<0.001). Relative to Multiparous women, Nulliparous women had two times the odds of being anaemia (OR = 2.51; CI 1.47 - 4.30, p < 0.001). Relative to women who received an antimalarial drug during the current pregnancy, those who did not receive an antimalaria drug had 2 times the odd of being anaemic (OR 2.02, CI 1.16 - 3.50 P = 0.013).Anaemia in pregnancy was significantly associated with malaria and HIV coinfection, with all coinfected women being anaemic (Χ2= 7.50, p = 0.006).
Table 2: Univariate analysis between anaemia and predictor variables
|
Variable |
Anaemia (%) |
Crude OR |
CI |
P-value |
|
Malaria |
||||
|
Negative |
76 (50) |
1 |
- |
<0.001 |
|
Positive |
90 (91.8) |
11.25 |
5.11 - 24.79 |
|
|
Age group |
||||
|
More than 20 years |
151 (64.5) |
1 |
- |
<0.001 |
|
Less than 20 years |
15 (93.8) |
8.24 |
1.07 - 63.53 |
|
|
Ownership of bednet |
||||
|
No |
101 (72.1) |
1 |
- |
0.031 |
|
Yes |
65 (59.1) |
0.56 |
0.33 - 0.95 |
|
|
Slept under bednet last night* |
||||
|
No |
43 (60.6) |
1 |
- |
0.672 |
|
yes |
22 (56.4) |
0.84 |
0.38 - 1.86 |
|
|
Trimester of pregnancy |
||||
|
First |
14 (63.6) |
1 |
- |
0.203 |
|
Second |
139 (65.6) |
1.09 |
0.44 - 2.71 |
|
|
Third |
9 (90.0) |
5.14 |
0.55 - 48.37 |
|
|
Gravidity |
||||
|
Multigravida |
78 (54.9) |
1 |
- |
<0.001 |
|
Primigravida |
88 (81.5) |
3.61 |
2.01 - 6.50 |
|
|
Fever (axillary temperature >37.5) |
||||
|
No |
132 (69.1) |
1 |
- |
0.11 |
|
Yes |
34 (57.6) |
0.61 |
0.33 - 1.11 |
|
|
History of Fever in the current pregnancy |
||||
|
No |
132 (69.1) |
1 |
- |
0.245 |
|
Yes |
34 (57.6) |
1.39 |
0.80 - 2.41 |
|
|
HIV status |
||||
|
No |
150 (64.7) |
1 |
- |
0.053 |
|
Yes |
16 (88.9) |
4.37 |
0.98 - 19.49 |
|
|
Marital status |
||||
|
Single |
85 (69.7) |
1 |
- |
0.28 |
|
Married |
81 (63.3) |
0.75 |
0.44 - 1.27 |
|
|
Clinical Malaria |
||||
|
No |
142 (63.7) |
1 |
- |
0.004 |
|
Yes |
24 (88.9) |
4.56 |
1.33 - 15.63 |
|
|
Antimalaria treatment during the current pregnancy |
||||
|
No |
121 (71.6) |
1 |
- |
0.013 |
|
Yes |
45 (55.6) |
0.50 |
0.29 - 0.86 |
|
3.3 Multivariable analysis between anaemia and exposure variables
In multivariable analysis, malaria parasitaemia and gravidity were significantly associated with anaemia (Table 3). shows the odds ratios obtained from the multivariable analysis. Relative to women without malaria, those with malaria parasitaemia were 9.479 times more likely of having anaemia (AOR 9.47; CI = 4.20 - 21.29, p <0.001) after adjusting for administration of antimalaria during the current pregnancy, Gravidity, ownership of bednet and maternal age group. Furthermore, relative to multigravida women, primigravida women had 1.98 times more likely of having anaemia (AOR = 1.98: CI 1.01 - 3.88, p = 0.044) after adjusting for administration of antimalaria during the current pregnancy, malaria parasitaemia, ownership of bednet and maternal age group.
