Post-Operative Complications Following Emergency Laparotomy are Common and Associated with increased Late Mortality - A Retrospective Multi-Centre study
Article Information
Shivam Sharma, Joseph Alderman, Dhruv Parekh, David Thickett, Jaimin M Patel*
Department of Anaesthesia and Intensive Care Medicine, The University of Birmingham, Edgbaston, Birmingham, B15 2TT, United Kingdom
*Corresponding author: Jaimin M Patel PhD, FRCA, Department of Anaesthesia and Intensive Care Medicine, The University of Birmingham, Edgbaston, Birmingham, B15 2TT, United Kingdom
Received: 30 November 2021; Accepted: 07 December 2021; Published: 06 January 2022
Citation: Shivam Sharma, Joseph Alderman, Dhruv Parekh, David Thickett, Jaimin M Patel. Post-Operative Complications Following Emergency Laparotomy are Common and Associated with increased Late Mortality - A Retrospective Multi-Centre study. Journal of Surgery and Research 5 (2022): 24-34.
View / Download Pdf Share at FacebookAbstract
Emergency abdominal surgery, often termed emergency laparotomy, is a common surgical procedure undertaken in the United Kingdom (U.K), with approximately 30000 procedures annually. Patients presenting for emergency abdominal surgery are heterogeneous and present with diverse pathology, resulting in challenges for the surgical, anaesthetic and critical care team that manage them. Emergency laparotomy, by its very nature is high-risk surgery, with an estimated 30-day mortality in the U.K of 11%, which is over 10 times greater than the mortality of patients undergoing major elective surgery (e.g. cardiac, vascular and oncological surgery) and a median hospital length of stay (LOS) of 12-days. Risk factors associated with poorer outcomes from emergency laparotomy have been identified by the National Emergency Laparotomy Audit (NELA) and include advancing age, with each decade above the age of 50 being associated with increasing risk. Additional risk factors include an American Society of Anaesthesia (ASA) status of 3 or more and Portsmouth- Physiological and Operative Severity Score for the enumeration of Mortality and morbidity (P-POSSUM) risk of death of greater than 5%. The development of post-operative pulmonary complications (PPCs) is a composite definition for a variety of respiratory complications that occur following surgery. They range from clinically significant bronchospasm and atelectasis, through to the development of pneumonia and the acute respiratory distress syndrome (ARDS). The incidence following elective major abdominal surgery has been estimated at 11.9% and is associated poorer outcomes with increased length of hospital stay, increased re-admissions and a higher mortality. Although emergency surgery is well established as a significant risk factor for the development of PPCs, the incidence is not well established. This study aimed to establish the incidence of PPCs in a cohort of patients undergoing emergency laparotom
Keywords
Post-operative Pulmonary Complications, Emergency laparotomy, Mortality, Re-admissions, Outcomes
Post-operative Pulmonary Complications articles; Emergency laparotomy articles; Mortality articles; Re-admissions articles; Outcomes articles
Post-operative Pulmonary Complications articles Post-operative Pulmonary Complications Research articles Post-operative Pulmonary Complications review articles Post-operative Pulmonary Complications PubMed articles Post-operative Pulmonary Complications PubMed Central articles Post-operative Pulmonary Complications 2023 articles Post-operative Pulmonary Complications 2024 articles Post-operative Pulmonary Complications Scopus articles Post-operative Pulmonary Complications impact factor journals Post-operative Pulmonary Complications Scopus journals Post-operative Pulmonary Complications PubMed journals Post-operative Pulmonary Complications medical journals Post-operative Pulmonary Complications free journals Post-operative Pulmonary Complications best journals Post-operative Pulmonary Complications top journals Post-operative Pulmonary Complications free medical journals Post-operative Pulmonary Complications famous journals Post-operative Pulmonary Complications Google Scholar indexed journals Emergency laparotomy articles Emergency laparotomy Research articles Emergency laparotomy review articles Emergency laparotomy PubMed articles Emergency laparotomy PubMed Central articles Emergency laparotomy 2023 articles Emergency laparotomy 2024 articles Emergency laparotomy Scopus articles Emergency laparotomy impact