Pre-Gestational Obesity and its Impact on Neonatal Morbidity and Mortality at Ehs “Nouar Fadela”
Article Information
Bouabida D*, Zelmat S, Belalaoui I
Faculty of Medicine, Oran University, Es Senia, Algeria
*Corresponding Author: Bouabida D, Faculty of Medicine, Oran University, Es Senia, Algeria
Received: 03 May 2020; Accepted: 14 June 2020; Published: 02 November 2020
Citation:
Bouabida D, Zelmat S, Belalaoui I. Pre-Gestational Obesity and its Impact on Neonatal Morbidity and Mortality at Ehs “Nouar Fadela”. Journal of Pediatrics, Perinatology and Child Health 4 (2020): 117-125.
View / Download Pdf Share at FacebookAbstract
Maternal obesity has become an important global public health problem and is responsible for neonatal morbidity and mortality.
Objective: to study the influence of maternal obesity on birth weight and neonatal complications.
Material and Methods: This is a cross-sectional study covering 664 files of mother-child couples, i.e., (324: 48.8% macrosomes and 340: 51.2% eutrophic) collected between January 1, 2015 to December 31, 2015. We we analyzed and compared the weights of newborns born to parents with or without overweight. The calculation of the body mass index [BMI] = P/T2 in kg/m2) had made it possible to classify parental corpulence according to the recommendations of the World Health Organization (WHO). The logistic regression analysis was been carried out.
Results: We recorded 4526 deliveries of which 664 or 324 (48.8%) macrosomes and 340 (51.2%) eutrophic) mother-newborn pairs were included in the study. Maternal pre-gestational overweight was significantly related at neonatal macrosomia (p<0.0001).
Conclusion: Excess weight has become a major public health problem worldwide. There is a positive correlation between newborn weight and maternal build before conception explaining the increased risk of fetal macrosomia in women with overweight. These data highlight the value of following recommendations for weight gain during pregnancy.
Keywords
Birth Weight, Macrosomia, Brachial Plexus Palsy, Mothers Overweight, Gestational Diabetes, Obesity
Birth Weight articles; Macrosomia articles; Brachial Plexus Palsy articles; Mothers Overweight articles; Gestational Diabetes articles; Obesity articles
Article Details
1. Introduction
Maternal excess weight has become a significant global public health problem.It is responsible for maternal-fetal morbidity and mortality.There is a positive correlation between newborn weight and maternal build before conception explaining the increased risk of fetal macrosomia in women with overweight.The World Health Organization (WHO) considers obesity to be a pandemic that affects both industrialized and developing countries. In 2014, excess weight affected more than 1.9 billion adults, including over 600 million were obese.In Algeria, overweight: 12% children under five and 18% between 12-23 months[1]. On the obstetrical level, the pregnancy of overweight women is more frequently marked by maternal and neonatal complications, also notingthat obesity in childbearing age varies between 6% and 15.5% and that from the age of 18 at 44 years old and the proportion of macrosomes varies between 15 and 30%.(Multiple Indicator Cluster Survey (MICS) 2012-2013). From these global literature data, the main objective of our work was tostudy the influence of excess pre-gestational maternal weight on the birth weight of a population of term newborns. And secondly to describe the maternal characteristics and to evaluate the neonatal morbidity and mortality.
2. Patients and Methods
This is a cross-sectional, descriptive and analytical study nested in the cohort of pregnant women who gave birth during the study period at the level of the neonatal service “EHS Nouar Fadéla” (Ex. Ste Anne).During the period from January 1 to December 31, 2015 inclusive,
● Inclusion criteria: We included in our study any mother-newborn couple whose gestational age varies between 37 and 42 weeks of amenorrhea (SA) and a birth weight>50th percentile for gestational age.
● Non-inclusion criteria:We excluded from this study all premature infants less than 37 weeks old.
We have developed survey forms that have been carefully completed through an interrogation with the mother, these include three parts:
- Maternal characteristics (age, occupation, marital status, socio-economic level, parity, pregnancy, obstetric history: abortion, stillbirth, previous diabetes, diabetes, pregnancy).
