Pre-operative Embolization Facilitating the Surgical Resection of Retroperitoneal Paraganglioma Associated to Horseshoe Kidney
Article Information
A.Abdou1, O. Almaghraoui2*, K. Moufid3, M. Alaoui2
1Cardiovascular surgery department, Avicenna military hospital, Marrakech, Morocco
2Vascular surgery department, Avicenna military hospital, Marrakech, Morocco
3Urology department, Avicenna military hospital, Marrakech, Morocco
*Corresponding author: Oussama Almaghraoui, Vascular surgery department, Avicenna military hospital, Marrakech, Morocco
Received: 02 December 2019; Accepted: 09 December 2019; Published: 08 December 2020
Citation: A. Abdou, O. Almaghraoui, K. Moufid, M. Alaoui. Pre-operative Embolization Facilitating the Surgical Resection of Retroperitoneal Paraganglioma Associated to Horseshoe Kidney. Cardiology and Cardiovascular Medicine 4 (2020): 746-752.
View / Download Pdf Share at FacebookAbstract
The authors report the successful removal of a paraganglioma associated with horseshoe kidney after preoperative embolization and two previous failed surgical attempts undergone in another center. Complete excision of the tumour was performed smoothly. Total blood loss was 205 ml and the surg-ical time was approximately 160 minutes. The posto-per-ative period was uneventful. Histological findings were of paraganglioma, and there was no surgical margin. This case emphasizes the necessity to include preoperative embolization in the manage-ment of difficult or inextirpable retro-peritoneal para-ganglioma and should be considered in difficult case.
Keywords
Embolization; Surgery; Paraganglioma
Embolization articles; Surgery articles; Paraganglioma articles
Article Details
1. Introduction
Arising from extra-adrenal chromaffin tissues, paraganglioma remains rare tumors ranging in incidence from 0.005% to 0.1% in the general population. Surgical excision is the treatment of choice for both primary and recurrent tumours [1, 2]. The Authors report a case with a rich icono-graphy of a voluminous abdominal paragang-lioma that is associated with horseshoe kidney in which pre- operative embolization therapy was an alternative potentially enabling local control with less morbidity. Here we report that such case successfully treated by trans arterial embolization (TAE). This case highlights the need for preoperative embolization as part of the multi-disciplinary approach to the management of paragangliomain difficult anatomical locations by the surgeon and could suggest new modalities of treatment of this entity.
2. Case Report
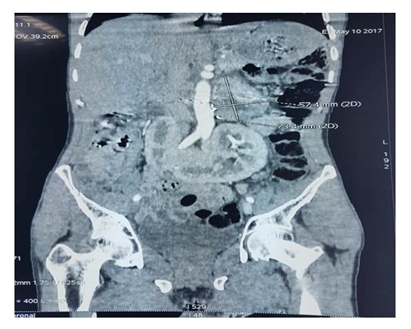
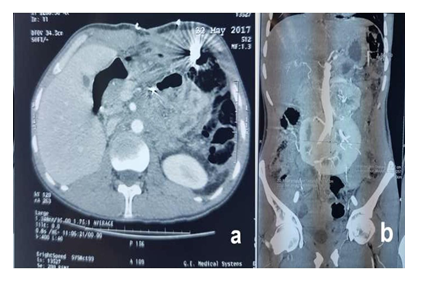
A 39-year-old man was referred from another urological centre for “inextirpable” functional retroperitoneal tumour (Figure 1).Measurements of plasma and urinary catecholamine and urinary total metanephrines ruled in the diagnosis with diabetes and hypertension. The month before his admission he has undergone two failed surgical attempts in another center to remove the lesion. A laparoscopic approach was attempted at first but was aborted due to dense adhesion between tumor and great vessels (Figure 2). Ten days later, an open procedure was subsequently performed unsuccessfully. Unexpectedly at laparotomy, despite adequate pre-operative imaging, once again the tumor was unable to be resected due to hemorrhage. A Planned blockage of blood vessels was then decided. Trans femoral access is obtained and a 5 Fr sheath is placed. A 5 Fr diagnostic catheter is then advanced into the artery on the left side of the tumor and angiography is performed to determine the arterial feeders of the tumor. Angiography showed three arteries with one dominant feeding artery arising from the left side of aortic artery (Figure 3a). Selective angiography was performed 2 days before the surgical removal of the tumor, and the feeding artery was successfully embolized with 3steel coils (Terrumo ®). Follow-up imaging revealed that devascularisation of at least 60% of the initial tumor blush was obtained (Figure 3b).
