Predicting Service Urgency in Children and Youth with Autism Spectrum Disorder: The Development of an Algorithm
Article Information
Shannon L. Stewarta, Gabrielle K.C. Kingb,*, Jocelyn N. Van Dykec, Jeffrey W. Possd
aFaculty of Education, Western University, 1137 Western Rd, N6G 1G7 London, Ontario, Canada
bFaculty of Education, Western University, 1137 Western Rd, N6G 1G7 London, Ontario, Canada
cFaculty of Education, Western University, 1137 Western Rd, N6G 1G7 London, Ontario, Canada
dFaculty of Health, University of Waterloo, 200 University Ave W., N2L 3G5 Waterloo, Ontario, Canada
*Corresponding Author: Gabrielle K.C. King, Faculty of Education, Western University, 1137 Western Rd, N6G 1G7 London, Ontario, Canada
Received: 23 November 2023; Accepted: 01 December 2023; Published: xx December 2023
Citation: Shannon L. Stewart, Gabrielle K.C. King, Jocelyn N. Van Dyke, Jeffrey W. Poss. Predicting Service Urgency in Children and Youth with Autism Spectrum Disorder: The Development of an Algorithm. Journal of Psychiatry and Psychiatric Disorders. 7 (2023): 210-222.
View / Download Pdf Share at FacebookAbstract
Background: Autism spectrum disorder (ASD) is often accompanied by various mental health-related symptoms that impact a child’s level of functioning. This variability leads to unequal service urgency needs among children and youth with ASD. However, there is no empirically-based and clinically-informed system that assesses the urgency needs of individuals with ASD seeking mental health services. The current study describes the methods used to develop an algorithm to determine mental health service urgency for children and youth with ASD.
Method: Assessments from 20,781 and 53,387 children and youth, drawn from two types of the interRAI Child and Youth Mental Health (ChYMH) instruments used in Ontario, were examined to identify service urgency among those with a probable ASD diagnosis. An interactive decisiontree tool identified rules-based groups that were subsequently assigned to a manageable number of levels using k-means clustering. The fit of the algorithm was assessed by logistic regression analyses.
Results: The algorithm used twelve items to predict service urgency among 1,598 children with a probable ASD diagnosis. The decision tree identified 18 groups that were collapsed to five levels, from lowest to highest service urgency. The highest urgency group, which includes 12.1% of children and youth with probable autism and for whom 36.1% are rated urgent, is 11.6 times more likely to be rated as urgent, compared to the lowest group.
Conclusions: By implementing the first empirically and clinically supported decision-support tool, appropriate and efficient access to community-based mental health resources can be allocated to children and youth with ASD.
Keywords
Autism Spectrum Disorder; Children and Youth; Service Urgency; Mental Health; interRAI
Autism Spectrum Disorder articles; Children and Youth articles; Service Urgency articles; Mental Health articles; interRAI articles
Autism Spectrum Disorder articles Autism Spectrum Disorder Research articles Autism Spectrum Disorder review articles Autism Spectrum Disorder PubMed articles Autism Spectrum Disorder PubMed Central articles Autism Spectrum Disorder 2023 articles Autism Spectrum Disorder 2024 articles Autism Spectrum Disorder Scopus articles Autism Spectrum Disorder impact factor journals Autism Spectrum Disorder Scopus journals Autism Spectrum Disorder PubMed journals Autism Spectrum Disorder medical journals Autism Spectrum Disorder free journals Autism Spectrum Disorder best journals Autism Spectrum Disorder top journals Autism Spectrum Disorder free medical journals Autism Spectrum Disorder famous journals Autism Spectrum Disorder Google Scholar indexed journals Children and Youth articles Children and Youth Research articles Children and Youth review articles Children and Youth PubMed articles Children and Youth PubMed Central articles Children and Youth 2023 articles Children and Youth 2024 articles Children and Youth Scopus articles Children and Youth impact factor journals Children and Youth Scopus journals Children and Youth PubMed journals Children and Youth medical journals Children and Youth free journals Children and Youth best journals Children and Youth top journals Children and Youth free medical journals Children and Youth famous journals Children and Youth Google Scholar indexed journals Service Urgency articles Service Urgency Research articles Service Urgency review articles Service Urgency PubMed articles Service Urgency PubMed Central articles Service Urgency 2023 articles Service Urgency 2024 articles Service Urgency Scopus articles Service Urgency impact factor journals Service Urgency Scopus journals Service Urgency PubMed journals Service Urgency medical journals Service Urgency free journals Service Urgency best journals Service Urgency top journals Service Urgency free medical journals Service Urgency famous journals Service Urgency Google Scholar indexed journals Mental Health articles Mental Health Research articles Mental Health review articles Mental Health PubMed articles Mental Health PubMed Central articles Mental Health 2023 articles Mental Health 2024 articles Mental Health Scopus articles Mental Health impact factor journals Mental Health Scopus journals Mental Health PubMed journals Mental Health medical journals Mental Health free journals Mental Health best journals Mental Health top journals Mental Health free medical journals Mental Health famous journals Mental Health Google Scholar indexed journals interRAI articles interRAI Research articles interRAI review articles interRAI PubMed articles interRAI PubMed Central articles interRAI 2023 articles interRAI 2024 articles interRAI Scopus articles interRAI impact factor journals interRAI Scopus journals interRAI PubMed journals interRAI medical journals interRAI free journals interRAI best journals interRAI top journals interRAI free medical journals interRAI famous journals interRAI Google Scholar indexed journals Ministry of Children, Community and Social Services articles Ministry of Children, Community and Social Services Research articles Ministry of Children, Community and Social Services review articles Ministry of Children, Community and Social Services PubMed articles Ministry of Children, Community and Social Services PubMed Central articles Ministry of Children, Community and Social Services 2023 articles Ministry of Children, Community and Social Services 2024 articles Ministry of Children, Community and Social Services Scopus articles Ministry of Children, Community and Social Services impact factor journals Ministry of Children, Community and Social Services Scopus journals Ministry of Children, Community and Social Services PubMed journals Ministry of Children, Community and Social Services medical journals Ministry of Children, Community and Social Services free journals Ministry of Children, Community and Social Services best journals Ministry of Children, Community and Social Services top journals Ministry of Children, Community and Social Services free medical journals Ministry of Children, Community and Social Services famous journals Ministry of Children, Community and Social Services Google Scholar indexed journals risk factor articles risk factor Research articles risk factor review articles risk factor PubMed articles risk factor PubMed Central articles risk factor 2023 articles risk factor 2024 articles risk factor Scopus articles risk factor impact factor journals risk factor Scopus journals risk factor PubMed journals risk factor medical journals risk factor free journals risk factor best journals risk factor top journals risk factor free medical journals risk factor famous journals risk factor Google Scholar indexed journals ASD Service Urgency for Children and Youth Algorithm articles ASD Service Urgency for Children and Youth Algorithm Research articles ASD Service Urgency for Children and Youth Algorithm review articles ASD Service Urgency for Children and Youth Algorithm PubMed articles ASD Service Urgency for Children and Youth Algorithm PubMed Central articles ASD Service Urgency for Children and Youth Algorithm 2023 articles ASD Service Urgency for Children and Youth Algorithm 2024 articles ASD Service Urgency for Children and Youth Algorithm Scopus articles ASD Service Urgency for Children and Youth Algorithm impact factor journals ASD Service Urgency for Children and Youth Algorithm Scopus journals ASD Service Urgency for Children and Youth Algorithm PubMed journals ASD Service Urgency for Children and Youth Algorithm medical journals ASD Service Urgency for Children and Youth Algorithm free journals ASD Service Urgency for Children and Youth Algorithm best journals ASD Service Urgency for Children and Youth Algorithm top journals ASD Service Urgency for Children and Youth Algorithm free medical journals ASD Service Urgency for Children and Youth Algorithm famous journals ASD Service Urgency for Children and Youth Algorithm Google Scholar indexed journals Child and Youth Mental Health articles Child and Youth Mental Health Research articles Child and Youth