- Characteristics of the current pregnancy and childbirth (weight at the beginning and end of pregnancy; pre-gestationalweight, weight gain), maternal height, blood pressure, screening for diabetes (hypoglycemia, glycated hemoglobin, venous glycemia); monitoring of pregnancy, history of macrosomia) and newborn characteristics (weight, height, bw) and neonatal complications.
2.1 Definition of terms
- Macrosomia
● A birth weight greater than 4000 or 4500 grams is a simple index, but which does not take into account gestational age.
● A birth weight above the 90th percentile for gestational age compensates for this defect.Gender, ethnicity and geographic environment influence birth weight, requiring the use of reference curves for each population.
- The weight index(weight * 100/height3) is easy to calculate, not influenced by ethnicity and sex and reference curves constructed according to gestational age allow a classification of macrosomia into two distinct groups:
● Non-segmental macrosomes, the weight index of which is less than the 90th
● Segmental macrosomes, the weight index of which is greater than the 90th percentile (newborn baby of a diabetic mother).
A pregnancy is said to be followed: if the mother has had three antenatal consultations.
● Perinatal asphyxiais retained if the APGAR score has remained below 7 to five minutes of life.
● Hypoglycemia: is defined by a blood glucose lower than 0.30 g/L on the first day and lower than 0.45 g/L beyond 24 hours.Capillary blood glucose tests are systematically performed in macrosome newborns at one hour of life.In the event of normal initial blood sugar levels, the newborn is put to the breast, monitored in the maternity ward next to his mother, the capillary blood sugar level is redone at three hours of life before the next breastfeeding, then every six hours for the first 24 hours. hours.If the initial blood sugar is low, the newborn is hospitalized for treatment.
2.2 Statistic study
Data entry as well as descriptive and analytical data analysis were performed using Statistical Package for Social Sciences (SPSS) version 20. Quantitative variables were presented as mean and standard deviation, qualitative variables expressed as a percentage.Chi testwas used for comparison of results.The cutoff of p<0.05 was considered statistically significant.
3. Result
During the period from January 1 to December 31, 2015 inclusive, 4,526 deliveries were carried out. We collected 664 mother/newborn couples who were the subject of this study, including 324 NN-MERES couples who were overweight and 340 newborns-mothers of normal weight.
3.1 Maternal characteristics
● The average age in our sample was: 30.60 ± 6 years.The predominant age group was between 26 and 35 years with a rate of 59.1% in mothers of macrosome newborns vs. 53.2% in mothers of eutrophic newborns.
● Maternal height varied between 145 cm and 175 cm.The average height in our sample was: 163 ± 6 163.85 ± 6.4 cm.
● Multiparity was observed in 50% of overweight mothers vs. 67% of newborns of normal weight mothers.
● the distribution of mothers in our study population according to BMI shows that more than 50% were normal weight, 21.8% overweight and 30% obese.
● Considering 15 kg as the limit weight gain during pregnancy, 15% of the overweight newborns were found to have had excessive weight gain with a well-known prior weight.
● The most marked antecedents and respectively in pregnant women with excess weight versus normal weight are: antecedent of macrosomia, MIU, HTA, Abortion;diabetes and weight gain with a significant difference (Table 1).
● 42.1% of pregnant women who were overweight had been screened for diabetes and only 12.5% were followed up during their pregnancy (PMI follow-up or private doctor).
3.2 Evolution of labor and decision of the mode of delivery
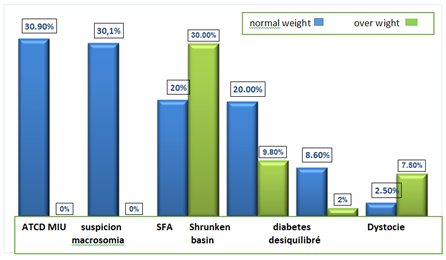
The majority of deliveries of macrosome newborns were by the high route (74% vs. 26% by the base route).Certain indications for caesarean section such as ATCD MIU, the suspicion of macrosomia, narrowed pelvis and unbalanced diabetes predominate in pregnant women who are excessively overweight vs pregnant women of normal weight (figure 1).