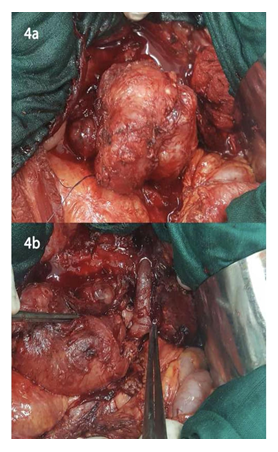
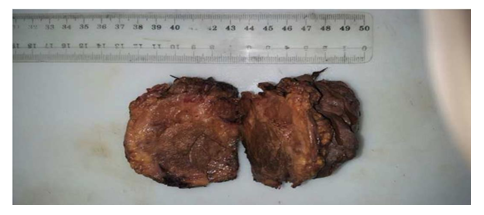
The patient then underwent surgical management by a bilateral subcostal approach. Per-operative exploration found a retroperitoneal tumor of about 07 cm in diameter that was soft and encapsulated. On exploration, there was a large blood supply by a 12 mm arterial rising directly from lateral side aorta. Complete excision of the tumor was performed smoothly after dissection along the basement (Figure 4 a, b). Total blood loss was 205 ml and the surgical time was approximately 160 minutes. The postoperative period was uneventful. His pre-operative symptoms improved, and he was discharged home one week after. At 6-months follow-up there was no recurrence of his symptoms. Histological findings were of paraganglioma, with negative surgical margin confirmed by postoperative histopathology (Figure 5).
3. Discussion
Although described for the first time in 1886, the diagnosis of PGL remains a challenge, because patients do not present with characteristic signs and symptoms [1-3]. A paraganglioma may be discovered in the absence of any symptom. For patients with functional tumor the most common type of presenting symptom was the classic triad of symptoms associated with catecholamine-secreting para-ganglioma: episodic headache, diaphoresis and tachycardia. The surgical removal of a tumor can often be in theory made easier if the blood supply to the mass is decreased prior to surgeryand allowing better visualization [3-5]. Laparoscopic resection of PG is considered challenging because of the altered anatomic location, dense peritumoral adhesions, high vascularity envelope, and proximity to major blood vessels [5, 6]. In our case, the anatomic alterations were majored with the association with a horseshoe kidney. Horseshoe kidneys are different in three main ways: location, orientation, and vasculature showing a greater variation in the origin and number of renal arteries and veins. Horseshoe kidney is the most common congenital renal fusion anomaly with an incidence of 1 in 400-600 individuals [7].
The pre-operative embolization of hyperactive vascular tumours is often performed to decrease intraoperative blood loss and facilitate tumor resection but its use in abdominal PG is controversial and still matter of debate [4, 5]. Conflicting data have been reported on the benefit of embolization, although the literature is limited to small single-centers series and case reports [3, 4, 6]. Several techniques concerning gloms tumor embolization via the endovascular route (arterial, venous, or combined) or through direct percutaneous puncture have been previously described in the literature. Therapeutic embolization is not free of risks: such procedures have an 8% rate of morbidity and a 2.5% rate of overall mortality but remains generally a safe procedure and most authors report low complication rates [5, 8]. Commonly used particles include gelatin sponge, polyvinyl alcohol (PVA), trys-acryl gelatin microspheres or coils. Prior identification of all possible anastomoses is important before the injection of such agents.
The resection of retroperitoneal paraganglioma presents a distinct challenge because the procedure can be associated with massive intraoperative blood losses. In 2016, XIAO-KE et al reported a large panel of 34 RPG in whom a patient with 7500 ml of blood loss during the removal of RPP and adjacent organ resection was required in 7 (21%) cases [9]. Few authors have reported using embolization as a useful presurgical adjunct for routine approach of paraganglioma [3, 10]. Apentcheko et al described a similar case in a 17 year old girl treated with partial embolization prior to surgery [11]. However, despite a blood loss of 50 cc and a surgical time estimated to 160 min, the authors conclude that inherent increased cost, potential risk during embolization cannot be recommended as a pre operative adjunct and should be only recommended for hype-vascularized tumor or when size is superior to 4 cm. Rosing et al has performed the same pre operative approach for a 12, 5 cm paraganglioma [12]. In both case, patients had undergone complete resections without complications or significant bleeding. Many authors reports same cases [13, 14]. In addition, Di Daniele et al reported a pelvic paraganglioma in young female patient successfully removed after initial TAE and marked decrease of circulating catecholamine`s levels [15]. To our knowledge, there are only two reported cases of RPG associated with horseshoe kidney and the only one managed with preoperative embolization [13, 14].
