Prevalence and Determinants of Arterial Hypertension among Patients with Ocular Diseases in South East Nigeria
Article Information
Arinze Anthony Onwuegbuna1, 2, Akunne Ijeoma Apakama1, 2 Chuka Michael Okosa1, 2, Emeka Akujuobi Chianakwalam2, Miriam-Benigna Chika Amobi2, Chisom God’swill Chigbo3, EjikeEkene Igboegwu2, Ekene Agatha
1Department of Ophthalmology, NnamdiAzikiwe University, Awka, Nigeria
2Guinness Eye Centre, Onitsha, Nigeria
3Department of Applied Microbiology, NnamdiAzikiwe University, Awka, Nigeria
4Department of Family Medicine, Faculty of Medicine, NnamdiAzikiwe University, Awka, Nigeria
5Department of Obstetrics and Gynecology, Faculty of Medicine, NnamdiAzikiwe University, Awka, Nigeria
6Department of Obstetrics and Gynecology, NnamdiAzikiwe University Teaching Hospital, Nnewi, Nigeria
*Corresponding author: George Uchenna Eleje, Department of Obstetrics and Gynecology, NnamdiAzikiwe University Teaching Hospital, Nnewi, Nigeria
Received: 17 August 2021; Accepted: 26 August 2021; Published: 09 October 2021
Citation: Arinze Anthony Onwuegbuna, Akunne Ijeoma Apakama, Chuka Michael Okosa, Emeka Akujuobi Chianakwalam, Miriam-Benigna Chika Amobi, Chisom God’swill Chigbo, Ejike Ekene Igboegwu, Ekene Agatha Emeka, George Uchenna Eleje. Prevalence and Determinants of Arterial Hypertension among Patients with Ocular Diseases in South East Nigeria. Fortune Journal of Health Sciences 4 (2021): 479-490.
View / Download Pdf Share at FacebookAbstract
Background: Most recent studies in Nigeria have documented high prevalence of ocular diseases among adults. Several mechanisms may link hypertension, dyslipidemia and obesity with ocular diseases. There are however no studies on the prevalence of arterial hypertension among the adults with ocular diseases. Objectives: To determine the prevalence and determinants of arterial hypertension among adult patients with ocular diseases and to justify the significance of routine blood pressure screening among adult patients in eye clinics.
Methods: A descriptive, cross-sectional study was conducted in eye clinics and community eye care out-reaches that offer primary, secondary and tertiary eye care services in Anambra State Nigeria. The primary outcome measure was the number of subjects with arterial hypertension. The pretested interviewer-administered self-administered semi-structured questionnaires were distributed amongst consenting adult patients. Data obtained were analyzed using the STATA version 16.0. Statistical Package for Social Sciences version 23. Statistical significance was set at p<0.05.
Results: Complete information was available for 455 (99.8%) of the subjects. The female: male ratio was 2:1 and the majority (35.41%) was between the ages of 63 and 77 years. The prevalence of arterial hypertension was 41.32% (188/455; 95% confidence interval (CI): 35.62– 47.67%). Arterial hypertension (p=0.004) and high cholesterol levels (p=0.001) were significantly higher in the urban subjects than in the rural subjects. Obesity (p<0.001), diabetes mellitus (p<0.001) and hypercholesterolemia (p=0.003) were significantly higher in the subjects with arterial hypertension than without arterial hypertension.
