Predicting Screening Factors for an Obesity Team’s Decision: A large Retrospective Cohort study
Article Information
Yentl Lodewijks1*, Jean-Paul de Zoete1, Roos van der Ven2, Angélique Schiffer3, Simon Nienhuijs1
1Department of Obesity Surgery, Catharina Hospital Eindhoven, Michelangelolaan 2, 5623 EJ Eindhoven, The Netherlands
2Department of Nutrition, Catharina Hospital Eindhoven, Michelangelolaan 2, 5623 EJ Eindhoven, The Netherlands
3Department of Medical Psychology, Catharina Hospital Eindhoven, Michelangelolaan 2, 5623 EJ Eindhoven, The Netherlands
*Corresponding Author: Yentl Lodewijks, Department of Obesity Surgery, Catharina Hospital Eindhoven, Michelangelolaan 2, 5623 EJ Eindhoven, The Netherlands.
Received: 18 November 2021; Accepted: 25 November 2021; Published: 11 January 2022
Citation: Lodewijks Y, de Zoete JP, Van der Ven R, Schiffer A, Nienhuijs S. Predicting Screening Factors for an Obesity Team’s Decision: A large Retrospective Cohort study. Journal of Surgery and Research 5 (2022): 35-45.
View / Download Pdf Share at FacebookAbstract
Background
The magnitude of the effect of bariatric surgery depends on the willingness and the ability of patients to adapt a healthier lifestyle. Therefore, it is worthwhile to know how to select patients for surgery and/or preoperative interventions.
Aim
To investigate the predictors for a disapproval at the time, direct approval or a prehabilitation program for bariatric surgery candidates after multidisciplinary evaluation.
Methods
Data on the SQ-48 total score, the RAND-36 total score, the general screening questionnaire, age, Body Mass Index (BMI), and the result of the multidisciplinary consultation were collected from all patients who participated in the screening process between February 2017 and February 2020. A multinomial logistic regression analysis was performed.
Results
Of the 2,063 included patients, 627 (30.4%) were approved for surgery, 1,275 (61.8%) received a preoperative trajectory advise and 161 (7.8%) were denied. Eleven variables appeared to be significant predictors for the result of the multidisciplinary consultation; gender, age, BMI, RAND-36 total score, SQ-48 total score, binging score, craving score, consciously eating, psychological help score, excessive drug use in the past and the impulsiveness score.
Conclusion
Although the predicting model might not be applicable to other centers, it could attribute to enhance patient selection and thereby improve healthcare logistics.
Keywords
Bariatric surgery screening, Multidisciplinary team, Preoperative program
Article Details
1. Introduction
Bariatric surgery is the only treatment with proven long-term results for patients with severe obesity [1-3]. However, the extent of surgery’s success depends on the willingness and ability to adapt to a healthier lifestyle. According to the interdisciplinary European guidelines on metabolic and bariatric surgery, patients eligible for bariatric surgery should follow an interdisciplinary evaluation [1]. This evaluation should be performed by an obesity team consisting of a surgeon, dietitian, psychologist, and a nurse. The team decides if a bariatric surgery candidate is psychologically and physically ready to make the required lifestyle changes for sustainable weight loss. The challenge for the multidisciplinary obesity team is to select patients with morbid obesity who are most likely to adhere to the necessary adjustments. Although this evaluation is widely accepted and practiced, there is no standardized assessment procedure described in international guidelines [1-3]. In addition to preoperative evaluation, some bariatric centers provide a preoperative prehabilitation program on exercise, diet and/or cognitive behavioral therapy. The positive effects of exercise and diet programs have been described in the enhanced recovery after surgery guidelines, such as reduced postoperative complications and reduced liver volume. However, the evidence is insufficient to standardize prehabilitation before bariatric surgery in clinical practice guidelines [3]. Additionally, a recent 12-year follow-up study showed that patients who were denied for surgery never sought weight loss surgery again although they eventually would qualify based on National Institutes of Health consensus criteria [4]. On the other hand, the extensive preoperative nutritional and psychological evaluation does not prevent the risk of weight regain [5,6]. To enhance the screening process and thus patient selection for an additional program, the retrospective cohort study aimed to investigate the predictors for disapproval at the time, approval. or a prehabilitation program for bariatric surgery candidates after multidisciplinary evaluation.