Mental Health review articles Child and Youth Mental Health PubMed articles Child and Youth Mental Health PubMed Central articles Child and Youth Mental Health 2023 articles Child and Youth Mental Health 2024 articles Child and Youth Mental Health Scopus articles Child and Youth Mental Health impact factor journals Child and Youth Mental Health Scopus journals Child and Youth Mental Health PubMed journals Child and Youth Mental Health medical journals Child and Youth Mental Health free journals Child and Youth Mental Health best journals Child and Youth Mental Health top journals Child and Youth Mental Health free medical journals Child and Youth Mental Health famous journals Child and Youth Mental Health Google Scholar indexed journals child protective services articles child protective services Research articles child protective services review articles child protective services PubMed articles child protective services PubMed Central articles child protective services 2023 articles child protective services 2024 articles child protective services Scopus articles child protective services impact factor journals child protective services Scopus journals child protective services PubMed journals child protective services medical journals child protective services free journals child protective services best journals child protective services top journals child protective services free medical journals child protective services famous journals child protective services Google Scholar indexed journals
Article Details
1. Introduction
There are many challenges facing Ontario, Canada’s children’s mental health system. Due to inefficient practices, such as the lack of a standardized system and inconsistent practices across the province, many children and youth in need have inadequate access to mental health services [1]. These inefficiencies lead to further barriers to accessing mental health care, including long wait times. A recent report on access to community child and youth mental health services in Ontario demonstrates that wait times for services are at an all-time high [2]. To address the service system shortfalls and subsequently improve access to children’s mental health care, researchers have called for a standardized system to measure and prioritize children’s mental health care needs [1]. Consequently, many mental health agencies across Ontario are now using the interRAI Child and Youth Suite of instruments to support service system integration as well as early identification, assessment, care planning, and quality assurance [3]. The current study suggests a method of mental health service prioritization for a population that has demonstrated consistently high mental health service needs, autism spectrum disorder [4,5,6]. For children and youth with ASD, the lack of a standardized system for determining mental health service need is particularly problematic. ASD is characterized by differences in social communication and interaction as well as restricted, repetitive patterns of behaviour, interests, or activities [7]. These children have significant mental health care needs, such as being 75.4% more likely than children without ASD to need treatment or counselling for emotional, developmental, or behaviour concerns [4]. Children with ASD are more likely to visit the emergency department compared to children without ASD [5, 6]. However, children with ASD are less likely than children without ASD to be admitted to the hospital, indicating that these emergency department visits may have been prevented or avoided perhaps if families had earlier access to resources [5]. Despite their potentially high need for support, families of children with ASD have more difficulties accessing health care and family support services than families with other non-ASD health care needs [8, 9]. These demands for services indicate a need to address current inefficiencies in the mental health care system. However, mental health service use is not the same for each child and youth with ASD. Some features and symptoms place children at a higher risk of requiring more urgent care than others, indicating a need-based, individualized approach to care to ensure those with the highest service urgency are able to access the appropriate, sufficient, and timely mental health care that is required.
1.1 Individual Risk Factors
Although a set of core features characterizes ASD, there is significant heterogeneity of phenotypic presentations that exist in terms of symptoms and range of abilities [10]. ASD is often accompanied by a co-occurring disorder, condition, or difficulty [11]. Common conditions and difficulties can include disruptive behaviours and irritability [12], motor problems, cognitive disabilities, temper tantrums, and self-injurious behaviours [10, 11]. Children with ASD are at increased risk of co-occurring disorders such as attention deficit hyperactivity disorder (ADHD), oppositional defiant disorder (ODD), anxiety disorders, and mood disorders [13, 14]. Due to the expected range of abilities and differences among children and youth diagnosed with ASD that impacts their likelihood to seek mental health services, service utilization is not evenly distributed [10, 15]. Within the broad spectrum of ASD, some risk factors increase the chances that children and youth may require services. Anxiety disorders, commonly co-morbid with ASD, have been associated with increases in mental health service use [16, 17]. Specifically, OCD, which is characterized by unwanted, recurrent repetitive behaviours, known as compulsions, and/or thoughts, known as obsessions, is estimated to impact approximately 17-37% of people with ASD [17; 18]. Co-occurring OCD and ASD are associated with an increased risk of hospitalization [17, 18]. Additionally, children with these co-occurring disorders have been found to engage in mental health services significantly longer than those who do not have co-occurring OCD and ASD [17,18]. Mood disorders and disturbances, including depressive and bipolar disorders, which also commonly co-occur in ASD are associated with greater service use [19, 20]. Compared to children and youth with ASD without a co-occurring psychiatric disorder, those with co-occurring disorders have been associated with an increased risk for hospitalization [17, 21]. Specifically, depression is associated with some of the most precarious and challenging behaviours associated with ASD, such as aggression and self-injury [22]. Previous research has found that children and youth with ASD who have externalizing problems, such as aggressive behaviours, were at an increased risk of presenting to the emergency department and hospitalization [17, 21]. However, there may be incongruence between the need and ability to access appropriate and sufficient care. For example, in a qualitative study, parents reported that disruptive and aggressive behaviours had negative impacts on their ability to access formal services and supports for their child with ASD [23]. Furthermore, it has been found that disruptive behaviours increase the chances of unmet service needs by over 400% [24]. Self-injurious behaviours among children with ASD is a serious and challenging problem impacting approximately 30% or more of those diagnosed [25]. Children with ASD who engage in self-injurious behaviours, such as hand or arm biting, headbanging, and self-choking, are also at an increased risk of presenting to emergency services and, under certain circumstances, increased hospitalization [6, 17, 21]. It has been found that children with ASD who received early intervention had a reduced prevalence of self-injurious behaviours [25]. The impact that early intervention can have on such challenging and precarious behaviours provides support for having efficient and streamlined access to mental health services. Finally, exposure to trauma, particularly child maltreatment such as emotional abuse, physical abuse, sexual abuse, and neglect, are experienced significantly more often by children and youth with ASD, compared to a non-clinical control group [26]. Possessing symptoms characteristic of ASD, such as having language delays, differences in social communication and interactions, as well as other co-morbidities may increase the likelihood that these children will not only be victimized by others, but also have severe emotional reactions to the trauma [27,28,29,30,31]. Child maltreatment in ASD populations is associated with a range of concerns, compared to children with ASD who have not been maltreated, including a higher likelihood of aggression, tantrums, hyperactivity [26], intrusive thoughts, distressing memories, loss of interest, irritability, and lethargy [32]. Furthermore, children with ASD who have been maltreated are more likely to use mental health services than those who had not been maltreated [33]. Such variability and breadth of functioning and service use of individuals with ASD supports a standardized assessment-to-intervention system that properly triages and prioritizes resources to the children and youth who have the highest service urgency need while also addressing their needs, strengths and preferences.