Conclusion: The prevalence of arterial hypertension was high in Nigeria among adult patients with ocular diseases. Its prevalence and dyslipidemia were signif
Keywords
Arterial hypertension; prevalence; adults; ocular diseases
Arterial hypertension articles, prevalence articles, adults articles, ocular diseases articles, Arterial hypertension articles Arterial hypertension Research articles Arterial hypertension review articles Arterial hypertension PubMed articles Arterial hypertension PubMed Central articles Arterial hypertension 2023 articles Arterial hypertension 2024 articles Arterial hypertension Scopus articles Arterial hypertension impact factor journals Arterial hypertension Scopus journals Arterial hypertension PubMed journals Arterial hypertension medical journals Arterial hypertension free journals Arterial hypertension best journals Arterial hypertension top journals Arterial hypertension free medical journals Arterial hypertension famous journals Arterial hypertension Google Scholar indexed journals prevalence articles prevalence Research articles prevalence review articles prevalence PubMed articles prevalence PubMed Central articles prevalence 2023 articles prevalence 2024 articles prevalence Scopus articles prevalence impact factor journals prevalence Scopus journals prevalence PubMed journals prevalence medical journals prevalence free journals prevalence best journals prevalence top journals prevalence free medical journals prevalence famous journals prevalence Google Scholar indexed journals adults articles adults Research articles adults review articles adults PubMed articles adults PubMed Central articles adults 2023 articles adults 2024 articles adults Scopus articles adults impact factor journals adults Scopus journals adults PubMed journals adults medical journals adults free journals adults best journals adults top journals adults free medical journals adults famous journals adults Google Scholar indexed journals ocular diseases articles ocular diseases Research articles ocular diseases review articles ocular diseases PubMed articles ocular diseases PubMed Central articles ocular diseases 2023 articles ocular diseases 2024 articles ocular diseases Scopus articles ocular diseases impact factor journals ocular diseases Scopus journals ocular diseases PubMed journals ocular diseases medical journals ocular diseases free journals ocular diseases best journals ocular diseases top journals ocular diseases free medical journals ocular diseases famous journals ocular diseases Google Scholar indexed journals STATA articles STATA Research articles STATA review articles STATA PubMed articles STATA PubMed Central articles STATA 2023 articles STATA 2024 articles STATA Scopus articles STATA impact factor journals STATA Scopus journals STATA PubMed journals STATA medical journals STATA free journals STATA best journals STATA top journals STATA free medical journals STATA famous journals STATA Google Scholar indexed journals Arterial hypertension articles Arterial hypertension Research articles Arterial hypertension review articles Arterial hypertension PubMed articles Arterial hypertension PubMed Central articles Arterial hypertension 2023 articles Arterial hypertension 2024 articles Arterial hypertension Scopus articles Arterial hypertension impact factor journals Arterial hypertension Scopus journals Arterial hypertension PubMed journals Arterial hypertension medical journals Arterial hypertension free journals Arterial hypertension best journals Arterial hypertension top journals Arterial hypertension free medical journals Arterial hypertension famous journals Arterial hypertension Google Scholar indexed journals hypercholesterolemia articles hypercholesterolemia Research articles hypercholesterolemia review articles hypercholesterolemia PubMed articles hypercholesterolemia PubMed Central articles hypercholesterolemia 2023 articles hypercholesterolemia 2024 articles hypercholesterolemia Scopus articles hypercholesterolemia impact factor journals hypercholesterolemia Scopus journals hypercholesterolemia PubMed journals hypercholesterolemia medical journals hypercholesterolemia free journals hypercholesterolemia best journals hypercholesterolemia top journals hypercholesterolemia free medical journals hypercholesterolemia famous journals hypercholesterolemia Google Scholar indexed journals
Article Details
1. Introduction
Arterial hypertension (AH) or elevated blood pressure is a global public health problem which causes serious morbidity and mortality [1]. About 1 in 4 men and 1 in 5 women have AH, two-thirds of them living in low and middle-income countries [1]. This means that over one billion people are estimated to be affected by AH globally [2]. Arterial hypertension is a major cause of premature death worldwide and unfortunately most of those affected with AH are not aware of the problem [1, 2].
The rising incidence of AH is thought to be due to increasing adult population and changing lifestyles [3, 4]. Also the socio- economic impact of AH and its complications are enormous [5]. In a resource poor country like Nigeria, the burden of AH is even worse where many live below two United State dollars per day [6].
A study of AH in Nigeria7 reported the prevalence of AH among the adult population to be between 6.2% to 48.9% for males and 10% to 47.3% for females using a level mark of 140/90 mmHg with males generally having a higher prevalence compared to females. This study also reported a higher prevalence of AH in the urban population, ranging from 17.5% to 51.6% in the urban areas and 4.6% to 43% in the rural areas [7].