Table 3: Multivariable analysis between significant univariable covariates and outcome
|
Variable |
Adjusted OR |
CI |
P-value |
|
Malaria |
|||
|
Negative |
1 |
- |
<0.001 |
|
Positive |
9.47 |
4.20 - 21.29 |
|
|
Age group |
|||
|
More than 20 years |
1 |
- |
0.084 |
|
Less than 20 years |
4.99 |
0.59 - 43.04 |
|
|
Ownership of Mosquito bednets |
|||
|
No |
1 |
- |
0.223 |
|
Yes |
0.68 |
0.37 - 1.23 |
|
|
Gravidity |
|||
|
Multigravida |
1 |
- |
0.044 |
|
Primigravida |
1.98 |
1.01 - 3.88 |
|
|
Antimalaria treatment during the current pregnancy |
|||
|
No |
1 |
- |
0.075 |
|
Yes |
0.56 |
0.30 - 1.06 |
|
3.4 Effect modification of early anti-malaria therapy and gravidity
There was a modification of the association between early anti-malaria therapy and relative risk of anaemia in pregnancy by gravidity (Χ2 = 3.66, p = 0.056). The adjusted stratum specific OR for the association between anti-malaria therapy and anaemia among primigravida and multigravida are illustrated in (Table 4). There was strong evidence that administration of early anti-malaria therapy during the current pregnancy in primigravidawas associated with a lower odds of anaemia in pregnancy (OR = 0.378, CI = 0.175 - 0.816, p = 0.013) after adjusting for malaria infection, ownership of bednet and maternal age group. This protective effect was not seen among multigravida.
Table 4: Stratum Specific AOR of association between anti-malaria treatment and anaemia in pregnancy
|
Gravidity |
AOR of association between anti-malaria treatment in current pregnancy and anaemia in pregnancy |
CI |
p-value |
|
Primigravida |
0.38 |
0.175 - 0.816 |
0.013 |
|
Multigravida |
1.58 |
0.430 - 5.785 |
0.491 |
3.5 Variation of malaria parasitaemia and haemoglobin
Among participants who had malaria, there was a strong negative correlation between the haemoglobin level and malaria parasitaemia of participants (β = -0.00013, r = -0.5816, p <0.001) (Figure 1). Shows the scatter plot of haemoglobin concentration and malaria parasitaemia and a fitted regression line.
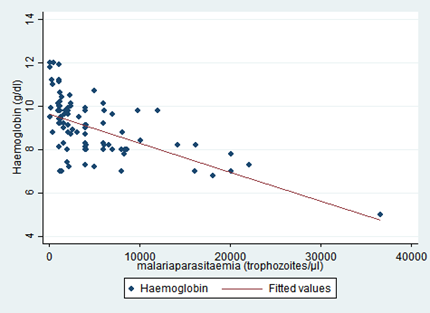
Figure 1: Scatter plot of haemoglobin and malaria parasitaemia count with fitted regression line
4. Discussion
This study sought to measure the prevalence and identify risk factors of anaemia among pregnant women attending their first antenatal visit at the Buea Regional Hospital. The prevalence of anaemia in the first antenatal visit in this study was 68.4%. Malaria infection and gravidity were significantly associated with anaemia at the first antenatal visit. Relative to women without malaria, those with malaria parasitaemia had 9.47 times more likely of having anaemia during the first antenatal visit. Furthermore, relative to multigravida, primigravida had 2.07 times more likely of having anaemia during the first antenatal visit.
Evidence from previous studies in malaria endemic countries have shown varying results on the prevalence of anaemia in pregnancy. A cross sectional study of women in their first ANC visit in Buea reported a similar prevalence of 68.9% [9]. The prevalence of severe anaemia in this study was 0.8% which is half that reported in a previous study in Buea [9]. This discrepancy may be due to the different techniques of haemoglobin measurement used in both studies. It has been well documented that measurements of the prevalence and incidence of anaemia are fundamentally dependent on the methods of blood collection and techniques of haemoglobin measurement [13]. In this study, we used a haemoglobin meter, while Achidi et al [9]. Used microcapillary tubes to measure the HB. Other studies in malaria endemic countries in Sub-Saharan Africa found similar prevalence of anaemia in pregnancy like in Kenya (69.1%) [6] and Calabar (59.6%) [14]. Furthermore, the prevalence of anaemia in this study was higher than the national prevalence of anaemia in pregnancy in Cameroon of 50.9% reported by WHO in 2008 [2]. On the other hand, lower prevalence of anaemia during the booking visit have been documented in other malaria endemic regions in Sub-Saharan Africa like Ibadan, Nigeria (25.6%) [15], and Port Harcourt, Nigeria (23.2% )[8].