2. Materials and Methods
In this retrospective cohort study, all patients with no prior bariatric treatment and who completed the preoperative screening process between February 2017 and February 2020 were extracted from the hospital database after informed consent. This screening starts with an educative session, after which patients receive login information for an eHealth platform on which e-learnings, informational videos and three screening questionnaires were provided: the Symptom Questionnaire 48 (SQ-48), the RAND-36, and a general screening questionnaire (GSQ) (supplementary material S1) [7-9]. The 46-item GSQ is a non-validated general screening questionnaire regarding eating behavior, quality of life and intoxications. The SQ-48 focuses on symptoms of psychopathology in seven subscales: anxiety, depression, somatization, social phobia, agoraphobia, aggression and cognitive problems. The other two subscales measure vitality and functioning at work. The total score of the SQ-48 was calculated by adding all the subscales without the work subscale, wherein a higher score indicates more symptoms of psychopathology [7]. The RAND-36 measured the experienced health-related quality of life and comprises 9 domains scoring from 0 to 100 in which higher scores indicate a better quality of life [8]. A validated Dutch translation was used and performed according to the original protocol [10]. Lastly, because a higher RAND-36 total score indicates a better quality of life, it was negatively recoded and therefore matched with the direction of the SQ-48 total score. After these questionnaires were completed, patients returned for consultations with an obesity nurse, psychologist, dietitian and physiotherapist. Also, blood samples were taken to screen for vitamin deficiencies. Finally, the patients attended a group-session with a focus on commitment to the required lifestyle adjustments after surgery. Meanwhile, the results of the consultations were discussed by the obesity team according to the IFSO guidelines to determine if a patient was approved for surgery, denied, or required an additional prehabilitation program by a dietitian and/or psychologist [1]. A direct approval could lead to scheduling a bariatric procedure using shared decision making, in which patients receive standard information concerning preoperative eating habits and the use of multivitamins. If a preoperative conditioning program was advised, a patient could refuse and would be referred back to the general practitioner. Or the patient accepted the 3-6 months program before a bariatric procedure was scheduled. If the result of the multidisciplinary team consultation was disapproval at the time, patients were referred back to primary care for conservative treatment. Patients who dropped out during the screenings process, had previously primary surgery, or had missing data on more than two entire questionnaires were excluded. The focus of this study was investigating the predicting factors of the obesity team’s decision to guide a more efficient bariatric trajectory.
3. Data Analysis
Depending on normality, differences for continuous variables between multidisciplinary outcome groups were measured using the one-way analysis of variance or the Kruskal-Walis test. Differences between gender for continuous variables were analyzed using the independent t-test or the Mann-Whitney U test, also depending on normality. If normally distributed, continuous variables were presented as mean and standard deviation. Not normally distributed data were reported as median and interquartile range. Multinomial logistic regression was conducted to analyze factors that were associated with the dependent variable, the multidisciplinary recommendation; accepted for surgery, a preoperative trajectory or denied for surgery. To reduce the number of variables that could be used to build the model, a reliability analysis was carried out for the GSQ. For the RAND-36 and SQ-48 the total scores were used. The continuous variables were converted to a 10-point scale to increase the readability of the model. To determine significant independent variables from the GSQ, the chi-square test of independence and Cramér’s V were used (cut-off point 0.10) in the univariate analysis. The subsequent multivariate multinominal logistic regression analysis was conducted using only significant and clinically relevant variables based on clinical experience (cut-off point p < 0.10). Multicollinearity was assessed using the correlation matrix, and stepwise backward elimination to build the model. The crude odds ratio of the variables were calculated, and the adjusted odds ratio for the multivariate model. Statistical analyses were performed using SPSS software (version 26). Significance levels were set for p-value <0.05. Missing values were at random, no imputation method was used as the percentage missing was <5%.