factor journals Emergency laparotomy Scopus journals Emergency laparotomy PubMed journals Emergency laparotomy medical journals Emergency laparotomy free journals Emergency laparotomy best journals Emergency laparotomy top journals Emergency laparotomy free medical journals Emergency laparotomy famous journals Emergency laparotomy Google Scholar indexed journals Mortality articles Mortality Research articles Mortality review articles Mortality PubMed articles Mortality PubMed Central articles Mortality 2023 articles Mortality 2024 articles Mortality Scopus articles Mortality impact factor journals Mortality Scopus journals Mortality PubMed journals Mortality medical journals Mortality free journals Mortality best journals Mortality top journals Mortality free medical journals Mortality famous journals Mortality Google Scholar indexed journals Re-admissions articles Re-admissions Research articles Re-admissions review articles Re-admissions PubMed articles Re-admissions PubMed Central articles Re-admissions 2023 articles Re-admissions 2024 articles Re-admissions Scopus articles Re-admissions impact factor journals Re-admissions Scopus journals Re-admissions PubMed journals Re-admissions medical journals Re-admissions free journals Re-admissions best journals Re-admissions top journals Re-admissions free medical journals Re-admissions famous journals Re-admissions Google Scholar indexed journals Emergency abdominal surger articles Emergency abdominal surger Research articles Emergency abdominal surger review articles Emergency abdominal surger PubMed articles Emergency abdominal surger PubMed Central articles Emergency abdominal surger 2023 articles Emergency abdominal surger 2024 articles Emergency abdominal surger Scopus articles Emergency abdominal surger impact factor journals Emergency abdominal surger Scopus journals Emergency abdominal surger PubMed journals Emergency abdominal surger medical journals Emergency abdominal surger free journals Emergency abdominal surger best journals Emergency abdominal surger top journals Emergency abdominal surger free medical journals Emergency abdominal surger famous journals Emergency abdominal surger Google Scholar indexed journals American Society of Anaesthesia articles American Society of Anaesthesia Research articles American Society of Anaesthesia review articles American Society of Anaesthesia PubMed articles American Society of Anaesthesia PubMed Central articles American Society of Anaesthesia 2023 articles American Society of Anaesthesia 2024 articles American Society of Anaesthesia Scopus articles American Society of Anaesthesia impact factor journals American Society of Anaesthesia Scopus journals American Society of Anaesthesia PubMed journals American Society of Anaesthesia medical journals American Society of Anaesthesia free journals American Society of Anaesthesia best journals American Society of Anaesthesia top journals American Society of Anaesthesia free medical journals American Society of Anaesthesia famous journals American Society of Anaesthesia Google Scholar indexed journals acute respiratory distress syndrome articles acute respiratory distress syndrome Research articles acute respiratory distress syndrome review articles acute respiratory distress syndrome PubMed articles acute respiratory distress syndrome PubMed Central articles acute respiratory distress syndrome 2023 articles acute respiratory distress syndrome 2024 articles acute respiratory distress syndrome Scopus articles acute respiratory distress syndrome impact factor journals acute respiratory distress syndrome Scopus journals acute respiratory distress syndrome PubMed journals acute respiratory distress syndrome medical journals acute respiratory distress syndrome free journals acute respiratory distress syndrome best journals acute respiratory distress syndrome top journals acute respiratory distress syndrome free medical journals acute respiratory distress syndrome famous journals acute respiratory distress syndrome Google Scholar indexed journals Portsmouth- Physiological and Operative Severity Score articles Portsmouth- Physiological and Operative Severity Score Research articles Portsmouth- Physiological and Operative Severity Score review articles Portsmouth- Physiological and Operative Severity Score PubMed articles Portsmouth- Physiological and Operative Severity Score PubMed Central articles Portsmouth- Physiological and Operative Severity Score 2023 articles Portsmouth- Physiological and Operative Severity