In China, the country’s prevalence of hypertension among adults aged >18 years was 27.9% in 2015 compared to prevalence of 25.1% in 2012 [8]. This shows an increasing prevalence of AH. This study also reported a higher prevalence of AH among rural dwellers compared to urban dwellers [8]. The rates of awareness, treatment and control of adult hypertension in Chinese rural areas were all lower than those in urban regions during the same period [9]. In the US, about 45% of adults aged 20 years and above have arterial hypertension with 16% of those affected unaware that they have hypertension [10, 11].
There has been a report of high incidence of AH among patients with ocular diseases. A study in Greece reported an incidence of AH of up to 43.8% among cataract patients [12]. Similarly a multi-country study reported that 29.5% of 473 participants who had their blood pressure screened in the eye clinic had AH [13]. Another study conducted in an eye clinic in Saudi Arabia reported that 21% of 443 patients who had their blood pressure tested had AH, and 67.7% of those with AH were unaware of their high blood pressure status [14].
Arterial hypertension is a preventable cause of death in the world [1]. It produces cardiovascular risk by causing end-organ damage which also affects the eyes [15]. Posterior segment ocular manifestations of poorly controlled AH include optic neuropathy, retinopathy and choroidopathy [16].
Other ocular problems associated with uncontrolled AH include retinal vein occlusion, central retinal artery occlusion, cranial nerve palsies, non-arteritic anterior ischemic optic neuropathy, sub conjunctival hemorrhage and worsening of diabetic retinopathy among others [17].
Since many of those affected with AH are not aware of having the condition, early detection and consequent treatment will go a long way in preventing morbidity and mortality associated with this disease [1]. This involves taking blood pressure of the general population, especially adults at every given opportunity, like in eye clinics. The eye clinic has been reported by previous studies as a good place for routine screening of AH [13, 18]. The aim of the study was to determine the prevalence and determinants of arterial hypertension among adult patients with ocular diseases and to justify the significance of routine blood pressure screening among adult patients in eye clinics.
2. Methods
2.1 Study Design
A descriptive, cross-sectional study
2.2 Study Population
Patients attending eye clinics that offer primary, secondary, and tertiary eye care services to people within and outside the state, and also to people with ocular diseases in community eye care out-reaches conducted in 4 rural communities of Anambra State, Nigeria.
2.3 Study Site
Eye clinics and community eye care out-reaches that offer primary, secondary, and tertiary eye care services to people within and outside Anambra state, Nigeria.
2.4 Inclusion Criteria
All consenting new adult patients of ≥18 years that presented to the eye care facility and community eye care out-reaches.
2.5 Exclusion Criteria
Patients who presented in the hospital and community eye care out-reaches without documented eye disorder were excluded.
2.6 Sample Size Determination
The sample size was calculated using Kish and Leslie formula for cross sectional studies,n = z2p(1-p)/d2. Where: z = Z score for 95% confidence interval = 1.96, p = prevalence, d = tolerable error =5%. A prevalence of 65.8% was used as p for a previous study in Nigeria [19]. Consequently, the minimal sample size of the study population was 416 participants, calculated with 20% attrition. However, we consecutively recruited all adults with ocular disorders who were attending the eye clinic and out-reach program during the study period to increase the power of our study. Therefore a total of 456 adult patients who met eligible criteria and consented to participate in the study were recruited.
2.7 Sample Technique
Non-random sampling technique was employed.
2.8 Study Outcome Measures
The prevalence of AH among adult patients with ocular diseases as well as pattern of ocular diseases.
2.9 Patient Examination
All patients provided a detailed medical and ocular history. Detailed visual acuity, anterior segment and dilated posterior segment examinations including measurement of blood pressure and intraocular pressure were done. We used guidelines of the European Society of Cardiology/European Society of Hypertension which defines hypertension as blood pressure of 140/90 mmHg or greater [20]. Three consultant ophthalmologists performed standardized eye examinations on the patients. Those study participants needing further evaluationin the community out reaches were referred to the base tertiary eye hospital.