Malaria infection is a significant cause of anaemia among pregnant women in malaria endemic regions. In this study, malaria infection was associated with almost 10 times increase in the odds of having anaemiaat the first antenatal visit after adjusting for other potential confounders. Similar studies have also found a strong association between malaria infection and anaemia at the first antenatal visit, but reported lower odds of disease association. Achidi et al. reported an OR of 2.86 [9]; Ouma et al. reported an OR of 1.34 [6]; Bardaji et al. reported an OR of 4.01 [16]. There are plausible reasons for the higher OR observed in our study compared to the others. The women in our study had a higher malaria parasitaemia with a higher geometric mean malaria parasite density of 2,643 compared to a mean parasite density of 994 reported by Achidi et al. [9]. and 1,678 reported by Bardaji et al. [16]. This higher parasite density could be the underlying reason for the stronger association between malaria infection and anaemia observed in our study. This supposition is further strengthened by the strong negative correlation between malaria parasitaemia and haemoglobin concentration found in this study. The pathophysiology of anaemia due to malaria has been well described. Some of the mechanisms through which malaria infection causes anaemia are: removal of parasitized red blood by the immune system: excessive removal and destruction of non-parasitized red blood by the immune system: and suppression erythropoiesis in the bone marrow [6]. The aetiology of anaemia in pregnancy is multifactorial but previous studies have shown that in tropical Africa, malaria infection, Iron and folate deficiencies are the most important causes [9].
Primigravida have a higher risk of malaria-induced anaemia in pregnancy compared to multigravida. In our study, primigravida had 2 times the odds of having anaemia during the first antenatal visit relative to multigravida. Similar findings have been reported in other studies [9]. A meta-analysis of an association between anaemia in primigravida compared to multigravida in malaria endemic regions reported that primigravida had 1.32 times the odds of having anaemia in pregnancy compared to multigravida (95%; CI 1.15-1.52) [17]. On the other hand, this discrepancy in the risk of being anaemic among primigravidae and multigravidae is absent in areas which are not endemic for malaria [17]. The higher prevalence of anaemia in primigravidae can be attributed to their higher susceptibility to malaria in pregnancy due to their lower immunity to malaria. On the other hand, primigravida who took an anti-malaria drug before the first antenatal visit were less likely to have anaemia in pregnancy.
HIV infection is an important risk factor for anaemia in pregnancy. Previous studies have identified HIV infection as a risk factor for anaemia in pregnancy [18,19]. Nevertheless, in our study, HIV was not significantly associated with anaemia. The p-value of the odds ratio for the association between HIV and anaemia was however very close to the cut-off for statistical significance. Therefore, a plausible reason why HIV infection was not significantly associated with anaemia in our study could be because our study was not powered to detect an association between HIV infection and anaemia. On the other hand, the mean haemoglobin among HIV positive women was lower than those of HIV negative women. Previous studies in Cameroon have reported HIV seropositive mothers to have a significantly lower haemoglobin compare to HIV negative mothers [20].