4. Results
In total 2,304 patients were extracted from the hospital database, of which 241 were excluded due to missing data on more than two questionnaires (n = 188) or applied for revisional surgery (n = 53). The remaining 2,063 patients were used in the main analysis of which 627 (30.4%) patients were approved for surgery, 1,275 (61.8%) received a preoperative trajectory advice. The remaining 161 patients (7.8%) in the disapproved group were significantly heavier and younger, there was also a difference in gender between groups with the highest percentage female in the approved for surgery group (p < 0.001) (Table 1).
Table 1: Patient characteristics for multidisciplinary recommendation.
|
Approved for surgery |
Preoperative trajectory |
Denied for surgery |
P |
|
|
Number of patients (%) |
627 (30.4%) |
1275 (61.8%) |
161 (7.8%) |
|
|
Age, mean, years (SD) |
44.4 (10.9) |
42 (12.0) |
41.3 (13.7) |
0.001* |
|
Weight, median, kg (IQR) |
117 (108 – 130) |
120 (111 – 135) |
120 (110.5 – 133) |
0.001 |
|
Body mass index, median, kg/m2 (IQR) |
40.9 (38.6 – 43.8) |
41.4 (39.4 – 44.5) |
42.3 (39.7 – 45) |
0.001 |
|
Percentage female, % |
80.8 |
72.4 |
77 |
0.001** |
P value for Kruskal-Wallis test.
*One-wayanalysis of variance
**Chi-square
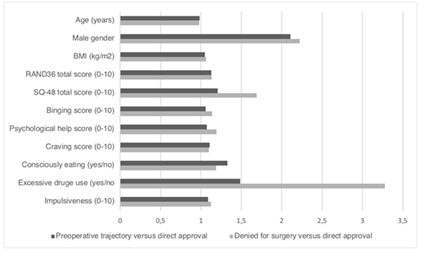
Following the reliability analysis, 10-point scales were made out of individual measured items such as the binging score, psychological help score, craving score and impulsiveness score. The final multinomial logistic regression model comprised 11 variables, representing an x2 of 331.641 (p < 0.001) indicating the model fits the data significantly better than a model without predictors (Table 2). The crude odds obtained from the univariate analyses differed from the adjusted ratio from the model for all variables except for age and Body Mass Index (BMI). The adjusted ratio for each group is represented in (Figure 1).
4.1 Preoperative trajectory versus direct approval for surgery
The adjusted odds ratio of the model with direct approval for surgery as reference category showed that the odds of receiving a preoperative trajectory is 2.1 times higher for males and 1.3 times higher if a patient did not eat consciously (table 2). For every 5 unit increase in BMI the odds increase by 25%, and for every 10 unit increase in age, the odds are 15.8% lower to receive a preoperative trajectory instead of direct approval for surgery. Regarding eating behavior, for every unit increase in the binging score the odds increase by 5.7% and for the craving score the odds increase by 10.7%. For every unit increase in SQ-48 score, RAND-36 score and impulsiveness score the odds increase by 21%, 13%, and 8.9% respectively. Patients who received psychological help or used psychotropic medications and therefore scored higher on the psychological help score elevated their odds by 7.1% Only the use of excessive drugs in the past did not significantly predict if patients were more likely to be administered a preoperative trajectory compared to direct approval. To predict the odds ratio for preoperative counseling compared to direct approval group equation 1 applies.
Equation 1
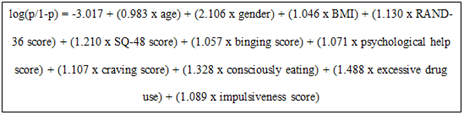
The variables gender, consciously eating and excessive drug use are dichotomous data and must be filled in as 0 if female, eating consciously and used excessive drugs in the past and as 1 if male, not eating consciously and did not use excessive drugs in the past.