1.2 Familial Risk Factors
Many familial risk factors affect service use among families with children with ASD. The odds of using ASD-related services are greater when caregivers have high stress [34]. Furthermore, families with higher incomes [34, 35] and families with a higher socioeconomic status [34, 36] have greater access to care. In contrast, service usage is lower for families with low levels of education, those from ethnic or racial minority groups [37], and those from nonmetropolitan areas, indicating potential disparities regarding access to services among these families [34]. Specifically related to mental health service usage, those from ethnic or racial minority groups are less likely to have access to a psychologist or a case manager [34]. Additionally, children with ASD from single-parent homes are more likely to require psychiatric hospitalization, than two-parent families [17]. Compared to other ASD-related services, hospitalization may be uniquely indicative of a failure to provide appropriate community-based care for these families [17].
1.3 Current Study
The Ontario Ministry of Children, Community and Social Services (MCCSS) has attempted to standardize the process for determining which children and youth with ASD can access services and supports by proposing ten risk factors [38]. These risk factors provide criteria for determining service urgency by focusing on the child or youth’s risk of aggression towards others and property, as well as risk of harm to self. The ten key risk factors proposed by the MCCSS are suicidal ideation or behaviour, violent thinking, fire starting, harm to animals, risk of exploitation, self-injurious behaviour, aggression, inappropriate sexual behaviour, flight risk, and property destruction [38]. Based on the presence of these risk factors, varying degrees of services and support, including urgent response services, are provided to the child or youth to prevent further escalation of risk [38]. However, some individual and familial factors that have been linked to increased use of services were not included within the list of identified risk factors, highlighting areas of consideration which might better predict service urgency. The current study expands upon the MCCSS initiative by developing an algorithm that will identify risk factors associated with service urgency for children and youth with ASD. Currently, there is no evidence-based systematic approach of prioritizing services to children and youth with ASD who indicate the highest need. To address this gap, the ASD Service Urgency for Children and Youth Algorithm (ASUCH) was developed. The current study aims to describe the clinical decision-making and empirical methods used to validate and develop an algorithm for service urgency for children and youth with ASD.
2. Materials and Methods
2.1 Participants
Assessments from 20,781 and 53,387 children and youth, drawn from two types of the interRAI Child and Youth Mental Health (ChYMH) instruments used in Ontario across 59 community-based and residential mental health agencies in Ontario, were examined to identify trends of service urgency among those with a probable ASD diagnosis. Research ethics was obtained from the University of Western Ontario (REB#106415).
2.2 Materials & Design
interRAI ChYMH and ChYMH-Developmental Disabilities. To inform mental health care plans and identify children and youth’s mental health risk factors and needs the interRAI Child and Youth Mental Health Assessment [39, 40] and the interRAI Child and Youth Mental Health and Developmental Disability Assessments [41], comprehensive assessment tools were utilized [42, 43]. The ChYMH is comprised of over 400 items that are organized into 22 sub-sections and contains a variety of algorithms and scales aimed to empirically assess areas of strengths, risks, needs, and overall functioning of the child and youth. The data is collected by trained multidisciplinary assessors as a standard clinical practice. Using multiple sources, such as information from the child or youth, their teachers, clinicians, caregivers, and any accessible education and medical records, trained administrators create a comprehensive assessment of the child and family’s needs, preferences and strengths. The interRAI ChYMH-Developmental Disabilities (ChYMH-DD) assessment was also used [41] to provide a comprehensive assessment for children and youth with developmental and intellectual disabilities with a core set of similar items for comparison and contrast. The ChYMH-DD has and some additional clinically relevant items for this vulnerable sub-population were added [42, 43].
interRAI ChYMH Screener. The interRAI ChYMH Screener [40] is a brief, 99 item, initial screening assessment used for the purpose of assisting in decision-making related to triaging and the prioritization of services [42, 43, 44]. The ChYMH-S has been adapted from the ChYMH and uses semi-structured interviews to provide a snapshot of the various aspects of the child’s functioning and aids in determining if a more comprehensive assessment is needed. The ChYMH, ChYMH-DD, and ChYMH-S are part of the Child and Youth suite of interRAI assessment tools, in which the scales and algorithms demonstrate robust psychometric properties [40, 45, 46, 47, 48, 49]. More information regarding the interRAI assessment tools can be found on the interRAI website (www.interrai.org). Informed consent was gained by parents of children through consent to provide treatments in participating mental health facilities.
RiSsK Scale. The Risk of Suicide and Self-Harm in Kids (RiSsK) scale is a psychometrically sound decision-support tool that can be calculated from the ChYMH-S assessment. Its seven-point scale represents increasing likelihood of suicide and self-harm [49].
2.3 Procedures
To achieve the goal of modeling service urgency among assessed mental health children and youth with ASD, a cohort of assessed individuals with ASD along with their rating of service urgency was required. None of the assessment instruments described above had both of these measures. As shown in Figure 1, the ChYMH and ChYMH-DD have an ASD diagnosis represented in the instrument, but not service urgency, and the ChYMH-S has service urgency, but not the ASD diagnosis. The key to the analytic plan was to identify cases in the ChYMH-S that were likely to have ASD, based on a number of characteristic items. There are four binary-coded ASD characteristic items common to both the ChYMH/ChYMH-DD and ChYMH-S: i) narrowly restricted range of interest, ii) excessive preoccupation with activity/routine, iii) lack of social and emotional conventions when socializing, and iv) difficulty adapting to even minor change. The first step of the analysis was to investigate the performance of these items in selecting observations in ChYMH and ChYMH-DD data where the ASD diagnosis was known to be present or absent. Univariate associations of each item with ASD, and trials of sums of the items were explored, involving sensitivity, specificity, and positive and negative predictive values. The chosen rules for selecting ASD observations were checked with regards to representativeness, specifically any significant age and sex differences those rules would select compared with all ASD observations. As the second step, these rules developed in the ChYMH and ChYMH-DD data for selecting observations that were likely to have ASD were applied to the ChYMH-S data, where the service urgency item was collected. These selected observations were then used to model service urgency. The dependent variable was “initiation of mental health services required within 7 days”. The response to this item is based on the assessor’s best judgement of urgency, given what they know about the case in the context of the information gathered to complete the screening assessment, and also additional information gleaned from all available sources at that point of contact with the client and their supports.