Public health interventions to reduce the burden of anaemia in pregnancy usually start at the first antenatal visit. This is because it is usually the time during which pregnant woman have their first contact with the health care system during pregnancy. Some of the interventions currently implemented in the Buea Regional Hospital include: routine provision of haematinics (iron and folic acid supplements) to pregnant women, routine testing and prompt treatment of malaria infections, provision of free mosquito nets in pregnancy and provision of Sulfadoxine and Pyrimethamine intermittent preventive therapy during pregnancy. Nevertheless, as our study has demonstrated, anaemia associated with malaria is a severe problem at first antenatal visit. Therefore, there is a need for innovative interventions which address the problem before the first antenatal visit. Previous studies have reported that most women of reproductive age in low-income countries have iron and folic acid deficiency, with risk factors acting synergistically, increasing their risk of anaemia [21]. Some of these factors include: poor nutrition; repeated infections by parasites like malaria and hookworm; monthly blood loss; and repeated pregnancies [21]. Therefore, designing and implementing public health interventions targeting women of reproductive age during preconception care could help to contribute in the reducing the burden of anaemia at the first antenatal visit and its burden in pregnancy.
Despite adding to the literature, our study has some limitations. Due to the small sample size, it is plausible that we could not detect statistical significance between some exposures and the outcome. Due to limited resources, some known causes of anaemia in pregnancy were not measured such as iron deficiency, helminthic infestation, chronic diseases, nutritional deficiencies. This could have led to an overestimation of the odds of association between anaemia and malaria.
5. Conclusions
Anaemia is a severe problem of public health significance as early as the first antenatal visit among pregnant women in the Buea Regional Hospital. Malaria infection and gravidity were significantly associated with anaemia at the first antenatal visit. This adds to the evidence of the risk of malaria and primigravida status as potential risk factors for anaemia in pregnancy. While there are interventions in place to reduce the burden of malaria and anaemia in pregnancy, women can only benefit after the booking visit when malaria and anaemia are already significant problems. Thus, there is a need for interventions higher upstream before women get pregnant via preconception care and during early pregnancy, especially during the first pregnancy. Our study design could only allow us to demonstrate associations and not a direct causal relationship between exposure and outcome variables. We recommend that more detailed studies be carried out to identify the causes of anaemia in pregnancy in the Buea Health district.
5.1 What is already known on this topic
- Anaemia in pregnancy is a major problem of public health significance in Sub-Saharan Africa.
- In malaria endemic countries, malaria is strongly associated with anaemia in pregnancy.
- Relative to multigravida, primigravida are at a higher risk of malaria and anaemia in pregnancy.
5.2 What this study adds
- There is a strong inverse relationship between malaria parasitaemia and haemoglobin concentration in pregnant women.
- There is evidence that early anti-malaria therapy during the current pregnancy before the first ANC visit in primigravida is associated with a lower relative risk of anaemia in pregnancy.
- Malaria and HIV coinfection is strongly associated with anaemia in pregnancy.
6. Competing interests
The authors of this research declare no conflicts of interest.
7. Funding
There was no external funding for this research.
8. Authors' contributions
ABN conceived the research idea, conducted the study, analysed the study and wrote the manuscript of this paper. AD, ANA, CBEO, TEA, CAM, METN, NJA proof-read and made necessary corrections to the manuscript.
9. Acknowledgements
The authors wish to thank all the members of the research collaboration group: Cameroon Initiative for Excellence in Clinical and Public Health Research (CIECPHER) for their support in writing this project.
References
- Getahun W, Belachew T, Wolide AD. Burden and associated factors of anaemia among pregnant women attending antenatal care in southern Ethiopia?: cross sectional study. BMC Res Notes 10 (2017):1-7.
- World Health Organization. Worldwide prevalence of anaemia 1993-2005: WHO global database on anaemia [Internet]. Benoist B de, McLean E, Egli I, Cogswell M, editors. World Health Organisation. Geneva: WHO Press; (2008):51.
- Gebre A, Mulugeta A. Prevalence of anaemia and associated factors among pregnant women in north western zone of tigray, northern Ethiopia: A cross-sectional study. J Nutr Metab. (2015):1-7.
- Idowu O a, Mafiana CF, Sotiloye. A survey of anaemia among pregnant women in Abeokuta, Nigeria. Afr Health Sci 5 (2005):295-9.
- Marchant T, Schellenberg JA, Nathan R, Abdulla S, Mukasa O, Mshinda H, et al. Anaemia in pregnancy and infant mortality in Tanzania. Trop Med Int Heal 9 (2004):262-6.