4.2 Denied for surgery versus direct approval for surgery
The adjusted odds ratio of the model with direct approval for surgery as reference category shows that the odds of being denied for surgery is 2.2 times higher for male individuals and 3.3 times higher for patients who excessively used drugs in the past (Table 2). For every 5-unit increase in BMI the odds increase by 34%, and for every 10 unit increase in age the odds are 20.8% lower to be denied for surgery compared to direct approval. For to the binging score, every unit increase in binging the odds increase by 13.8%. For every unit increase in SQ-48 score, psychological help score and impulsiveness score the odds increase by 69%, 19.1% and 12.4% respectively. The variables RAND-36 total score, consciously eating and the craving score did not significantly predict if patients were rather denied for surgery compared to direct approval. To predict the odds ratio for denied for surgery compared to direct approval group equation 2 is applicable.
Equation 2
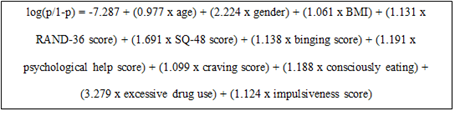
The variables gender, consciously eating and excessive drug use are dichotomous data and must be filled in as 0 if female, eating consciously and used excessive drugs in the past and as 1 if male, not eating consciously and did not use excessive drugs in the past.
Table 2: Multinomial logistic regression for the multidisciplinary recommendation
|
95% CI for Odds Ratio |
|||||
|
B (SE) |
Lower |
Odds ratio |
Upper |
P |
|
|
Preoperative counselling vs approved for surgery (ref) |
|||||
|
Intercept |
-3.017 (0.62) |
0.001 |
|||
|
Age (years) |
-0.018 (0.005) |
0.974 |
0.983 |
0.992 |
0.001 |
|
Gender (female/male) |
0.745 (0.135) |
1.617 |
2.106 |
2.743 |
0.001 |
|
Body mass index (kg/m2) |
0.045 (0.012) |
1.022 |
1.046 |
1.07 |
0.001 |
|
RAND36 total score (0-10) |
0.122 (0.036) |
1.052 |
1.13 |
1.213 |
0.001 |
|
SQ-48 total score (0-10) |
0.191 (0.052) |
1.094 |
1.21 |
1.339 |
0.038 |
|
Binging score (0-10) |
0.055 (0.027) |
1.003 |
1.057 |
1.113 |
0.001 |
|
Psychological help score (0-10) |
0.068 (0.019) |
1.032 |
1.071 |
1.111 |
0.001 |
|
Craving score (0-10) |
0.102 (0.033) |
1.038 |
1.107 |
1.181 |
0.002 |
|
Consciously eating (yes/no) |
0.284 (0.112) |
1.065 |
1.328 |
1.655 |
0.012 |
|
Excessive drug use (yes/no) |
0.397 (0.461) |
0.603 |
1.488 |
3.67 |
0.388 |
|
Impulsiveness (0-10) |
0.085 (0.026) |
1.034 |
1.089 |
1.146 |
0.001 |
|
Denied for surgery vs approved for surgery (ref) |
|||||
|
Intercept |
-7.287 (1.075) |
0.001 |
|||
|
Age (years) |
-.023 (0.009) |
0.961 |
0.977 |
0.994 |
0.007 |
|
Gender (female/male) |
0.799 (0.249) |
1.366 |
2.224 |
3.62 |
0.001 |
|
Body mass index (kg/m2) |
0.059 (0.020) |
1.021 |
1.061 |
1.103 |
0.003 |
|
RAND36 total score (0-10) |
0.123 (0.073) |
0.981 |
1.131 |
1.305 |
0.09 |
|
SQ-48 total score (0-10) |
0.525 (0.087) |
1.426 |
1.691 |
2.004 |
0.001 |
|
Binging score (0-10) |
0.129 (0.049) |
1.033 |
1.138 |
1.253 |
0.009 |
|
Psychological help score (0-10) |
0.175 (0.030) |
1.123 |
1.191 |
1.263 |
0.001 |
|
Craving score (0-10) |
0.094 (0.061) |
0.974 |
1.099 |
1.239 |
0.126 |
|
Consciously eating (yes/no) |
0.172 (0.207) |
0.791 |
1.188 |
1.782 |
0.406 |
|
Excessive drug use (yes/no) |
1.188 (0.551) |
1.113 |
3.279 |
9.661 |
0.031 |
|
Impulsiveness (0-10) |
0.117 (0.046) |
1.028 |
1.124 |
1.23 |
0.01 |
5. Discussion