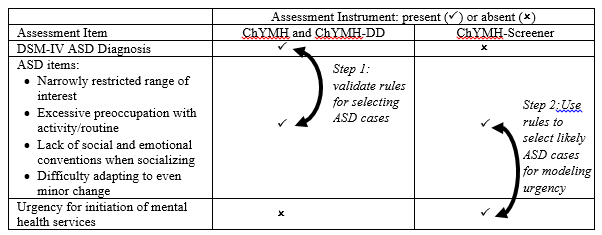
Figure 1: Assessment Instruments Showing Key Variables
2.4 Analysis
An interactive decision-tree tool available in the SAS Enterprise Miner software was used. Decision trees iteratively subset the observations into smaller branches using the available items as split points, achieving final groupings that represent distinct levels of likelihood of the dependent variable [50]. In contrast to multi-variable regression where understanding interactions among predictive items is challenging when there are large numbers of predictors, tree models naturally handle and represent interactions. In this application, the modeler manually selects the splitting variables at each possible point, using a combination of statistical power of that branch and the context of that clinical item in the tree. Branching continues until either too few observations remain in a branch, or no remaining splitting variable produces a significant difference in the dependent variable. Many possible trees can be composed, in an iterative manner. The first split of a tree is particularly influential. The dataset here was a modest size for this type of modeling, and the decision was made to not set aside a randomly selected validation sub-sample since it would restrict the tree to one that was simpler and less powerful. Instead, the interactive software supports an approach whereby the data are split randomly (here 70%/30%) and the modeler sees the effect of a suggested branch in the 30% sub-sample and can reject splits where there was not agreement between the two. In this way, we sought to avoid over-fitting, where the model fits the derivation data well due to random associations in those data but fails to achieve this in new data. A design goal of the resulting assessment urgency algorithm was for it to have a range of values from 1 to 5. The many final branches of the decision tree were subsequently grouped, informed by a k-means cluster algorithm, into five groups. Logistic regression was used to assess the fit of the algorithm. Analyses were performed using SAS 9.4 and SAS Enterprise Miner 14.
3. Results
In the first step, the ChYMH/ChYMH-DD data comprised 20,781 assessments, of which 2,594 (12.5%) had a diagnosis of ASD. Conventional methods showed that one of the four ASD indicator items, difficulty adapting to even minor change, showed lower association with an ASD diagnosis than the other three. Two formulations of the four indicator items were tried, one requiring all four binary items, and the other dropping the weak item. Table 1 summarizes the results of the two options using the full assessments (ChYMH and ChYMH-DD) and ASD rule samples. The 3-item rule selected almost twice as many cases (1,580 versus 860). The positive predictive value is the most important metric, since we wish to have the highest confidence possible that those cases selected with the rule do in fact have an ASD diagnosis, and here the values were quite close: 54.4% for 3-items, 55.6% for 4-items. Checking the ability of the two rules to select cases that were representative of the age and sex distribution of ASD cases, the 3-item rule performed slightly better (results in Supplemental Table). On the strength of selecting more cases with no significant loss of confidence that most of these cases had ASD, and being more representative, the 3-item rule was chosen for the second step. Applying the 3-item rule to eligible observations (n=53,387) of the ChYMH-S (first observations of unique individuals within service providers), there were 1,598 (3.0%) that were selected with probable ASD, of which 23.4% were female. This final sample included 1,598 (23.4% female) children and youth with probable ASD,. Participants were an average of 10.3 years old (SD = 3.4, range: 4-18) with most participants (n= 600, 37.8%) between the ages of 8 and 11. See Table 2 for ChYMH-S decision tree derivation sample characteristics and responses to items used to assess service urgency. Of these 1,598 children and youth with probable ASD, 213 were rated as requiring services to be initiated within 7 days (13.3%). These data were modeled with the interactive decision tree tool. Multiple trees were explored, notably including choosing a first split of sex, and of age group, and a powerful item, outburst of anger. The RiSsK scale of self-harm showed good characteristics when used as a three-way initial split, but the resulting tree included only characteristics of the child/youth. One measure of the family, belief (by child/youth, family, staff, or others) that parents are not sufficiently engaged in the child’s/youth’s life, showed a strong association with service urgency, but it was too rare in this sample to be used anywhere but as the first split, which was done, followed by a 3-way split of the RiSsK scale. The final tree (Figure 2) has 18 terminal nodes and uses 12 different items. Two items (irritability, obsessive thoughts) are each used twice in the tree logic. Gathering the 18 terminal nodes into five groups produced the distribution shown in Table 3, with proportions requiring services within 7 days shown along with odds ratios. For the highest urgency group, representing 12.1% of the ChYMH-S sample, 36.1% required services within 7 days, resulting in an odds ratio of 17.9 compared to the lowest urgency group.
Table 1: ASD Indicator Item Analysis for the Full Assessments (ChYMH and ChYMH-DD)
(Used to test two options of rules for subsequently selecting those likely to have ASD where no diagnosis is recorded in the ChYMH-S data)
|
All 4 items a true |
Best 3 items b true |
|
|
Observations selected (n) |
860 |
1,580 |
|
Sensitivity (%) |
18.4 |
33.1 |
|
Specificity (%) |
97.9 |
96.0 |
|
Positive Predictive Value (%) |
55.6 |
54.4 |
|
Negative Predictive Value (%) |
89.4 |
91.0 |
Note: n = 20,781 assessments, of which 2,594 (12.5%) had a diagnosis of ASD.
aThe four ASD indicator items include: a) narrowly restricted range of interest, b) excessive preoccupation with activity/routine, c) lack of social and emotional conventions when socializing, and d) difficulty adapting to even minor change.
bThe best 3 ASD indicator items include: a) narrowly restricted range of interest, b) excessive preoccupation with activity/routine, and c) lack of social and emotional conventions when socializing.