4. Conclusion
This case emphasizes the necessity to include preoperative embolization in the management of difficult or inextirpable retroperitoneal para-ganglioma and should be considered in difficult case. Additional studies with larger sample sizes and long-term follow- ups are required to validate the benefits of preoperative approach but small patient numbers make prospective trials difficult to conduct on this topic.
Conflicting Interests
The Authors declare that there is no conflict of interest.
Consent Statement
Informed consent has been obtained from the patient for publication of the case report and accompanying images.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for- profit sectors.
References
- Fliedner SM, Lehnert H, PacakK. Metastatic paraganglioma. Semin Oncol 37 (2010): 627-637.
- Lac E E. Tumors of the Adrenal Gland and Extra-adrenal Paraganglia In: Atlas of Tumor Pathology, Third Series, Fascicle 19, Armed Forces Institute of Pathology, Washington, DC, (1997).
- Xu W, Li H, Ji Z, Yan W, Zhang Y, Zhang X, et al. Retroperitoneal Laparoscopic Management of Paraganglioma: A Single Institute Experience. PLoS ONE 11 (2016): e0149433.
- Kang SW, Kandil E, Kim MJ, Kim KS, Lee CR, Jeong JJ, et al. Posterior Retroperitoneoscopic Resection of Extra-adrenal Paraganglioma Located in the Aorto-caval Space. Ann SurgOncol (2018).
- Jackson RS, Myhill JA, Padhya TA, McCaffrey JC, McCaffrey TV, Mhaskar RS. The Effects of Preoperative Embolization on Carotid Body Paraganglioma Surgery: A Systematic Review and Meta-analysis. Otolaryngol Head Neck Surg 153 (2015): 943-950.
- Kassahun WT. Update on the optimal management of patients with vascular extension of pheochromocytoma.Vascular 23 (2015): 297-304.
- Sheng Tai, Jianzhong Wang, Jun Zhou, Zongyao Hao, Haoqiang Shi, Yifei Zhang, et al. The Robotic-Assisted Laparoscopy, Isthmusectomy, and Pyeloplasty in a Patient With Horseshoe Kidney: A Case Report. Medicine (Baltimore) 95 (2016).
- Romaric Loffroy, Pramod Rao, Byung-Kook Kwak, Shinichi Ota, Ming De Lin, Eleni Liapi, et al. Transcatheter Arterial Embolization in Patients with Kidney Diseases: an Overview of the Technical Aspects and Clinical Indications. Korean J Radiol 11 (2010): 257-268.
- Xiao-Ke Ji, Xiang-Wu Zheng, Xiu-Lin Wu, Zheng-Ping Yu, Yun-Feng Shan, Qi-Yu Zhang, et al. Diagnosis and surgical treatment of retroperitoneal paraganglioma: A single-institution experience of 34 cases. Oncol Lett 14 (2017): 2268-2280.
- Ji XK, Zheng XW, Wu XL, Yu ZP, Shan YF, Zhang QY, et al. Diagnosis and surgical treatment of retroperitoneal paraganglioma: A single-institution experience of 34 cases. Oncol Lett 14 (2017): 2268-2280.
- Natalia Apentchenko Eriutina, Camilo J Castellón Pavón, Carlos García Vásquez, Irene Gonzalo Montesinos, Santos Jiménez de los Galanes, Pedro A. Pacheco Martínez, Juan Gómez Patiño. Retroperitoneal paragan-glioma-Is pre operative embolization useful?. Int J Surg Case Rep 39 (2017): 64-68.
- Rosing JH, Jeffrey RB, Longacre TA, Greco
- Massive extra-adrenal retroperitoneal paraganglioma: pre-operative embolization and resection. Dig Dis Sci 54 (2009): 1621-1624.
- Iashin NP, Egorova TM. Extraorganic retroperitoneal paraganglioma associated with a horseshoe kidney. Urol Nefrol (1986): 63-64.
- Eduardo de Paula Miranda, Roberto Iglesias Lopes, Guilherme Philomeno Padovani, Paulo Renato Marcelo Moscardi, Fernanda Gardini Maciel Nishimura, Berenice Bilharinho de Mendonça, et al. Malignant paraganglioma in children treated with embolization prior to surgical excision. World J Surg Oncol 14 (2016): 26.
- Di Daniele N, Canale MP, Tesauro M, Rovella V, Gandini R, Schillaci O, et al. Preoperative embolization reduces the risk of cathecolamines release at the time of surgical excision of large pelvic extra-adrenal sympathetic paraganglioma. Case Rep Endocrinol 2012 (2012): 481328.