A multinomial logistic regression model was built using three screening questionnaires and basic characteristics from 2,063 patients to investigate the predicting factors for the obesity team’s decision: approval for surgery, denial at the time, or a preoperative prehabilitation program. Eleven variables appeared to be significant predictors, i.e., gender, age, BMI, RAND-36 total score, SQ-48 total score, binging score, craving score, consciously eating, psychological help score, excessive drug use in the past and the impulsiveness score. All variables were positively correlated with a higher odds for receiving prehabilitation advice or being denied for surgery compared to the direct approval group, except for age.
Men had a significantly higher chance for either a preoperative program advice or refusal for surgery. This finding is consistent with that of Wee et al. who examined patients’ consideration for surgery and showed that weight loss was more desired by women than men and therefore women might be more motivated [11]. Furthermore, compared to women, men were less likely to have accurate weight perception, weight dissatisfaction, and attempted weight loss [12].
In our study, denied patients were significantly heavier and younger (Table 1). Despite being statistically significant, it is debatable if the absolute difference is clinically relevant. The predictive model also showed that younger and heavier participants had a higher chance of being denied for surgery or advised a preoperative program. Age and preoperative BMI as predictive factors in bariatric surgery remains controversial. For instance, Ahmed et al. stated that younger bariatric patients had a lower risk of 6-months postoperative complications [13]. Other studies also showed that older age was associated with less successful weight loss one year after surgery [14,15]. On the other hand, Altieri et al. reported that patients between 30 and 50 years of age and with higher preoperative weights may be more successful in losing weight in a 3 to 6-months during preoperative weight loss program including behavioral modifications and nutrition counseling [16]. Also, higher preoperative weights appeared to be positively correlated to postoperative weight loss up to 60 months [17]. On the contrary, other authors found that greater preoperative BMI was negatively associated with postoperative weight loss up to 135 months [6,14].
Current drug abuse is a contraindication for bariatric surgery, prior abuse is less obvious [1]. Tedesco et al. showed that patients with substance abuse achieve equivalent weight loss at 6 and 12 months postoperative compared to patients without alcohol or drug abuse [18]. A review of 2019 by Kanji et al. supported this belief, but it may contribute to increased substance abuse after bariatric surgery [19]. New-onset abuse is also evident after surgery, the follow-up in our center favorably endures for 5 years [20,21]. In our model, the odds of being denied for surgery was 3.3 times higher for patients who abused drugs in the past compared to patients who did not.
The variables concerning eating behavior were scores on binging, craving, impulsiveness and whether patients ate consciously. Higher scores were all associated with lower chances of direct approval. Although eating disorders are a contraindication for surgery, it seemed as simple as a negative answer to the question ‘do you eat consciously?’ as it increased the odds by 30% for a preoperative program [1].