Table 2: ChYMH Screener Decision Tree Derivation Sample Characteristics
|
n (%) |
|
|
All |
1,598 |
|
Sex, Female |
374 (23.4%) |
|
Age M (SD) |
10.3 (3.4) |
|
under 7 |
381 (23.8%) |
|
8 to 11 |
600 (37.6%) |
|
12 to 14 |
393 (24.6%) |
|
15 to 18 |
224 (14.0%) |
|
RiSsK Scorea: 0,1 or 2 |
1,244 (77.9%) |
|
3 |
223 (13.9%) |
|
4 or 5 |
131 (8.1%) |
|
Self-injury attempt in the last year |
221 (13.8%) |
|
Outburst of anger: no, or not daily |
1,111 (69.5%) |
|
daily, 1 or 2 episodes |
256 (16.5%) |
|
daily, 3 or more episodes |
231 (14.5%) |
|
Socially inappropriate/disruptive behaviour in last 3 days |
192 (12.0%) |
|
Irritability |
490 (30.7%) |
|
Made negative statements |
1,014 (63.5%) |
|
Sad, pained, worried facial expression |
233 (14.6%) |
|
Labile affect |
436 (27.3%) |
|
Obsessive thoughts |
777 (48.6%) |
|
Stealing - never |
1,331 (83.3%) |
|
Yes, not in last 3 days |
241 (15.1%) |
|
Yes, in last 3 days |
26 (1.6%) |
|
Victim emotional abuse |
283 (17.7%) |
|
Parents not sufficiently engaged |
37 (2.3%) |
a RiSsK: Risk of Suicide and Self-Harm in Kids scale
Supplemental Table: Comparing Demographics of 3-Item Rule vs 4-Item rule for Identifying ASD in the ChYMH/ChYMH-DD Cases
|
All with ASD diagnosis |
4-item rule |
3-Item rule (selected) |
|
|
n |
2,594 |
860 |
1,580 |
|
Age M (SD) |
12.1 (3.41) |
11.2 (3.23) |
11.5 (3.31) |
|
Under 7 |
11% |
13% |
13% |
|
8 to 11 |
32% |
40% |
37% |
|
12 to 14 |
30% |
28% |
29% |
|
15 and older |
28% |
18% |
21% |
|
Male |
75% |
78% |
78% |
Table 3: ASD Service Urgency Algorithm Results
|
Algorithm Value |
n |
Percent of sample (%) |
Percent of sample requiring services within 7 days (%) |
Odds ratios |
|
(95% CI) |
||||
|
1 |
426 |
26.7 |
3.1 |
ref |
|
2 |
262 |
16.4 |
6.1 |
2.07 (0.98 - 4.37) |
|
3 |
358 |
22.4 |
10.6 |
3.77 (1.98 - 7.20) |
|
4 |
358 |
22.4 |
20.9 |
8.42 (4.58 - 15.46) |
|
5 |
194 |
12.1 |
36.1 |
17.93 (9.60 - 33.50) |
|
Total |
1,598 |
100 |
13.3 |
c-statistic: 0.746 |
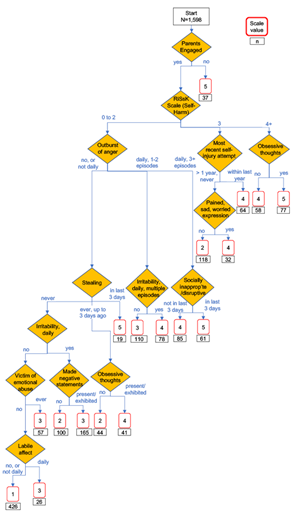
Figure 2: ASD Service Urgency Algorithm Tree Diagram, with Derivation n’s
4. Discussion
Service urgency in ASD was predicted by several different contributors, including familial factors and child-level symptoms and behaviours. Parental disengagement is a familial factor that received the highest level of urgency in the algorithm. There are many potential reasons why parents may be disengaged, and subsequently, their children may require an urgent need for services to circumvent or prevent out-of-home placements. Compared to children who are typically developing or those with intellectual disabilities, children with ASD have a higher prevalence and risk of being involved with the foster care system [51]. Additionally, children with ASD, as well as those with other disabilities, are more likely to be involved in child protective services (CPS) than children without disabilities [52]. Previous studies point to a lack of available resources, including non-urgent treatments and supports, as a reason why parents of children with ASD may struggle to manage their child’s difficult behaviours [51]. This may add to parental disengagement, as families have no other option but to turn to urgent services to prevent out-of-home placements. There are multiple psychological and financial stressors impacting parents of children with ASD which may also contribute to parental disengagement. Compared to caregivers of neurotypical children, caregivers of children with ASD are more likely to be at risk for mental health issues, including poor psychological well-being [53] and parenting stress [54]. Furthermore, children with ASD who come from families with parental mental health issues were overrepresented in CPS [53]. There are many stressors placed on families with children who have ASD, such as a higher financial burden and more lost wages related to increased demands on the caregiver [55]. For families without supports, these stressors may be overwhelming and may contribute to poor parental mental health and subsequent disengagement. Contrarily, families with informal support systems, such as friends, family, or others in their circle of care, have improved mental health, such as lower levels of depression and anxiety [56, 57] and reduced stress levels [58]. This indicates that those who lack this informal support system may have higher stress and lower well-being, which may impact the caregiver’s ability to sufficiently engage in their child’s life. Therefore, poor parental mental health and the potential for subsequent parental disengagement are important factors to consider when examining the child’s risk for needing urgent supports. Access to financial resources may also contribute to disengagement between the parent and child. Previous literature suggests that access to services is greater in families with higher income and education status [34, 35, 36]. Low-income families, in addition to having more difficulties accessing services for early intervention, may have to focus their cognitive resources on a myriad of other stressors, which may result in a reduced ability to engage with their child’s potentially complex needs. Furthermore, children with ASD from single parent homes are more likely to require psychiatric hospitalization, perhaps due to a lack of appropriate resources to access early intervention and expensive home-based services [17]. Hospitalization may serve as a respite for these families [17]. Therefore, families with many financial and other stressors may be unable to sufficiently engage with their children or may lack the appropriate resources to engage in early intervention services, resulting in urgent unmet needs for these children. Being a victim of emotional abuse was another factor that contributed to service urgency in children with ASD. Though previous studies have demonstrated that maltreatment in children with ASD is associated with a range of outcomes including internalizing and externalizing problems [32], recent research has extended this work by examining if certain subtypes of abuse are more strongly related to outcomes in children with ASD [26]. Interestingly, it was discovered that emotional abuse, but not physical abuse, is associated with behavioural concerns in children with ASD [33]. This finding aligns with other recent research indicating that emotional abuse is a pervasive and highly impactful form of child maltreatment [59, 60]. When compared to other forms of maltreatment, emotional abuse is associated with the largest increase in revictimization, the highest rates of posttraumatic stress disorder (PTSD) symptoms [61], and is the strongest predictor of emotion dysregulation [62]. It is one of the most common forms of child maltreatment, with 27.7% of children from a clinical sample having experienced emotional abuse [31]. Furthermore, emotional abuse is a good indicator that other forms of abuse may be present, with 85.4% of emotionally abused children meeting the criteria for other forms of maltreatment, such as physical abuse, neglect, witnessing domestic violence, or sexual abuse [31, 59, 63]. Therefore, this item in the algorithm may be a good way to identify children at risk for high service urgency need, as well as capture many children who have been maltreated, including those who may be exposed to other forms of abuse. Several of the predictor variables were related to child-level symptoms and behaviours. The risk of suicide and self-harm and the child’s most recent self-injury attempt were found to be related to service urgency in children with ASD. This result is aligned with previous literature, which has identified self-harm and suicidal ideation as an influential factor in children and youth’s level of resource intensity across clinical populations [42, 48], as well as increased service use in ASD populations [6, 17, 21, 25]. The increased use of intensive and urgent services by children and youth who self-harm and are at high-risk for suicide is due to the naturally imminent risk of partaking in such life-threatening behaviours [64] Suicidal and non-suicidal self-injury have been major risk factors for future self-harm and suicidality [49, 65]. In addition to self-harm and suicide-related behaviours, previous research has shown that other internalizing-related symptoms and behaviours with co-occurring ASD, such as depression, anxiety, and other mood disturbances, are associated with increased service use [16, 17, 18, 21]. These relationships were accounted for within the current algorithm, with the items labile affect, sad, pained, or worried expression, irritability, the use of negative statements, and obsessive thoughts. Behaviours and symptoms that are related to the child’s safety (suicide and self-harm) and emotional distress (mood and anxiety) have been identified by caregivers of children and youth with ASD as top reason to visit the emergency department for mental health-related issues [66]. Emergency services provide opportune support that will ensure the provision of professional and prompt care and safety of the child with hospital procedures and policies in place [67]. With the absence of clear pathways of support and respite care, overwhelmed and stressed parents are turning to hospital services for support, which may be driving the increased hospitalizations of children with ASD [68]. The last child-level symptom group identified as a contributing factor to ASD service urgency is externalizing symptoms such as aggressive and disruptive behaviours. Specifically, the algorithm found that behaviours such as stealing, outbursts of anger, and socially inappropriate and disruptive behaviours predicted high service urgency needs. These findings are aligned with previous research, which has found that externalizing symptoms leads to increased service use, including hospitalizations and use of emergency services in both ASD and non-ASD populations [17, 21, 48, 69]. One study found that externalizing behaviours in children with ASD were the leading cause of visits to the emergency department for mental health-related reasons [6]. Furthermore, externalizing behaviours in ASD have been found to be a leading cause of parental stress [70]. Therefore, while ensuring immediate care and safety of children, accessing support through services [67] may also help alleviate parental stress through professional care [68].