3.3 Features of newborns
● Gender: The male predominance is among the NN overweight mothers with a rate equal to 72.9%.
● Weight and gestational age: The birth weight (PNN) varied between 4000 g and 5900 g with an average PNN of: 4075 ± 346 g vs the birth weight of the controls varied between 2380 g and 3800 g with an average PNN of: 3535 ± 271 gr. The mean head circumference of newborns from overweight mothers was: 35.82
± 1.26 cm vs. controls was 34 ± 1.10 cm.The mean size of the macrosome newborns was: 51 ± 2.31 cm vs the controls was 48.7 ± 2.12 cm.
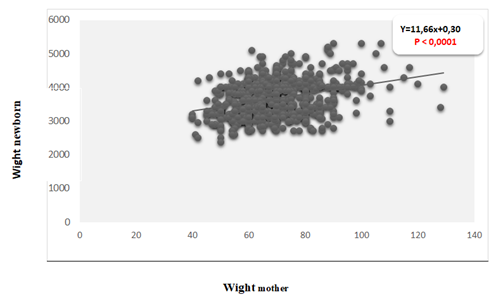
3.4 Correlation between maternal weight and birth weight in the two populations of newborns
The correlation between maternal weight and birth weight shows that whatever the weight of the newborn, their birth weight increases simultaneously with the body mass index of their mothers, The coefficient of determination being positive, it confirms the correlationpositive between the weight of the mother and the weight of the newborn(figure 2).
3.5 Neonatal complications
Neonatal morbidity in newborns of overweight mothers is dominated respectively by: hypoglycemia in 19.3%;hematomas in 3.8%;brachial plexus palsy in 2.1%.Lethality is noted in 0.9% of cases.Becoming newborns: 66% were given to their mothers and 34% newborns were hospitalized (Table 2).
|
Mother's BMI (Kg/m2) |
664 Mother-Newborn Couples |
|
|
NOT |
% |
|
|
Normal (18.5 <BMI <24.9 kg/m2) |
340 |
51.2 |
|
Excess weight (25-29 kg/m2) |
145 |
21.8 |
|
Obese (≥30 kg/m2) |
179 |
26.9 |
Table 1: Distribution of mothers according to BMI.
|
Mothers characteristics |
Excess weight N = 324 |
Normal weight N = 340 |
OR [95% CI] |
Meaning threshold p |
|
% |
% |
|||
|
Abortion |
18 |
10 |
1.85 [1.6-2.2] |
<0.1 |
|
Miu |
6 |
2 |
2.6 [1.29-5.5] |
<0.1 |
|
Gestational Diabetes |
18 |
10 |
1.88 [0.9-1.9] |
<0.1 |
|
HTA |
20 |
9 |
2.47 [0.9-5.6] |
<0.001 |
|
Atcd macrosomia |
32 |
15 |
2.6 [1.04-5.7] |
<0.001 |
|
Term> 42 (sa) |
5 |
4 |
Ns |
Ns |
|
Multiparity |
50 |
67 |
1.07 [0.9-1.4] |
<0.001 |
|
Weight gain |
15 |
2 |
0.8 [0.4-1.1] |
<0.05 |
Table 2: Maternal medical history.
|
Neonatal complications |
Macrosomes |
Meaning threshold P |
|
|
Yes NOT (%) |
No NOT (%) |
||
|
Hypoglycemia (<0.40 gr/l) |
82 (19.3) |
49 (10.6) |
<0.0001 |
|
Hypocalcaemia (<80 mg/l) |
7 (1.6) |
16 (3.4) |
NS |
|
Hyperbilirubinemia |
45 (10.6) |
115 (24.8) |
<0.0001 |
|
Polycythemia |
1 (0.2) |
2 (0.4) |
NS |
|
Perinatal asphyxia (APN) |
23 (5.4) |
45 (9.7) |
NS |
|
Respiratory distress |
42 (9.9) |
124 (26.7) |
<0.0001 |
|
Hypertrophic cardiomyopathy (CMH) |
3 (0.7) |
4 (0.9) |
NS |
|
Brachial plexus palsy (PPB) |
9 (2.1) |
1 (0.2) |
0.007 |
|
Clavicle fracture |
3 (0.7) |
1 (0.2) |
NS |
|
Humeral fracture |
5 (1.2) |
0 (0) |
- |
|
Serum blood lump |
37 (8.7) |
58 (12.5) |
NS |
|
Hematomas |
16 (3.8) |
9 (1.9) |
NS |
|
Death |
5 (0.9) |
3 (0.6) |
NS |
Table 3: Distribution of neonatal morbidities.