Score 2024 articles Portsmouth- Physiological and Operative Severity Score Scopus articles Portsmouth- Physiological and Operative Severity Score impact factor journals Portsmouth- Physiological and Operative Severity Score Scopus journals Portsmouth- Physiological and Operative Severity Score PubMed journals Portsmouth- Physiological and Operative Severity Score medical journals Portsmouth- Physiological and Operative Severity Score free journals Portsmouth- Physiological and Operative Severity Score best journals Portsmouth- Physiological and Operative Severity Score top journals Portsmouth- Physiological and Operative Severity Score free medical journals Portsmouth- Physiological and Operative Severity Score famous journals Portsmouth- Physiological and Operative Severity Score Google Scholar indexed journals post-operative pulmonary complications articles post-operative pulmonary complications Research articles post-operative pulmonary complications review articles post-operative pulmonary complications PubMed articles post-operative pulmonary complications PubMed Central articles post-operative pulmonary complications 2023 articles post-operative pulmonary complications 2024 articles post-operative pulmonary complications Scopus articles post-operative pulmonary complications impact factor journals post-operative pulmonary complications Scopus journals post-operative pulmonary complications PubMed journals post-operative pulmonary complications medical journals post-operative pulmonary complications free journals post-operative pulmonary complications best journals post-operative pulmonary complications top journals post-operative pulmonary complications free medical journals post-operative pulmonary complications famous journals post-operative pulmonary complications Google Scholar indexed journals emergency surgery articles emergency surgery Research articles emergency surgery review articles emergency surgery PubMed articles emergency surgery PubMed Central articles emergency surgery 2023 articles emergency surgery 2024 articles emergency surgery Scopus articles emergency surgery impact factor journals emergency surgery Scopus journals emergency surgery PubMed journals emergency surgery medical journals emergency surgery free journals emergency surgery best journals emergency surgery top journals emergency surgery free medical journals emergency surgery famous journals emergency surgery Google Scholar indexed journals
Article Details
1. Background
Emergency abdominal surgery, often termed emergency laparotomy, is a common surgical procedure undertaken in the United Kingdom (U.K), with approximately 30000 procedures annually [1]. Patients presenting for emergency abdominal surgery are heterogeneous and present with diverse pathology, resulting in challenges for the surgical, anaesthetic and critical care team that manage them. Emergency laparotomy, by its very nature is high-risk surgery, with an estimated 30-day mortality in the U.K of 11%, which is over 10 times greater than the mortality of patients undergoing major elective surgery (e.g. cardiac, vascular and oncological surgery) and a median hospital length of stay (LOS) of 12-days [2,3]. Risk factors associated with poorer outcomes from emergency laparotomy have been identified by the National Emergency Laparotomy Audit (NELA) and include advancing age, with each decade above the age of 50 being associated with increasing risk. Additional risk factors include an American Society of Anaesthesia (ASA) status of 3 or more and Portsmouth- Physiological and Operative Severity Score for the enumeration of Mortality and morbidity (P-POSSUM) risk of death of greater than 5% [3]. The development of post-operative pulmonary complications (PPCs) is a composite definition for a variety of respiratory complications that occur following surgery. They range from clinically significant bronchospasm and atelectasis, through to the development of pneumonia and the acute respiratory distress syndrome (ARDS) [4]. The incidence following elective major abdominal surgery has been estimated at 11.9% and is associated poorer outcomes with increased length of hospital stay, increased re-admissions and a higher mortality [5]. Although emergency surgery is well established as a significant risk factor for the development of PPCs, the incidence is not well established. This study aimed to establish the incidence of PPCs in a cohort of patients undergoing emergency laparotomy and the consequences on patient outcomes.