4.1 Implications
Based on the current study's findings, the ASUCH is a psychometrically sound decision-support tool that may inform the service urgency needs of children and youth with ASD seeking facility-or-community-based services. It has been found to be a strong identifier of children requiring service urgency, with those scoring five having greater odds of requiring services (odds ratio = 16.93) within seven days compared to those scoring one. This will support staff to provide systematic evaluations of the child’s service urgency needs.
The ASUCH results can be accessed by service providers who have administered the interRAI ChYMH-S, automatically through embedded algorithm software. Similar to other algorithms previously published, such as the Risk of Suicide and Self-harm (RiSsK), the Risk of Injury to Others (RIO), the interRAI ChYMH Caregiver Distress Algorithm [71] and Resource Intensity for Children and Youth (RIChY), scores can be accessed immediately and interpreted alongside other sources of information gathered for the interRAI assessment and in conjunction with clinical judgment [48, 49, 72]. The responsibility of prioritization and resource allocation remains with the clinical team to make informed decisions about the child’s relative service urgency needs. The child and family should also be included in care planning decisions to ensure consideration of the child’s unique needs, strengths, and preferences. The results obtained from the ASUCH can be used to inform the service provider’s decisions regarding the prioritization of resources for children and youth with ASD. Furthermore, together with other sources of information, it can inform what resources are allocated to the child. The care plan is developed based on whether the child obtains a lower or higher service urgency score. A lower ranged service urgency score may require further clinical interpretation to ensure that the score is appropriate based on other sources of information. If an individual obtains a higher ranged service urgency score that is aligned with other sources of information, the clinical team should also ensure that this score is appropriate based on other sources of information and consider prioritizing resources to address the child’s urgency needs. In addition to the benefits of individualized care planning, the ASUCH also enables the opportunity for an integrated health information system using standardized data (see www.interai.org). For example, ASD service urgency levels at intake can help examine differences in how services are used by degree of needs across various regions. As a result, patterns can be identified at multiple levels (i.e., regional, organizational, national, international). Furthermore, it can be used to evaluate the effectiveness of treatment through pre-post measurements and justify expenditures. This quantifiable information can be used to inform agencies and their stakeholders of progress. Comparisons can therefore be made across different interventions and across different agencies with respect to outcome measurement.
This study has strengths, such as having a large sample size that is specific to ASD. However, it is not without its limitations. First, this study included a clinical sample of children and youth accessing inpatient and outpatient mental health services. Therefore, generalizability to other populations is limited. Secondly, the current sample uses likely ASD cases rather than confirmed ASD cases. Confirmed ASD cases from the ChYMH and ChYMH-DD were used to validate the criteria for selecting likely ASD cases on the ChYMH-S. These criteria included three items that provided the highest confidence that those who endorsed these items have ASD. The resulting criteria was then applied to the ChYMH-S to select likely ASD cases to model service urgency needs in the current study. Third, this study is modelling service urgency and not service complexity [see 73]. There are recognized challenges using service urgency to model need, for example an urgent need for services does not mean the services are necessarily complex or expensive. However, it is assumed in the current study that service urgency will pick up cases with complex service needs. Finally, due to the cross-sectional nature of the dataset, causal conclusions cannot be made. In the future, longitudinal data should be conducted to examine the service urgency needs of children with ASD as they develop. Future research should also examine whether this study's findings are consistent with non-clinical samples as well as samples with confirmed ASD diagnoses to strengthen applicability across broader populations.
5. Conclusion
The ASUCH is a decision-support tool that service providers can use to identify the service urgency needs of treatment seeking children and youth with ASD. Furthermore, this algorithm can be used to support resource allocation and prioritize needs informed by systematic evaluation. The ASUCH has applications at both the individual level to support resource allocation as well as at the systemic level to inform expenditures on a broader level and support the development of new policies.
Acknowledgements
The authors would like to thank the children, youth, and their families for their participation. The authors would also like to thank the trained assessors within the field for their contributions to the research process.
Funding:
The authors did not receive support from any organization for the submitted work.
Declaration of Interest: None
Competing Interests: The authors have no financial or proprietary interests in any material discussed in this article.
References
- Duncan L, Boyle, MH, Abelson J, et al. Measuring children’s mental health in Ontario: policy issues and prospects for change. Journal of the Canadian Academy of Child and Adolescent Psychiatry, 27 (2018): 88.
- Children’s Mental Health Ontario. Kids can’t wait: 2020 report on wait lists and wait times for child and youth mental health care in Ontario. 2020.
- Stewart SL, Toohey A. Screening and assessment of mental health problems in students: Using an integrated Assessment-to-Intervention approach to enhance integrated care. In Mental Health Assessment, Prevention, and Intervention: Promoting Child and Youth Well-Being (2022): (57-84). Cham: Springer International Publishing.
- Gurney JG, McPheeters ML, Davis, MM. Parental report of health conditions and health care use among children with and without autism: National Survey of Children's Health. Archives of Pediatrics & Adolescent Medicine, 160 (2006): 825-830.
- Deavenport-Saman A, Lu Y, Smith K, et al. Do Children with Autism Overutilize the Emergency Department? Examining Visit Urgency and Subsequent Hospital Admissions. Maternal and Child Health Journal, 20 (2016): 306-314.
- Kalb LG, Stuart EA, Freedman B, et al. Psychiatric-related emergency department visits among children with an autism spectrum disorder. Pediatric Emergency Care, 28 (2012): 1269-1276.
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders fifth edition: DSM-5. Washington, DC: American Psychiatric Association (2013).
- Kogan MD, Strickland BB, Blumberg SJ, et al. A national profile of the health care experiences and family impact of autism spectrum disorder among children in the United States, 2005-2006. Pediatrics, 122 (2008): e1149-e1158.
- Thomas KC, Parish SL, Rose RA, & Kilany, M. Access to care for children with autism in the context of state Medicaid reimbursement. Maternal and Child Health Journal, 16 (2012): 1636-1644.