Likewise was the influence of the predicting variables regarding psychological help and the SQ-48, higher scores per unit increased the odds for disapproval with 19.1% and 69% respectively compared to direct approval for surgery. Probably because the obesity team understands that the presence of psychopathology predicts less BMI reduction and estimated weight loss 5 years after surgery [22]. Surprisingly, the RAND-36 score did not significantly predict the odds of being denied for surgery. This finding was unexpected as health-related quality of life is one of the motivating factors for seeking bariatric surgery [23]. Its influence is most likely overruled by the other variables, as the univariate analysis showed an increased probability of 52% for every increase in the RAND-36 score. This suggests that the eleven variables should only be considered together within this model, not as independent factors. It remains debatable how to imply this predicting model in clinical practice. Every patient should be screened when referred for a bariatric procedure, however a denial at the time could be a misjudgment and there is no consensus for the use of a preconditioning program [1,4, 24]. Nevertheless, many obesity centers administer an additional program but it remains a challenge to what extent and by which professional the screening for bariatric surgery should consist. In that case, this model could improve the screening process logistics. For example, patients could receive extended standard preoperative education, could be guided by more experienced healthcare professionals or receive more postoperative guidance.
Several limitations apply to the results. The odds were calculated based on the decision of our unique multidisciplinary team and therefore limiting generalizability. Furthermore, the GSQ has not been validated yet nor is the use of the SQ-48 questionnaire standard for the obesity centers in the Netherlands [25-27]. Nevertheless, the elements from these questionnaires and therefore comparable demands for bariatric surgery are likely to be universal. Another limitation was the content of the prehabilitation program as well as the possibility for conservative treatment after denial. Lastly, the model has not been validated yet prospectively or in other settings. The authors have planned to perform this study design in the future.
6. Conclusion
A multinomial logistic regression was built using three screening questionnaires and basic characteristics from 2,063 patients to investigate the predicting factors for the obesity team’s decision. Although the exact model might not apply to other bariatric centers, the elements found are likely to be universal. This predictive model could attribute to enhance patient selection and thereby improve healthcare logistics.
Ethical approval
No formal ethical approval was necessary in line with legislation on non-WMO research in the Netherlands, and as the accessed data was fully anonymized. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Conflict of interests
The authors declare that they have no conflict of interest.
Informed consent
Informed consent was obtained from all individual participants included in the study.
References
- Fried M, Yumuk V, Oppert JM, et al. Interdisciplinary European guidelines on metabolic and bariatric surgery. Obes Surg 24 (2014): 42-55.
- Mechanick JI, Apovian C, Brethauer S, et al. Clinical practice guidelines for the perioperative nutrition, metabolic, and nonsurgical support of patients undergoing bariatric procedures - 2019 update: cosponsored by American Association of Clinical Endocrinologists/American College of Endocrinology, The Obesity Society, American Society for Metabolic & Bariatric Surgery, Obesity Medicine Association, and American Society of Anesthesiologists. Surg Obes Relat Dis 16 (2020): 175-247.
- Thorell A, MacCormick AD, Awad S, et al. Guidelines for Perioperative Care in Bariatric Surgery: Enhanced Recovery After Surgery (ERAS) Society Recommendations. World J Surg 40 (2016): 2065-2083.
- Kappus MS, Phillips BT, Zenquis N, et al. Unintended consequences for patients denied bariatric surgery: a 12-year follow-up. Surg Obes Relat Dis 16 (2020): 1458-1462.
- King WC, Hinerman AS, Courcoulas AP. Weight regain after bariatric surgery: a systematic literature review and comparison across studies using a large reference sample. Surg Obes Relat Dis 16 (2020): 1133-44.
- Csendes A, Burgos AM, Martinez G, et al. Loss and Regain of Weight After Laparoscopic Sleeve Gastrectomy According to Preoperative BMI : Late Results of a Prospective Study (78-138 months) with 93% of Follow-Up. Obes Surg 28 (2018): 3424-3430.
- Carlier I, Schulte-Van Maaren Y, Wardenaar K, et al. Development and validation of the 48-item Symptom Questionnaire (SQ-48) in patients with depressive, anxiety and somatoform disorders. Psychiatry Res 200 (2012): 904-910.
- VanderZee KI, Sanderman R, Heyink JW, et al. Psychometric qualities of the RAND 36-Item Health Survey 1.0: a multidimensional measure of general health status. Int J Behav Med 3 (1996):104-122.