2. Methods
2.1 Design and Setting
A retrospective analysis was conducted of patient that underwent emergency laparotomy between December 1st 2014 and November 31st 2015 at University Hospital Birmingham National Health Service (NHS) Foundation trust and Heartlands Hospital, Birmingham (part of the Heart of the England NHS Foundation Trust). The two hospitals combined serve a population of approximately 1 million people, have a total of 3000 hospital beds, with 120 critical care beds and offer acute surgical services. The study did not require ethical approval or research registration. This was confirmed by the online National Research Ethics Survey decision tool and the research and development departments at the University of Birmingham [6]. Patients were identified using the NELA databases for each NHS trust which collects local hospital data for emergency laparotomy, however this is not a fully comprehensive database. Therefore, in addition to this, each hospital’s electronic patient records (EPR) were searched over the same timeframe to cross-reference patients and collect patients that had not been initially identified using the NELA database.
2.2 Data collected
Individual patient data was collected using the NELA database which collects information to include baseline demographics, date of operation, risk stratification using ASA score, P-POSSUM, serum lactate and serum creatinine, operative details, critical care service utilisation post-operatively and in-hospital outcomes. This was supported by electronic EPR systems at each trust to collect data for PPCs, unplanned hospital re-admissions and mortality at 90-days, 180-days and 365-days.
2.3 Definition of High-Risk and Low-Risk patients
As described previously patients presenting for emergency surgery are heterogeneous with different groups of patients having variable outcomes. Patients were therefore categorized as high or low-risk based upon either an an ASA ?3 or a P-POSSUM predicted mortality of ?5% . This categorization was based on evidence from 30000 cases analysed by the NELA group, that suggested that adverse outcomes occur if a patient meets any one of these three variables(3).
2.4 Diagnosis of PPCs
PPCs were identified using the Melbourne Group Score. This is a validated daily screening tool for identifying patients with PPCs and has been used previously in patients undergoing major abdominal and thoracic surgery(7). The score consists of 8 dichotomous factors that include microbiological, clinical and physiological parameters, with a score of 4 or more indicating the development of a clinically significant PPCs that are likely to adversely affect the patient’s clinical course (figure 1). Patients EPRs were screened daily from the day of operation till the seventh post-operative day for PPCs using the Melbourne Group Score. The daily score was recorded and where a patient met the diagnosis of a PPC the post-operative day of occurrence was recorded.
2.5 Statistical Analysis
Continuous data was analysed for normality using a D’Agostino and Pearson omnibus normality test. All data were non-parametric and therefore all continuous is represented as median and inter-quartile ranges (IQR), with comparative tests between groups analysed using a Mann-Whitney U test. Categorical data are represented as numbers and proportions with any comparative tests performed using a Fisher’s exact or Chi-squared test. Kaplan-Meier analysis and odd’s ratio were performed to quantify the consequences of PPC development on survival and re-admissions. These were calculated using a log-rank Mantel-Cox Chi-squared test. All data analysis was performed using GraphPad PRISM version 6 (La Jolla, USA). Additionally, to identify factors that may predict the development of PPCs Cox-logistical regression was carried out using SPSS. Significance was taken as a p-value of less than 0.05.
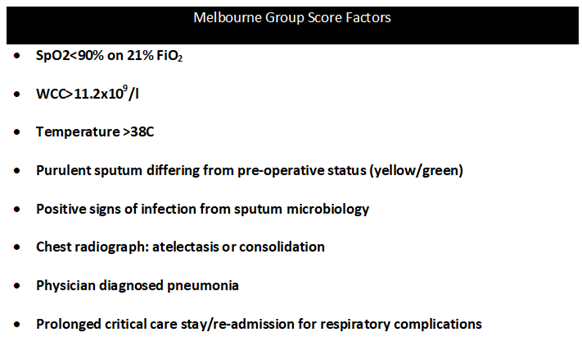
Figure 1: The Melbourne Group Score. A post-operative pulmonary complicsation can be diagnosed if 4 or more of these factors are present.
3. Results
A total of 437 patients were identified as having undergone emergency laparotomy between the 1st of December 2014 and 31st November 2015. 75 cases were excluded due to duplication or incorrect coding of the procedures. Of the 362 remaining patients, 136 were classified as low-risk patients and 226 as being high-risk (figure 2).