- Lord C, Brugha, TS, Charman T, et al. Autism spectrum disorder. Nature Reviews Disease Primers, 6 (2020): 1-23.
- Soke GN, Maenner MJ, Christensen D, et al. Prevalence of Co-occurring Medical and Behavioral Conditions/Symptoms Among 4- and 8-Year-Old Children with Autism Spectrum Disorder in Selected Areas of the United States in 2010. Journal of Autism and Developmental Disorders, 48 (2018): 2663-2676.
- Chandler S, Howlin P, Simonoff E, et al. Emotional and behavioural problems in young children with autism spectrum disorder. Developmental Medicine and Child Neurology, 58 (2016): 202-208.
- Levy SE, Giarelli E, Lee LC, et al. Autism spectrum disorder and co-occurring developmental, psychiatric, and medical conditions among children in multiple populations of the United States. Journal of Developmental and Behavioral Pediatrics: JDBP, 31 (2010): 267-275.
- Rosen TE, Mazefsky CA, Vasa RA, et al. Co-occurring psychiatric conditions in autism spectrum disorder. International Review of Psychiatry, 30 (2018): 40-61.
- Havdahl KA, Hus Bal V, Huerta M, et al. Multidimensional influences on autism symptom measures: Implications for use in etiological research. Journal of the American Academy of Child and Adolescent Psychiatry, 55 (2016): 1054-1063.
- Kirsch AC, Huebner A, Mehta SQ, et al. Association of Comorbid Mood and Anxiety Disorders With Autism Spectrum Disorder. JAMA Pediatrics, 174 (2020): 63-70.
- Mandell DS. Psychiatric hospitalization among children with autism spectrum disorders. Journal of Autism and Developmental Disorders, 38 (2008): 1059-1065.
- Martin AF, Jassi A, Cullen AE, et al. Co-occurring obsessive-compulsive disorder and autism spectrum disorder in young people: prevalence, clinical characteristics and outcomes. European Child & Adolescent Psychiatry, 29 (2020), 1603-1611.
- Carlson GA. Differential diagnosis of bipolar disorder in children and adolescents. World Psychiatry, 11 (2012): 146-152.
- Gotham K, Pezzimenti F, Eydt-Beebe M. (2020). Co-occurring mood problems in autism spectrum disorder. The Oxford Handbook of Autism and Co-Occurring Psychiatric Conditions (p. 28-51). Oxford University Press.
- Lunsky, Y., Paquette-Smith, M., Weiss, J. A., & Lee, J. (2015). Predictors of emergency service use in adolescents and adults with autism spectrum disorder living with family. Emergency Medicine Journal: EMJ, 32 (2015): 787-792.
- Ghaziuddin M, Ghaziuddin N, Greden J. Depression in persons with autism: implications for research and clinical care. Journal of Autism and Developmental Disorders, 32 (2002): 299-306
- Hodgetts S, Nicholas D, Zwaigenbaum L. Home sweet home? Families’ experiences with aggression in children with autism spectrum disorders. Focus on Autism and Other Developmental Disabilities, 28 (2013): 166-174.
- Hodgetts S, Zwaigenbaum L, Nicholas, D. Profile and predictors of service needs for families of children with autism spectrum disorders. Autism: The International Journal of Research and Practice, 19 (2015): 673-683.
- Rattaz C, Michelon C, Baghdadli A. Symptom severity as a risk factor for self-injurious behaviours in adolescents with autism spectrum disorders. Journal of Intellectual Disability Research: JIDR, 59 (2015): 730-740.
- McDonnell CG, Boan AD, Bradley CC, et al. Child maltreatment in autism spectrum disorder and intellectual disability: results from a population-based sample. Journal of Child Psychology and Psychiatry, and Allied Disciplines, 60 (2019): 576-584.
- Hoover DW. The effects of psychological trauma on children with autism spectrum disorders: A research review. Review Journal of Autism and Developmental Disorders, 2 (2015): 287-299.
- Lapshina N, & Stewart SL. Traumatic life events, polyvictimization, and externalizing symptoms in children with IDD and mental health problems. Research in Developmental Disabilities, 116 (2021):
- Stewart SL, Semovski V, & Lapshina N. Adolescent inpatient mental health admissions: An exploration of interpersonal polyvictimization, family dysfunction, self-harm and suicidal behaviours. Child Psychiatry & Human Development, 1-12 (2022)
- Stewart SL, Lapshina N, & Semovski V. Interpersonal polyvictimization: Addressing the care planning needs of traumatized children and youth. Child Abuse & Neglect, 114 (2021).
- Stewart SL, Toohey A, Lapshina N. Childhood maltreatment and risk of harm to self and others: The role of sex and polyvictimization. International Journal of Child and Adolescent Resilience (IJCAR), 7 (2020): 108-122.
- Brenner J, Pan Z, Mazefsky C, et al. Behavioral symptoms of reported abuse in children and adolescents with autism spectrum disorder in inpatient settings. Journal of Autism and Developmental Disorders, 48 (2018), 3727-3735.
- McDonnell CG, Andrzejewski T, Dike J. Intergenerational trauma: Parental PTSD and parent-reported child abuse subtypes differentially relate to admission characteristics in the autism inpatient collection. Autism Research: Official Journal of the International Society for Autism Research, 15 (2022): 665-676.
- Thomas KC, Ellis AR, McLaurin C, et al. Access to care for autism-related services. Journal of Autism and Developmental Disorders, 37 (2007): 1902-1912.
- Irvin DW, McBee M, Boyd BA. et al. (2012). Child and family factors associated with the use of services for preschoolers with autism spectrum disorder. Research in Autism Spectrum Disorders, 6 (2012): 565-572.
- Patten E, Baranek GT, Watson LR, et al. Child and family characteristics influencing intervention choices in autism spectrum disorders. Focus on Autism and Other Developmental Disabilities, 28 (2013): 138-146.
- Stewart, SL Dimos, T, & Poss, JW. Treatment seeking children who have experienced war zone trauma: Examining the mental health care planning needs. Child Psychiatry and Human Development (2023).
- Ministry of Children, Community, and Social Services (MCCSS; 2021). Ontario autism program: Urgent response service regional based proposal guidelines.
- Stewart SL, Hirdes, JP, Curtin-Telegdi N, et al. interRAI Child and Youth Mental Health (ChYMH) Assessment Form and User’s Manual. Version 9.3. Washington, DC: interRAI publications 2015.
- Stewart SL, Hirdes JP, McKnight M, et al. interRAI Child and Youth Mental Health Screener (ChYMH-S) Assessment Form and User’s Manual. Version 9.3. Washington, DC: interRAI publications 2017.
- Stewart SL, LaRose L, Gleason K, Nicolson R, McKnight, M., Knott, W., Currie, M., Morris, J. N., Berg, K., Björkgren, K., Declercq, A., Fries, B. E., Frijters, D., Gray, L., Head, M. J., Henrard, J. C., Hirdes, J. P., Ljunggren, G., Meehan, B., Smith, T. F., ...Topinková, E. (2015). interRAI Child and Youth Mental Health and Developmental Disability (ChYMH-DD) Assessment Form and User’s Manual. Version 9.3. interRAI, Washington DC.