- Ouma P, Van Eijk AM, Hamel MJ, Parise M, Ayisi JG, Otieno K, et al. Malaria and anaemia among pregnant women at first antenatal clinic visit in Kisumu, western Kenya. Trop Med Int Heal 12 (2007):1515-23.
- Aghajanian P, Ainbinder SW, Akhter MW, Andrew DE, Dennis R. Anti E, Archie CL, et al. Current Diagnosis & Treatment Obstetrics & Gynecology. 10th ed. H. DA, Nathan L, Goodwin TM, Laufer N, editors. McGraw-Hill Companies (2007):500.
- Buseri FI, Uko EK, Jeremiah ZA, Usanga EA. Prevalence and Risk Factors of Anaemia Among Pregnant women in Nigeria. Open Hematol J 2 (2008):14-9.
- Achidi EA, Kuoh AJ, Minang JT, Ngum B, Achimbom BM, Motaze SC, et al. Malaria infection in pregnancy and its effects on haemoglobin levels in women from a malaria endemic area of Fako Division, South West Province, Cameroon. J Obstet Gynaecol (Lahore) 25 (2005):235-40.
- World Health Organization. Malaria Microscopy Quality Assurance Manual Version 1. Geneva: WHO pres (2009):1-150.
- World Health Organisation. Haemoglobin concentrations for the diagnosis of anaemia and assessment of severity. Micronutrients Indicators. Geneva, Switzerland (2011).
- Sullivan D. Uncertainty in mapping malaria epidemiology: Implications for control. Epidemiol Rev. 32 (2010):175-87.
- Sari M, de Pee S, Martini E, Herman S, Sugiatmi, Bloem MW, et al. Estimating the prevalence of anaemia: a comparison of three methods. Bull World Heal Organ 79 (2001):506-11.
- Agan T, Ekabua JE, Udoh AE, Ekanem EI, Efiok EE, Mgbekem MA. Prevalence of anemia in women with asymptomatic malaria parasitemia at first antenatal care visit at the University of Calabar Teaching Hospital, Calabar, Nigeria. Int J Womens Health 2 (2010):229-33.
- Falade CO, Olayemi O, Dada-Adegbola HO, Aimakhu CO, Ademowo OG, Salako LA. Prevalence of malaria at booking among antenatal clients in a secondary health care facility in Ibadan, Nigeria. Afr J Reprod Health 12 (2008):141-52.
- Bardaji A, Martinez-Espinosa FE, Arevalo-Herrera M, Padilla N, Kochar S, Ome-Kaius M, et al. Burden and impact of Plasmodium vivax in pregnancy: A multi-centre prospective observational study. 4957 (2017):1-22.
- Savage EJ, Msyamboza K, Gies S, D’Alessandro U, Brabin BJ. Maternal anaemia as an indicator for monitoring malaria control in pregnancy in sub-Saharan Africa. BJOG An Int J Obstet Gynaecol. 114 (2007):1222-31.
- Melku M, Addis Z, Alem M, Enawgaw B. Prevalence and Predictors of Maternal Anemia during Pregnancy in Gondar, Northwest Ethiopia: An Institutional Based Cross-Sectional Study. Hindawi Publ Corp (2014):1-9.
- Oladeinde B, Omoregie R, Oladeinde O. Prevalence of HIV, HBV, and HCV infections among pregnant women receiving antenatal care in a traditional birth home in Benin City, Nigeria. Saudi J Heal Sci 2 (2013):113.
- Nkuo-akenji T, Tevoufouet EE, Nzang F, Fon E, Ebong IN. HIV / AIDS and malaria in pregnant women from Cameroon Short running title: HIV , malaria in pregnancy. Afr J Heal Sci 18 (2011):105-9.
- Erhabor O, Adias TC, Hart ML. Effects of falciparum malaria on the indices of anaemia among pregnant women in the Niger Delta of Nigeria. J Clin Med Res 2 (2010):35-41.