2.10 Procedures Involved and Data Collection
Data collection were done using a pretested, interviewer-administered, semi-structured questionnaire that captured the patients’ sociodemographics, patient’s hypertensive status, and duration of AH and treatment, family history of AH, smoking history, obesity, ocular and systemic complications of AH, and other co-morbidities like diabetes mellitus, dyslipidemia etc.
2.11 Data Quality Assurances
For quality assurance, the principal researcher was continuously supervising the data collectors for completeness and consistency and the records were cross-checked. The training was given for data collectors and supervisors. The data collection was supervised daily and it was pretested on 10% of the sample size. Based on the findings of the pre-test, some questions were modified and some others were added.
2.12 Data Processing and Statistical Analysis
All collected data were entered and cleaned by Excel spreadsheet. The cleaned data were exported to the STATA version 16.0, statistical software for analysis. Descriptive statistical measures such as mean ± Standard Deviation (SD) for continuous variables, and percentages were computed for categorical variables. Association between two independent categorical variables was assessed by using Chi-square or Fisher’s exact tests wherever applicable. The associations of continuous variables with two independent groups were analyzed by using independent t-tests. The effects of different independent variables on arterial hypertension were examined by univariate analysis. All the results were considered significant if the p-value was <0.05. Statistical analysis was performed using STATA 16.0, College Station, Texas, USA.
2.13 Ethical Consideration
Generally, our study followed the Declaration of Helsinki. Ethical clearance was obtained from the Chukwuemeka Odumegwu Ojukwu University Teaching Hospital Ethics Committee (Reference No. COOUTHWU/CMAC/ETH.C/VOL.1/FN:04/0102 and date of ethical approval obtained. 13/07/2021). All aspects of the study were conducted according to Good Clinical Practice and Good Laboratory Practice guidelines. The study in the four rural communities of Anambra State, Nigeria was approved by the respective town union leaders. Confidentiality of the study participants’ information was securely stored and identified by study number.
3. Results
Complete information was available for 455 (99.8%) of the subjects in the study. Table 1 shows the socio-demographic variables in the study population. The female: male ratio was 2:1. In terms of age distribution, the majority (35.41%) were between the ages of 63 and 77 years. This is shown in Figure 1. Table 2 shows the mean levels of SBP, DBP and pulse rate between the rural and urban study population. There was no significant difference in the mean systolic blood pressure (p=0.476), mean diastolic blood pressure (p=0.210) as well as mean pulse rate (p=0.478) and the type of residence of the subjects.
Table 1: Sociodemographic variables in the study population
|
Variable |
Frequency |
Percentage (%) |
|
Age (years) |
||
|
18-32 years |
43 |
9.58 |
|
33-47 years |
74 |
16.48 |
|
48-62 years |
146 |
32.52 |
|
63-77 years |
159 |
35.41 |
|
78-92 years |
25 |
5.57 |
|
93 years and above |
2 |
0.45 |
|
Sex |
||
|
Female |
282 |
61.84 |
|
Male |
174 |
38.16 |
|
Ethnicity |
||
|
Igbo |
449 |
98.46 |
|
Non-Igbo |
7 |
1.54 |
|
Educational level |
||
|
None |
49 |
10.79 |
|
Primary |
180 |
39.65 |
|
Secondary |
130 |
28.63 |
|
Tertiary |
95 |
20.93 |
|
Occupation |
||
|
Artisan |
63 |
13.82 |
|
Civil servant |
9 |
1.97 |
|
Clergy |
7 |
1.54 |
|
Dependent |
91 |
19.96 |
|
Farmer |
45 |
9.87 |
|
Professionals |
17 |
3.73 |
|
Retired |
22 |
4.82 |
|
Student |
21 |
4.61 |
|
Teacher |
18 |
3.95 |
|
Trader |
163 |
35.75 |
|
Location |
||
|
Rural |
293 |
64.25 |
|
Urban |
163 |
35.75 |
|
Total |
456 |
100 |
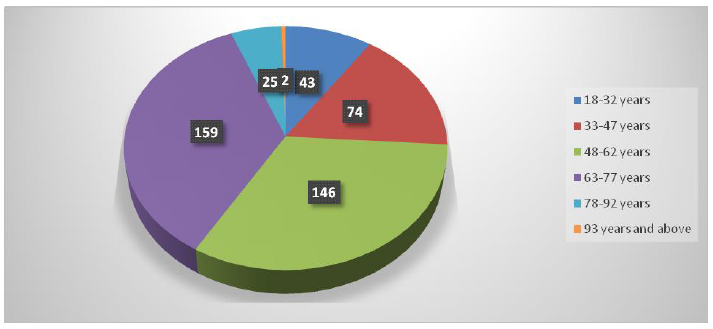
Figure 1: Age distribution among the study participants
Table 2: Showing the mean levels of SBP, DBP and Pulse rate between the rural and urban study population.