3.1 Demographics
The median age of the entire cohort was 62 years (IQR 45-74 years), with 47% (n=170) of patients being male. The majority of patients (64% n=230) had an ASA ³3 with a median P-POSSUM score of 6% (2.3-19.3%). 48% (n=174) of patients were admitted directly to critical care units (CCU) following surgery. The median length of hospital stay was 13 days (IQR 6-25), with a 30-day mortality of 12% (n=44). (see table 1). High-risk patients were older (67 years {IQR 51-77} vs. 48 {IQR 38-66}; p<0.001) and had higher P-POSSUM predicted mortality scores (10.6% {IQR 5.6-31.3} vs. 2% {IQR 1.3-3.1}; p<0.001). These patients also had higher plasma creatinine (74mmol/L {59-104mmol/L} vs. 70mmol/L {58-80mmol/L}; p=0.003) and lactate levels (1.8mmol/L {1.2-3.5mmol/L} vs. 1.5mmol/L {1.1-2.6mmol/L}; p=0.044) at the time of surgery. High-risk patients had significantly poorer outcomes with an increased length of hospital stay (17days {IQR 9-32} vs. 9days {IQR 6-15}; p<0.001) and an increased 30-day mortality (14% vs. 1.4%; p<0.001).

Figure 2: This image shows an overall summary of our starting cohort being broken down into separate groups. 75 patients were excluded as they were either duplicated or the procedure was incorrectly coded.
3.2 Incidence of PPCs
The incidence of PPCs within the entire cohort was 30% (n=108). The burden of PPCs were almost entirely in the high-risk patients with an incidence of 37% (n=84), with only 6% (n=8) of the low-risk patients developing a PPC. The demographics of patients who were diagnosed with and without a PPC are shown in table 2. There were no significant differences between these patients, although patients who did develop a PPCs showed a trend towards an increased pre-operative P-POSSUM predicted mortality scores and were more likely to be admitted directly to CCU (85% vs. 71%; p=0.02). Importantly, there were no differences between these two cohorts in baseline respiratory or cardiovascular disease as measured by the P-POSSUM risk score. The commonest post-operative day to develop a PPC was day 3(median; IQR 1-4days).
|
All Patients |
Low Risk Patients |
High-Risk Patients |
p-values |
|
|
N=362 |
N=136 |
N=226 |
||
|
Age |
62 (45-74) years |
48 (38-66) |
67 (51-77) |
<0.001 |
|
Sex, male:female (%) |
47:53:00 |
49:51:00 |
44:58:00 |
|
|
ASA |
||||
|
01-Feb |
37% (132) |
100% |
24% (54) |
|
|
≥3 |
64% (230) |
0% |
||
|
76% (172) |
||||
|
P-POSSUM (mortality) |
6% (2.3-19.3%) |
2% (1.1-3.1%) |
10.6 (5.6-31.3) |
<0.001 |
|
ICU admission: |
||||
|
P-POSSUM 5-10% (N=72) |
11% (40) |
0 |
34 (20%) |
|
|
P-POSSUM >10% (N=156) |
37% (134) |
0 |
||
|
Total (232) |
48% (174) |
Total (0) |
123 (72%) |
|
|
Total (170) |
||||
|
Length of stay |
13 (6-25) days |
9 (6-15) days |
17 (9-32) days |
<0.001 |
|
30-day Mortality |
12% (44) |
1.4% (2) |
14% (42) |
<0.001 |
|
PPC |
30% |
6% |
37% |
<0.001 |
Table 1: Demographics and risk stratification of our cohort are showing in this table. The table demonstrates high risk patients ended up having significantly worse outcomes than low risk patients.
|
Demographics of patients with a PPC and without a PPC |
|||
|
High Risk Laparotomies |
No PPC |
PPC |
p-value |
|
N=142 |
N=84 |
||
|
Age, years |
67 (51-77) |
68.5 (51.5-78) |
0.88 |
|
P-POSSUM %(mortality) |
12.3 (6.5-31.2) |
19.4 (7.4-41.6) |
0.07 |
|
No dyspnoea (n) |
67% (92) |
62% (52) |
0.61* |
|
No failure (n) |
53% (96) |
61% (51) |
0.69* |
|
Admission to ICU (n) |
71% (101) |
85% (71) |
0.02* |
Table 2: Table showing the differences in demographics between patients who developed a PPC after laparotomy vs patients who did not.