4. Discussion
4.1 The prevalence of obesity and overweight
In our study, it was 21.8% overweight and 26.9% obese, respectively. Some results of studies are similar to ours and others are different.This percentage difference may be due to the increase in the frequencies of maternal diabetes and to the very different eating habits and lifestyle of each country especially between developed and developing countries[1-6].
4.2 Pathologies of pregnancy and characteristics of childbirth
● We found 15% of patients who were over pre-pregnancy weight who gained excessive weight during pregnancy.Some study results are similar to ours and others are different.Excessive weight gain would be responsible for a modification of maternal metabolism because it is dependent on food, thus explaining macrosomia by anabolism[2].
● The average age of mothers in our sample was 30 ± 5.7 years, which is almost identical in some studies.However, other authors describe a younger population.Exceeding the term was significantly observed in pregnant women who were overweight.This can be explained by: lack of an early ultrasound for dating the pregnancy imprecision of the dates of the last menstruation and the irregular nature of prenatal consultations.
● The proportions of multiparas were higher in normal weight mothers than in overweight mothers (67% and 50%) respectively and the difference is significant.Regardless of the type of diabetes, our results match those of the literature, but the percentage of gestational diabetes in our series is high compared to the data in the literature.This can be explained above all by the ethnic and genetic variations of populations, but also, to a lesser extent, by the diversity of strategies and screening methods used[7-9].
● The history of macrosomia is the most implicated factor in the occurrence of macrosomia.Its pathophysiology has not yet been elucidated. This confirms that a woman who has given birth to a macrosome most often recurs with a risk multiplied by six (OR = 6) and in our series, this is multiplied by[10-12].
● Male predominance has been reported by most authors.with a relative risk multiplied by 2 and our results agree with most studies.For this, hypotheses have been proposed to explain why girls are born lighter than boys.Wilkin and Murphy have suggested that gender-specific genes affecting insulin sensitivity are responsible for the gender difference in birth weight.According to them, the female fetus is genetically more resistant to insulin and less sensitive to the trophic effects of insulin and is therefore smaller[11-13].
4.3 Childbirthtype
● Our results show that obese and overweight pregnant women are more at risk of giving birth by caesarean section with a statistically significant association.Our results agree with those of the literature.The risk of cesarean section in these women would be related to the higher risk of preeclampsia, fetal macrosomia and dynamic obstructed labor.In our study, the indications for caesarean section were varied and dominated by the suspicion of macrosomia and a history of in utero death[10, 14, 15].
● Regarding neonatal morbidity, the frequency of macrosomia increases with BMI. Several studies have shown that overweight women, especially obese women, were more frequently at risk of giving birth to macrosome newborns.This percentage difference may be due to the food character of each country, especially between developed and developing countries[1-3].
● Hypoglycemia was observed in 19.3% of newborns born to overweight mothers;this is higher than that observed by most of the authors.There is a linear relationship between birth weight and shoulder dystocia and PPB. Birth trauma was greater in the group of overweight mothers compared to controls (deep hematomas 3.8%, PPB 2, 1%, humeral fracture 1.7%) with a significant link. Our results agree with most of the studies.Neonatal mortality was greater in newborns of overweight mothers (5 cases: 0.9%);our resultsagree withmost studies, this could be explained by the fact that most pregnancies were not followed[8, 16-19].