|
Variable |
Total |
Location (mean±SD) |
t-value |
p-value |
|
|
Rural (n=293) |
Urban (n=162) |
||||
|
SBP (mmHG) |
137.42±22.43 |
137.98±22.36 |
136.41±22.58 |
0.712 |
0.476 |
|
DBP (mmHG) |
86.65±13.97 |
87.26±11.99 |
85.55±16.97 |
1.253 |
0.210 |
|
Pulse/m |
69.32±8.91 |
69.09±9.70 |
69.80±7.02 |
-0.708 |
0.478 |
Abbreviations: SBP=Systolic Blood Pressure; DBP=Diastolic Blood Pressure
The prevalence of arterial hypertension in the study population (41.32% (188/455; 95% confidence interval (CI): 35.62– 47.67%)) is shown in Table 3, while the Table 4 and figure 2 show the prevalence of arterial hypertension according to the rural and urban study population. Arterial hypertension was significantly higher in the urban subjects than in the rural subjects (p=0.004).
Table 3: Prevalence of Family History of Hypertension among the study population
|
Hypertension |
Frequency |
Prevalence (%) |
|
Absent |
267 |
58.68 |
|
Present |
188 |
41.32 |
|
Total |
455 |
100.00 |
Table 4: Prevalence of Family History of Hypertension in the rural and urban study population
|
Variable |
Total |
Location (%) |
χ2-value |
p-value |
|
|
Rural (n=293) |
Urban (n=162) |
||||
|
Hypertension |
|||||
|
Absent |
267 (58.7) |
186 (63.7) |
81 (49.7) |
8.462 |
0.004* |
|
Present |
188 (41.3) |
106 (36.3) |
82 (50.3) |
||
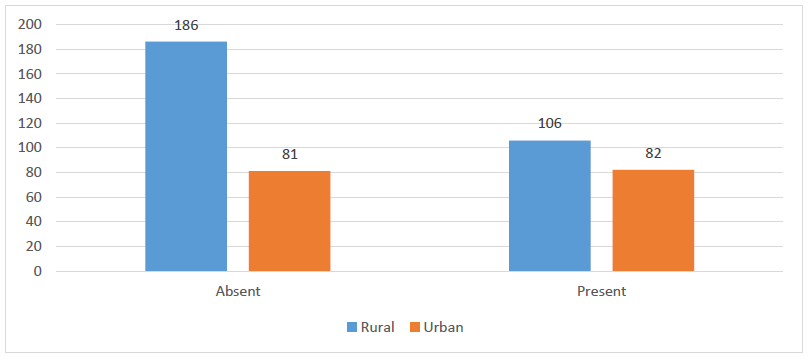
Figure 2: Hypertension in the rural and urban study population
Table 5 shows the smoking, obesity, diabetes, and cholesterol effects according to the rural and urban study population. Cholesterol levels were significantly higher in the urban subjects than in the rural subjects (p=0.001).
Table 6 shows the association between hypertension and smoking, obesity, diabetes mellitus, and cholesterol levels. Obesity (p<0.001), diabetes mellitus (p<0.001) and hypercholesterolemia (p=0.003) were significantly higher in the subjects with arterial hypertension than without arterial hypertension.