3.3 Outcomes in patients with PPCs
Patients that developed a PPC during the first 7 post-operative days had poorer outcomes compared to patients who did not develop a PPCs. This included a median increase in CCU length of stay by 1-day (p-0.002) and a median increase in hospital length of stay of 3days (p=0.01). There was no difference in 30-day mortality, however there was a significant increase in both 90, 180 and 365-day mortality (see figure 3). In addition, the number of re-admissions in patients who developed a PPC was increased at similar time-points.
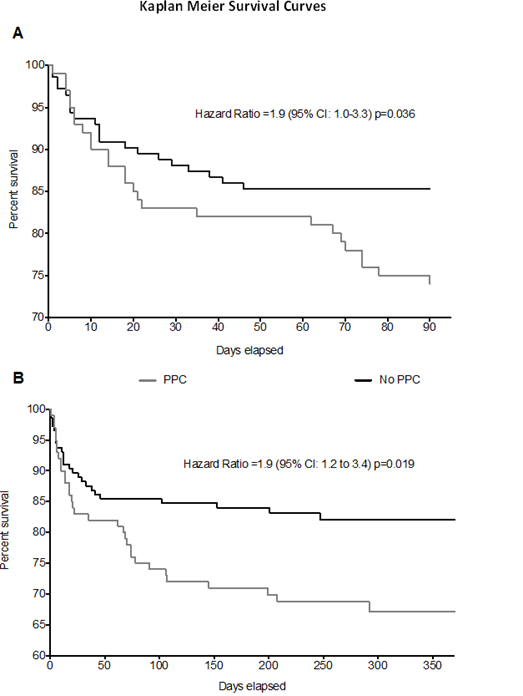
Figure 3: Kaplan Meier survival curves for our cohort over 360 days. PPC patients had significantly higher 90, 180 and 365 day mortality rates.
3.4 Multivariate analysis
Cox’s multiple regression was performed on factors that may have predicted the development of a PPC in the high-risk cohort. No individual factors predicted the likelihood of PPC development in the high-risk cohort.
4. Discussion
Emergency abdominal surgery by its very nature is associated with increased morbidity and mortality. This study demonstrates that the well validated ASA and P-POSSUM scoring tools in conjunction with age can be used to identify patients at high risk of developing PPCs. Importantly we demonstrate that the patients who develop a PPC overall have poorer outcomes and consume more resources. Although, in-hospital or 30-day mortality was no different, patients who developed a PPC did stay in CCU for longer and have prolonged hospital stays compared to those who did not develop a PPC. Longer term outcomes, were also poorer, with unplanned hospital readmissions and mortality increased at all time points. The pathophysiology of PPCs following emergency surgery is multi-factorial and complex. Post-operative pain following surgery is implicated as this prevents patients from ventilating dependent portions of the lung(8). The site of the surgical incision is also relevant with incisions that extend above the umbilicus, or sub-phrenic incisions causing significant respiratory compromise. Control of pain is a key principal of anaesthesia and post-operative management and regional anaesthesia, especially the use of neuro-axial blockade, can effectively mitigate against these factors in the elective operative setting. In emergency surgery, neuro-axial blockade may be relatively contra-indicated due to physiological and coagulation abnormalities and as such are utilised less frequently. Patients undergoing emergency abdominal surgery are heterogenous with multiple pathologies leading to their definitive operative procedures. These can range from blunt or penetrating trauma causing internal visceral damage with/without major haemorrhage, to contained bowel obstruction to fulminant peritonitis or ischaemic bowel. An added complexity is the underlying disease processes in non-trauma patients are varied, such as bowel cancer, inflammation (diverticulitis) and anatomical abnormalities (hernias/volvulus). Furthermore, these patients may present with poorly controlled co-morbid disease, such as diabetes, ischaemic heart disease, lung diseases, which cannot be significantly pre-optimized prior to surgery, increasing the chances of peri- and post-operative complications. Studies in cohorts of elective patients undergoing major elective surgery have demonstrated similar finding to our current study [9,10]. These studies suggest that elective patients who develop PPCs have increased length of stay and an increased 30-day mortality [11,12]. Our study supports these findings; however it demonstrates that its incidence is much higher and that outcomes in the longer term (through to 1-year) are much worse. Interestingly our study showed that PPCs were one of the major sources of morbidity, with surgical site infections and acute myocardial ischaemia being infrequently reported. PPCs are a composite definition, with the validated Melbourne Group Score designed to select the clinically significant infection and atelectasis, which arguably are the most serious and often lead to acute lung injury (ALI) and ARDS. The development of