- Hinnen CDP, Salet S. Richtlijn bariatrische psychologie (2021).
- Hays RD, Morales LS. The RAND-36 measure of health-related quality of life. Ann Med 33 (2001): 350-357.
- Wee CC, Huskey KW, Bolcic-Jankovic D, et al. Sex, race, and consideration of bariatric surgery among primary care patients with moderate to severe obesity. J Gen Intern Med 29 (2014): 68-75.
- Tsai SA, Lv N, Xiao L, et al. Gender Differences in Weight-Related Attitudes and Behaviors Among Overweight and Obese Adults in the United States. Am J Mens Health 10 (2016): 389-398.
- Ahmed AE, Alanazi WR, BI AL, et al. Impact of age on postoperative complications following bariatric surgery. Qatar Med J (2019): 11.
- Nickel F, de la Garza JR, Werthmann FS, et al. Predictors of Risk and Success of Obesity Surgery. Obes Facts 12 (2019): 427-439.
- Cadena-Obando D, Ramirez-Renteria C, Ferreira-Hermosillo A, et al. Are there really any predictive factors for a successful weight loss after bariatric surgery? BMC Endocr Disord 20 (2020): 20.
- Altieri MS, Tuppo C, Telem DA, et al. Predictors of a successful medical weight loss program. Surg Obes Relat Dis 11 (2015): 431-435.
- Seyssel K, Suter M, Pattou F, et al. A Predictive Model of Weight Loss After Roux-en-Y Gastric Bypass up to 5 Years After Surgery: a Useful Tool to Select and Manage Candidates to Bariatric Surgery. Obes Surg 28 (2018): 3393-3399.
- Tedesco M, Hua WQ, Lohnberg JA, et al. A prior history of substance abuse in veterans undergoing bariatric surgery. J Obes (2013): 740312.
- Kanji S, Wong E, Akioyamen L, et al. Exploring pre-surgery and post-surgery substance use disorder and alcohol use disorder in bariatric surgery: a qualitative scoping review. Int J Obes (Lond) 43 (2019): 1659-1674.
- Ivezaj V, Saules KK, Schuh LM. New-onset substance use disorder after gastric bypass surgery: rates and associated characteristics. Obes Surg 24 (2014): 1975-1980.
- King WC, Chen JY, Courcoulas AP, et al. Alcohol and other substance use after bariatric surgery: prospective evidence from a U.S. multicenter cohort study. Surg Obes Relat Dis 13 (2017): 1392-1402.
- Oltmanns JR, Rivera Rivera J, Cole J, et al. Personality psychopathology: Longitudinal prediction of change in body mass index and weight post-bariatric surgery. Health Psychol 39 (2020): 245-254.
- Andersen JR, Aasprang A, Karlsen TI, et al. Health-related quality of life after bariatric surgery: a systematic review of prospective long-term studies. Surg Obes Relat Dis 11 (2015): 466-473.
- Marshall S, Mackay H, Matthews C, et al. Does intensive multidisciplinary intervention for adults who elect bariatric surgery improve post-operative weight loss, co-morbidities, and quality of life? A systematic review and meta-analysis. Obes Rev 21 (2020): 13012.
- Aarts F, Hinnen C, Gerdes VE, et al. Psychologists' evaluation of bariatric surgery candidates influenced by patients' attachment representations and symptoms of depression and anxiety. J Clin Psychol Med Settings 21 (2014): 116-123.
- Al Amer R, Al Khalifa K, Alajlan SA, et al. Analyzing the Psychometric Properties of the Short Form-36 Quality of Life Questionnaire in Patients with Obesity. Obes Surg 28 (2018): 2521-2527.
- Poelemeijer YQM, van der Knaap ETW, Marang-van de Mheen PJ, et al. Measuring quality of life in bariatric surgery: a multicentre study. Surg Endosc 34 (2020): 5522-5532.