Table 5: Smoking, Obesity, Diabetes mellitus, and Cholesterol features in the rural and urban study population
|
Variables |
Total |
Location (%) |
χ2-value |
p-value |
|
|
Rural (n=293) |
Urban (n=162) |
||||
|
Smoking |
|||||
|
Absent |
448 (98.3) |
288 (98.3) |
160 (98.2) |
0.011 |
0.917 |
|
Present |
8 (1.7) |
5 (1.7) |
3 (1.8) |
||
|
Obesity |
|||||
|
Absent |
389 (85.3) |
251 (85.7) |
138 (84.7) |
0.084 |
0.772 |
|
Present |
67 (14.7) |
42 (14.3) |
25 (15.3) |
||
|
Diabetes mellites |
|||||
|
Absent |
388 (85.1) |
252 (86.0) |
136 (83.4) |
0.545 |
0.460 |
|
Present |
68 (14.9) |
41 (14.0) |
27 (16.6) |
||
|
Cholesterol |
|||||
|
Absent |
413 (90.6) |
275 (93.9) |
138 (84.7) |
10.366 |
0.001* |
|
Present |
43 (9.4) |
18 (6.1) |
25 (15.3) |
||
*=significant p-value<0.05
Table 6: Association between hypertension and smoking, obesity, diabetes mellites, and cholesterol
|
Variables |
Total |
Hypertension (%) |
χ2-value |
p-value |
|
|
Absent (n=267) |
Present (n=188) |
||||
|
Smoking |
|||||
|
Absent |
448 (98.5) |
262 (98.1) |
186 (98.9) |
0.476 |
0.490 |
|
Present |
7 (1.5) |
5 (1.9) |
2 (1.1) |
||
|
Obesity |
|||||
|
Absent |
388 (85.3) |
242 (90.6) |
146 (77.7) |
14.795 |
<0.001* |
|
Present |
67 (14.7) |
25 (9.4) |
42 (22.3) |
||
|
Diabetes mellites |
|||||
|
Absent |
387 (85.0) |
241 (90.3) |
146 (77.7) |
13.784 |
<0.001* |
|
Present |
68 (15.0) |
26 (9.7) |
42 (22.3) |
||
|
Cholesterol |
|||||
|
Absent |
412 (90.5) |
251 (94.0) |
161 (85.6) |
9.029 |
0.003* |
|
Present |
43 (9.5) |
16 (6.0) |
27 (14.4) |
||
*=significant p-value<0.05
4. Discussion
The motivation for this study was that systemic arterial hypertension has been linked to a wide range of major ocular diseases. This is because high arterial blood pressure decreases choroidal circulatory flow, increases intraocular pressure, and is associated with retinal micro vascular abnormalities and occurrence of retinal vein occlusion and retinopathy [21]. This study determined the up-to-date prevalence of arterial hypertension in adults with ocular diseases. The overall prevalence of arterial hypertension was 41.32% % (188/455; 95% CI: 35.62– 47.67%).Arterial hypertension (p=0.004) and high cholesterol levels (p=0.001) were significantly higher in the urban subjects than in the rural subjects. Obesity (p<0.001), diabetes mellitus (p<0.001) and cholesterol (p=0.003) were significantly higher in the subjects with arterial hypertension than without arterial hypertension.
The prevalence of arterial hypertension was higher than 29.4% reported by Varadaraj et al among patients visiting an eye clinics in multi-countries involving India, USA, UK, and China [13] and 30.3% (95% CI 26.1-34.8%) reported in a systematic review in Ghana by Atibila et al. [22],, but lower than 65.8% reported by Okoye et al in Enugu, Nigeria among obese individuals [19].
In this study, compared to rural settings, the burden of hypertension and high cholesterol levels in urban populations was significantly higher. This finding was similar to reports by Atibila et al in Ghana [22]. It is also similar to another study in Enugu, Nigeria [23]. In sub-Saharan Africa, rapid urbanization and changing lifestyles have modified the profile and pattern of various medical disorders including hypertension. On the contrary, a recent multi-country study concluded that hypertension is the most frequently observed cardiovascular disease risk factor in both urban and rural communities in multiple regions in sub-Saharan Africa and the determinants were consistently similar in both rural and urban study populations [24].