nosocomial pneumonia and infections has been shown in several studies to increase length of stay in CCU and also in-hospital, however the precise reasons why longer-term outcomes are poorer is uncertain. It has been suggested that episodes of infection/sepsis cause prolonged immune dysfunction placing survivors of infection/sepsis at higher risk of subsequent infections following discharge from hospital [13]. This may explain the increased rates of emergency re-admissions and later mortality in these patients. PPCs following emergency abdominal surgery have been poorly evaluated, with many studies and trials concentrating on elective surgical populations, where significant risk-factors for PPCs (e.g. smoking and respiratory disease) can be potentially modified [9,10]. The high incidence of PPCs in the high-risk cohort suggests that potential therapies should be targeted at them to attempt to modify their risks of pulmonary complications and that by doing so may improve their longer-term outcomes. Peri-operative ventilation strategies to modify PPCs have been investigated. The landmark IMPROVE trial investigated the use of lung protective ventilation using positive end-expiratory pressure (PEEP) and low tidal volumes and showed significantly reduced incidence of both pulmonary and non-pulmonary infection [14]. Whilst the PROVILHO study investigated the use of high versus low PEEP and demonstrated no difference, but importantly did suggest that high PEEP strategies were associated with increased cardiovascular compromise [15]. Both these studies have potentially important implications in emergency abdominal surgery, however they only recruited patients undergoing major abdominal surgery. The use of protective ventilation in emergency surgery would seem intuitive and supported by evidence in ventilated critically ill patients without ALI/ARDS. Indeed, a prospective observational study of ventilation practices did demonstrate that anaesthetists adopted a more protective strategy in this cohort of patients [16]. Post-operative interventions have also been evaluated, with the recently completely OPERA trial, investigated the use of high-flow nasal oxygen in patients undergoing major abdominal surgery, but found no difference in oxygenation 4 hours post-operatively (primary outcome), nor in any of their clinical secondary outcomes, which included PPCs and LOS [17]. This study, however recruited very few emergency surgical patients. The retrospective nature of this study clearly has clear limits, with perhaps the incidence of PPCs begin over-estimated and with the inability to account for confounding factors. Additionally, due to the retrospective review of EPR and collected data some important factors that may contribute to PPCs were not collected. For example, the smoking status of patients was not collected, nor were individual co-morbidities that may account for some of the differences seen between the high-risk cohorts. The P-POSSUM score does adjust the score dependent on cardiac and respiratory disease, but the classification is broad and dependent on reliable documentation. However, the ASA scores between the groups were not different, suggesting that all patients were subjectively risk assessed appropriately for their pre-existing disease.
List of abbreviations:
United Kingdom – U.K
Length of stay - LOS
National Emergency Laparotomy Audit – NELA
American Society of Anaesthesia - ASA
Portsmouth- Physiological and Operative Severity Score for the enumeration of Mortality and morbidity – PPOSSUM
Post-operative pulmonary complications – PPCs
National Health Service - NHS
Acute respiratory distress syndrome – ARDS
Electronic patient records - EPR
Melbourne Group Score – MGS
Inter-quartile ranges - IQR
Critical Care unit – CCU
Length of Stay – LOS
Acute Lung Injury – ALI
Positive end-expiratory pressure – PEEP
Declarations
Ethics approval and consent to participate
The study did not need ethical approval or research registration. This was confirmed by the online National Research Ethics Survey decision tool completed by the research and development departments at the University of Birmingham.