- Stewart SL, Celebre A, Semovski V, et al. The interRAI Child and Youth Suite of Mental Health Assessment Instruments: An Integrated Approach to Mental Health Service Delivery. Frontiers in Psychiatry, 13 (2022).
- Hirdes JP, Van Everdingen C, Ferris J, et al. The interRAI suite of mental health assessment instruments: An integrated system for the continuum of care. Frontiers in Psychiatry, 10 (2020): 926.
- Stewart SL, Babcock SE (2020). InterRAI Child and Youth Mental Health Screener (ChYMH S): A psychometric evaluation and validation study. Child Psychiatry and Human Development, 51 (2020): 769-780.
- Lau C, Stewart SL, Saklofske DH, Hirdes JP. Development and psychometric validation of the interRAI ChYMH externalizing subscale. Clinical Child Psychology and Psychiatry, 26(2018): 295-305.
- Lau C, Stewart SL, Saklofske DH, Hirdes JP. The interRAI Child and Youth Mental Health Internalizing subscale: Scale development and psychometric properties. Psychiatric Research, 278 (2019): 235-241.
- Stewart SL, Hamza CA. The Child and Youth Mental Health Assessment (ChYMH): An examination among of the psychometric properties of an integrated assessment developed for clinically referred children and youth. Exceptionality Education International, 26 (2017): 5-20.
- Stewart SL, Poss JW, Thornley E, et al. Resource Intensity for Children and Youth: The Development of an Algorithm to Identify High Service Users in Children's Mental Health. Health Services Insights, 12 (2019): 1178632919827930.
- Stewart, SL, Celebre A, Hirdes, JP, & Poss, JW. Risk of suicide and self-harm in kids: The development of an algorithm to identify high-risk individuals within the children's mental health system. Child Psychiatry and Human Development, 51(2020): 913-924.
- Van den Berg B, Breur T. Merits of interactive decision tree building: Part 1. Journal of Targeting, Measurement and Analysis for Marketing, 15 (2007): 137-145.
- Cidav Z, Xie M, Mandell DS. Foster care involvement among medicaid-enrolled children with autism. Journal of Autism and Developmental Disorders, 48 (2018): 176-183.
- Hall-Lande J, Hewitt A, Mishra S, et al. Involvement of children with autism spectrum disorder (ASD) in the child protection system. Focus on Autism and Other Developmental Disabilities, 30 (2015): 237-248.
- Ekas NV, Lickenbrock DM, Whitman TL. Optimism, social support, and well-being in mothers of children with autism spectrum disorder. Journal of Autism and Developmental Disorders, 40 (2010): 1274-1284.
- Hayes SA, Watson SL (2013). The impact of parenting stress: A meta-analysis of studies comparing the experience of parenting stress in parents of children with and without autism spectrum disorder. Journal of Autism and Developmental Disorders, 43(2013): 629-642.
- Rogge N, Janssen J. The Economic Costs of Autism Spectrum Disorder: A Literature Review. Journal of Autism and Developmental Disorders, 49 (2019): 2873-2900.
- Benson PR. The impact of child symptom severity on depressed mood among parents of children with ASD: the mediating role of stress proliferation. Journal of Autism and Developmental Disorders, 36 (2006): 685-695
- Boyd BA. Examining the relationship between stress and lack of social support in mothers of children with autism. Focus on Autism and Other Developmental Disabilities, 17 (2002): 208-215.
- Tehee E, Honan R, Hevey D (2009). Factors contributing to stress in parents of individuals with autistic spectrum disorders. Journal of Applied Research in Intellectual Disabilities, 22 (2009): 34-42.
- Stewart SL, Vasudeva AS, Mistry D, & Poss, JW. The impact of child maltreatment on mental health outcome improvements amongst children and youth accessing community mental health care. Child abuse and neglect. 139 (2023): 106066.
- Stewart SL, Graham AA, Poss JW. Examining the Mental Health Indicators and Service Needs of Children Living with Foster Families. Children and Youth Services Review, 147 (2023). https://doi.org/10.1016/j.childyouth.2023.106833
- Gama CMF, Portugal LCL, Gonçalves RM, et al. The invisible scars of emotional abuse: a common and highly harmful form of childhood maltreatment. BMC psychiatry, 21 (2021): 1-14.
- Burns EE, Jackson JL, Harding HG. Child maltreatment, emotion regulation, and posttraumatic stress: The impact of emotional abuse. Journal of Aggression, Maltreatment & Trauma, 19 (2010): 801-819.
- Stewart SL, Withers A, Semovski V, Lapshina N (2023. Polyvictimization and impairments in functioning for children and youth with fetal alcohol spectrum disorder. Journal of Mental Health Research in Intellectual Disabilities.DOI: 10.1080/19315864.2023.22850.
- Olfson M, Gameroff MJ, Marcus SC, et al. Emergency treatment of young people following deliberate self-harm. Archives of General Psychiatry, 62 (2005): 1122-1128.
- Brent DA, Baugher M, Bridge J, et al. Age- and sex-related risk factors for adolescent suicide. Journal of the American Academy of Child and Adolescent Psychiatry, 38 (1999): 1497-1505.
- Cloutier P, Kennedy A, Maysenhoelder H, et al. Pediatric mental health concerns in the emergency department: caregiver and youth perceptions and expectations. Pediatric Emergency Care, 26 (2010): 99- 106.
- McGuire K, Erickson C, Gabriels RL, et al. Psychiatric Hospitalization of Children With Autism or Intellectual Disability: Consensus Statements on Best Practices. Journal of the American Academy of Child and Adolescent Psychiatry, 54 (2015): 969-971
- Cooke E, Smith V, Brenner M. Parents’ experiences of accessing respite care for children with Autism Spectrum Disorder (ASD) at the acute and primary care interface: a systematic review. BMC pediatrics, 20 (2020): 1-12.
- Zwaanswijk M, Van Der Ende, JAN, et al. Factors associated with adolescent mental health service need and utilization. Journal of the American Academy of Child & Adolescent Psychiatry, 42 (2003): 692-700.
- Olson L, Chen B, Ibarra C, et al. Externalizing behaviors are associated with increased parenting stress in caregivers of young children with autism. Journal of Autism and Developmental Disorders, 52 (2022): 975-986.
- Stewart SL, Toohey A, Poss, JW. iCCareD: the development of an algorithm to identify factors associated with distress among caregivers of children and youth referred for mental health services. Frontiers in psychiatry, 12 (2021): 737966.
- Stewart SL, Celebre A, Hirdes JP, et al. Risk of Injury to Others: The Development of an Algorithm to Identify Children and Youth at High-Risk of Aggressive Behaviours. Frontiers in Psychiatry, 12 (2022): 750625.
- Semovski V, King C, Lapshina N, Stewart SL. A cross-sectional examination of service complexity in youths with co-occurring autism spectrum disorder and psychiatric or medical diagnosis across service sectors. Frontiers in Psychology, 13 (2023): 1027373.