Serum lipid profile abnormalities are major predictors for coronary artery diseases. In this study, the prevalence of dyslipidemia among hypertensive patients was high. This finding was similar to a recent Ethiopian study by Kifle et al which documented those independent variables such as family history of hypertension, smoking, diabetes mellitus, and body mass index were significant determinants of dyslipidemia [25]. The high prevalence of dyslipidemia in this study could be due to sedentary physical activity, better socioeconomic status, and adjustment in the intensity of work, and high urbanization or dietary habits.
As shown in this study, obesity, diabetes mellitus and total cholesterol were significantly higher in the subjects with arterial hypertension than without arterial hypertension. Previous studies had also confirmed that diabetes mellitus and obesity increased the risk of dyslipidemia [26, 27]. Additionally, hypertensive patients with diabetes mellitus were at higher risk for having high levels of total cholesterol (AOR=1.71, 95% CI=1.21–2.91) when compared to patients who had not diabetes mellitus [25]. Similarly, participants who had a family history of hypertension were at higher risk for having high levels of total cholesterol (AOR=1.66, 95% CI=1.04–2.33) than respondents who had not hypertension [25].Thus, there is a need for targeted health education among adults to address the burden of obesity, dyslipidemia, and diabetes to reduce the burden of hypertensive heart disease in the individuals with already existing ocular diseases.
The major strength of the study is the large sample size of the study subjects. The study focused primarily on arterial hypertension, and all study subjects were examined by specialist ophthalmologists for accurate diagnosis of ocular disorders. The limitation of the study is that we were not able to assess other systems like glycosylated hemoglobin and echocardiography. These could have been useful for further risk factor assessment of ocular diseases. Those participants who required further examination were referred for further evaluation.
5. Conclusion
The prevalence of arterial hypertension was high in Nigeria among adult patients with ocular diseases. Its prevalence and dyslipidemia were significantly higher in the urban subjects than in the rural subjects. Obesity, diabetes mellitus and hypercholesterolemia were significantly higher in arterial hypertensives. There is a need for screening of arterial hypertension among subjects with ocular disorders as well as regular eye check-ups for early detection of vision threatening diseases to save the vision in the population.
6. References
- Brouwers S, Sudano I, Kokubo Y, Sulaica EM. Arterial hypertension. Lancet 398 (2021): 249-261.
- Jordan J, Kurschat C, Reuter H. Arterial Hypertension. DtschArztebl Int 115 (2018): 557-568.
- Kayima J, Wanyenze RK, Katamba A, Leontsini E, Nuwaha F. Hypertension awareness, treatment and control in Africa: a systematic review. BMC Cardiovasc Disord 13 (2013): 54.
- Heizhati M, Li N, Shi Q, Yao X, Zhang D, Zhou K, et al. Effects of Simplified Antihypertensive Treatment Algorithm on Hypertension Management and Hypertension-Related Death in Resource-Constricted Primary Care Setting between 1997 and 2017. Int J Hypertens (2021): 9920031.
- Kazibwe J, Tran PB, Annerstedt KS. The household financial burden of non-communicable diseases in low- and middle-income countries: a systematic review. Health Res Policy Syst 19 (2021): 96.
- Ilesanmi OS, Ige OK, Adebiyi AO. The managed hypertensive: the costs of blood pressure control in a Nigerian town. Pan Afr Med J 12 (2012): 96.
- Akinlua JT, Meakin R, Umar AM, Freemantle N. Current Prevalence Pattern of Hypertension in Nigeria: A Systematic Review. PLoS One 10 (2015): e0140021.
- Wang Z, Chen Z, Zhang L, Wang X, Hao G, Zhang Z, et al. Status of Hypertension in China: Results From the China Hypertension Survey, 2012-2015. Circulation 137 (2018): 2344-2356.
- Ma WJ, Tang JL, Zhang YH, Xu YJ, Lin JY, Li JS, et al. Hypertension prevalence, awareness, treatment, control, and associated factors in adults in southern China. Am J Hypertens 25 (2012): 590-6.
- Barszczyk A, Yang D, Wei J, Huang W, Feng ZP, Lee K, Luo H. Potential Impact of the 2017 High Blood Pressure Guideline Beyond the United States: A Case Study of the People's Republic of China. Am J Hypertens 33 (2020): 846-851.