Consent for publication
Not applicable
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Competing interests
The authors declare that they have no competing interests.
Funding
Not applicable
Author’s contributions
SS helped collect the data and helped write the manuscript. JP oversaw the collection of data, analysed and wrote the manuscript. All authors read and approved the final manuscript.
Acknowledgements
Not applicable
Author’s information
Nothing further to add.
References
- Barrow E, Anderson ID, Varley S, et al. Current UK practice in emergency laparotomy. Annals of the Royal College of Surgeons of England 95 (2013): 599-603.
- Bhangu A, Fitzgerald JE, Fergusson S, et al. Determining universal processes related to best outcome in emergency abdominal surgery: a multicentre, international, prospective cohort study. BMJ Open 4 (2014): e006239.
- Team Np. First patient report of the National Emergency Laparotomy Audit. London (2015).
- Denu ZA, Yasin MO, Melekie TB, et al. Postoperative Pulmonary Complications and Associated Factors among Surgical Patients. J Anesth Clin Res 6 (2015): 554.
- Serejo LG, da Silva-Junior FP, Bastos JP, et al. Risk factors for pulmonary complications after emergency abdominal surgery. Respir Med 101 (2007): 808-813.
- Council MR. Decision Tool: NHS health research authority (2014).
- Agostini P, Naidu B, Cieslik H, et al. Comparison of recognition tools for postoperative pulmonary complications following thoracotomy. Physiotherapy 97 (2011): 278-283.
- Kelkar KV. Post-operative pulmonary complications after non-cardiothoracic surgery. Indian J Anaesth 59 (2015): 599-605.
- Haines KJ, Skinner EH, Berney S, et al. Association of postoperative pulmonary complications with delayed mobilisation following major abdominal surgery: an observational cohort study. Physiotherapy 99 (2013): 119-125.
- Scholes RL, Browning L, Sztendur EM, Denehy L. Duration of anaesthesia, type of surgery, respiratory co-morbidity, predicted VO2max and smoking predict postoperative pulmonary complications after upper abdominal surgery: an observational study. Aust J Physiother 55 (2009): 191-198.
- McAlister FA, Bertsch K, Man J, et al. Incidence of and risk factors for pulmonary complications after nonthoracic surgery. Am J Respir Crit Care Med 171 (2005): 514-517.
- Smetana GW, Lawrence VA, Cornell JE. Preoperative pulmonary risk stratification for noncardiothoracic surgery: systematic review for the American College of Physicians. Ann Intern Med 144 (2006): 581-595.
- Wang T, Derhovanessian A, De Cruz S, et al. Subsequent infections in survivors of sepsis: epidemiology and outcomes. J Intensive Care Med 29 (2014): 87-95.
- Futier E, Constantin JM, Paugam-Burtz C, et al. A trial of intraoperative low-tidal-volume ventilation in abdominal surgery. N Engl J Med 369 (2013): 428-437.
- Hemmes SN, Gama de Abreu M, Pelosi P, et al. High versus low positive end-expiratory pressure during general anaesthesia for open abdominal surgery (PROVHILO trial): a multicentre randomised controlled trial. Lancet 384 (2014): 495-503.
- Patel JM, Baker R, Yeung J, et al. Intra-operative adherence to lung-protective ventilation: a prospective observational study. Perioper Med (Lond) 5 (2016): 8-10.
- Futier E, Paugam-Burtz C, Constantin JM, et al. The OPERA trial - comparison of early nasal high flow oxygen therapy with standard care for prevention of postoperative hypoxemia after abdominal surgery: Study protocol for a multicenter randomized controlled trial. Trials 14 (2013): 341-349.