5. Conclusion
Pregnancy in overweight women must therefore be considered “at risk”, regardless of maternal, obstetric and neonatal complications. Awareness of this too often neglected pathology and orientation towards multidisciplinary management of obese patients during routine consultations.
● Appropriate education of mothers on nutrition and physical activity to reduce theprevalence of overweight.
● Good blood sugar control before and during pregnancy helps prevent macrosomia and other complications such as maternal and neonatal trauma during birth.
● Pregnancy monitoring.
● Childbirth should be planned without leaving anything to chance.It should be organized with a multidisciplinary team.
Declaration of Interests
The authors declare that they have no conflictof interest in relation to this article.
References
- Ducarme G, Rodrigues A, Aissaoui F, et al. Pregnancy in Obese Patients: What risks should we fear?. Obstetrics and Fertility Gynecology 35 (2007): 19-24.
- Djrolo F, Megnigbeto Obey A, De Souza J, et al. Influence of Maternal Weight on the Evolution of Pregnancy in Cotonou (Benin). J Gynecolobstetbiolreprod 31 (2002): 243-247.
- Hamon C, Fanello S, Catala L, et al. Consequences of Maternal Obesity on the Course of Labor and Childbirth. J Gynecolobstetbiolreprod 34 (2005): 109-114.
- Zhang J, Bricker L, Wray S. Poor Uterinecontractility in Obese Women. Bjog 114 (2007): 343-348.
- Chu Sy, Kim Sy, Bish Cl. Prepregnancy obesity prevalence in Theunited States, 2004-2005. Matern Child Health J 13 (2009): 614-620.
- O'dwyer V, O'toole F, Darcy S, et al. Maternal Obesity and Gestational Weight Gain. Journal of Obstetrics and Gynecology 33 (2013): 671-674.
- Weiss Jl, Malone Fd, Emig D. Obesity, Obstetric Complications and Cesareandelivery Rate- A Population-based Screening Study. Am J Obstetgynecol 190 (2004): 1091-1097.
- Last P. Obesity and Pregnancy. Gynecolobstetfertil 39 (2011): 100-105.
- Dempsey Jc, Ashiny Z, Qiu Cf, et al. Maternalpre-Pregnancy overweight status and Obesity as Riskfactors Forcesareandelivery. J Maternfetalneonatal Med 17 (2005): 179-185.
- Magnin G. Childbirth of the Big Child. Prat Childbirth J Lansac G Bodyeds Vilerbanne Simep Edn (1989): 149.
- Fettah Meriem Full Term Fetal Macrosomia (About 340 Cases) these Presented and Publicly Supported on 06/29/2016 Fes, Morocco (2016).
- John Andersen, Joe Watt, Jaret Olson, et al. Perinatal Brachial Plexus Palsy. Paediatrics & Child Health (2006): 93-100.
- Aisha Salim Said, Karim Premji Manji. Risk Factors and Outcomes of Fetal Macrosomia in a Tertiary Center in Tanzania: A Case-Control Study. Bmc Pregnancy and Childbirth 16 (2016): 243
- Panel P, De Meus Jb, Yanolopoulos B, et al. Childbirth of the Big Child. J.Gynecol. Obstet. Biol. Reprod 20 (1991): 729-736.
- Touzet S, Rocher L. Study of Observation of Gestational Diabetes Screening Practices from a Cohort of 701 Women 2001. Journal De Gynecologie Obstetrique Et Biologie De Reproduction 31 (2002): 248-225.
- Cedergren Mi. Maternal morbidobesity and the Risk of Adverse Pregnancy outcome. Obstetgynecol 103 (2004): 219-224.
- Ndiaye O, Sylla A, Cisse Ct, et al. Influence of Excess Maternal Weight on the Birth Weight of a Population of Term Newborns in Senegal. Journal of Pediatrics and Childcare 18 (2005): 33-37.
- Kumari As. Pregnancy outcome in Women with morbid obesity. Int J Gynaecolobstet 73 (2001): 101-107.
- Grossetti E, Beucher G, Regeasse A, et al. Obstetric Complications of Morbid Obesity. J Gynecolobstetbiol Reprod 33 (2004): 739-744.