- Benjamin EJ, Virani SS, Callaway CW, Chamberlain AM, Chang AR, Cheng S, et al. Heart Disease and Stroke Statistics-2018 Update: A Report From the American Heart Association. Circulation 137 (2018): e67-e492.
- Mylona I, Dermenoudi M, Ziakas N, Tsinopoulos I. Hypertension is the Prominent Risk Factor in Cataract Patients. Medicina (Kaunas) 55 (2019): 430.
- Varadaraj V, Vardhan A, Mudie LI, LaBarre S, Ong Y, Wang B, Sherrod C, Friedman DS. Uncontrolled Hypertension Is Common in Glaucoma Clinics. Am J Hypertens 32 (2019): 88-93.
- AlAnazi SA, Osuagwu UL, AlMubrad TM, Ahmed HK, Ogbuehi KC. Effectiveness of in-office blood pressure measurement by eye care practitioners in early detection and management of hypertension. Int J Ophthalmol 8 (2015): 612-21.
- Suvila K, McCabe EL, Lehtonen A, Ebinger JE, Lima JAC, Cheng S, Niiranen TJ. Early Onset Hypertension Is Associated With Hypertensive End-Organ Damage Already by MidLife. Hypertension (2019).
- Lee WH, Park JH, Won Y, Lee MW, Shin YI, Jo YJ, et al. Retinal Microvascular Change in Hypertension as measured by Optical Coherence Tomography Angiography. Sci Rep 9 (2019): 156.
- Chen X, Liu L, Liu M, Huang X, Meng Y, She H, et al. Hypertensive Retinopathy and the Risk of Stroke Among Hypertensive Adults in China. Invest Ophthalmol Vis Sci 62 (2021): 28.
- Adji A. Eye Clinic as a Potential Site to Measure Blood Pressure. Am J Hypertens 32 (2019): 12-14.
- Okoye I, Ezeala-Adikaibe BA, Mbadiwe N, Onodugo OD, Anyim OB, Ijoma UN, et al. Prevalence and distribution of hypertension in overweight and obese subjects in an urban community in Enugu, South East Nigeria. A post hoc analysis. Niger J ClinPract 23 (2020): 1566-1571.
- de la Sierra A. New American and European Hypertension Guidelines, Reconciling the Differences. Cardiol Ther 8 (2019): 157-166.
- Katsi V, Marketou M, Vlachopoulos C, Tousoulis D, Souretis G, Papageorgiou N, et al. Impact of arterial hypertension on the eye. CurrHypertens Rep 14 (2012): 581-90.
- Atibila F, Hoor GT, Donkoh ET, Wahab AI, Kok G. Prevalence of hypertension in Ghanaian society: a systematic review, meta-analysis, and GRADE assessment. Syst Rev 10 (2021): 220.
- Ezeala-Adikaibe BA, Orjioke C, Ekenze OS, Ijoma U, Onodugo O, Okudo G, et al. Population-based prevalence of high blood pressure among adults in an urban slum in Enugu, South East Nigeria. J Hum Hypertens 30 (2016): 285-91.
- Hendriks ME, Wit FW, Roos MT, Brewster LM, Akande TM, de Beer IH, et al. Hypertension in sub-Saharan Africa: cross-sectional surveys in four rural and urban communities. PLoS One 7 (2012): e32638.
- Kifle ZD, Alehegn AA, Adugna M, Bayleyegn B. Prevalence and predictors of dyslipidemia among hypertensive patients in Lumame Primary Hospital, Amhara, Ethiopia: A cross-sectional study. Metabol Open 11 (2021): 100108.
- Jeenduang N, Whanmasae S, Seepawin P, Kullabootr S. The prevalence of dyslipidemia among a rural Thai population in the Nakhon Si Thammarat province. J Med Assoc Thai 96 (2013): 992-1000.
- Cai L, Zhang L, Liu A, Li S, Wang P. Prevalence, awareness, treatment, and control of dyslipidemia among adults in Beijing, China. J AtherosclerThromb 19 (2012): 159-68.
