Pneumocistis jiroveci Pneumonia in an AIDS-presenter Host: Missing the Target in the COVID-19 Epidemic
Article Information
Vergori A1*, Mastrorosa I1, Pinnetti C1, Camici M1, Di Stefano F2, Mastrobattista A3, Vulcano A4, Bartolini B4, Granata G5, Topino S5, Amendola A6, Antinori A1
1HIV/AIDS Unit, National Institute for Infectious Diseases, Lazzaro Spallanzani IRCCS, Rome, Italy
2Radiology Unit, National Institute for Infectious Diseases Lazzaro Spallanzani IRCCS, Rome, Italy
3 Respiratory Infectious Diseases Unit, National Institute for Infectious Diseases Lazzaro Spallanzani IRCCS, Rome, Italy
4Microbiology Unit, National Institute for Infectious Diseases Lazzaro Spallanzani IRCCS, Rome, Italy
5Severe and Immunedepression-Associated Infectious Diseases Unit, National Institute for Infectious Diseases Lazzaro Spallanzani IRCCS, Rome, Italy
6Laboratory of Virology, National Institute for Infectious Diseases, Lazzaro Spallanzani IRCCS, Rome, Italy
*Corresponding Author: Dr. Alessandra Vergori, HIV/AIDS Unit, National Institute for Infectious Diseases L. Spallanzani, IRCCS, Via Portuense, 292-00149 Rome, Italy
Received: 07 August 2020; Accepted: 25 August 2020; Published: 21 September 2020
Citation: Vergori A, Mastrorosa I, Pinnetti C, Camici M, Di Stefano F, Mastrobattista A, Vulcano A, Bartolini B, Granata G, Topino S, Amendola A, Antinori A. Pneumocistis jiroveci Pneumonia in an AIDS-presenter Host: Missing the Target in the COVID-19 Epidemic. Archives of Clinical and Medical Case Reports 4 (2020): 946-951.
View / Download Pdf Share at FacebookAbstract
We report a case of a previously healthy man admitted with the suspicion of a COVID-19 pneumonia during the Italian pandemic. After 9 days the patient was diagnosed with a new HIV-1 infection with an etiologically confirmed Pneumocistis jiroveci pneumonia (PJP). With this description we would like to highlight the similarities of COVID-19 with PJP and that clinicians should consider other causative agents and that HIV testing should always be offered.
Keywords
COVID-19, HIV; Pneumocistis jiroveci; interstitial pneumonia; AIDS-defining disease
COVID-19 articles, HIV articles, Pneumocistis jiroveci articles, interstitial pneumonia articles, AIDS-defining disease articles
COVID-19 articles COVID-19 Research articles COVID-19 review articles COVID-19 PubMed articles COVID-19 PubMed Central articles COVID-19 2023 articles COVID-19 2024 articles COVID-19 Scopus articles COVID-19 impact factor journals COVID-19 Scopus journals COVID-19 PubMed journals COVID-19 medical journals COVID-19 free journals COVID-19 best journals COVID-19 top journals COVID-19 free medical journals COVID-19 famous journals COVID-19 Google Scholar indexed journals HIV articles HIV Research articles HIV review articles HIV PubMed articles HIV PubMed Central articles HIV 2023 articles HIV 2024 articles HIV Scopus articles HIV impact factor journals HIV Scopus journals HIV PubMed journals HIV medical journals HIV free journals HIV best journals HIV top journals HIV free medical journals HIV famous journals HIV Google Scholar indexed journals Pneumocistis jiroveci articles Pneumocistis jiroveci Research articles Pneumocistis jiroveci review articles Pneumocistis jiroveci PubMed articles Pneumocistis jiroveci PubMed Central articles Pneumocistis jiroveci 2023 articles Pneumocistis jiroveci 2024 articles Pneumocistis jiroveci Scopus articles Pneumocistis jiroveci impact factor journals Pneumocistis jiroveci Scopus journals Pneumocistis jiroveci PubMed journals Pneumocistis jiroveci medical journals Pneumocistis jiroveci free journals Pneumocistis jiroveci best journals Pneumocistis jiroveci top journals Pneumocistis jiroveci free medical journals Pneumocistis jiroveci famous journals Pneumocistis jiroveci Google Scholar indexed journals imaging articles imaging Research articles imaging review articles imaging PubMed articles imaging PubMed Central articles imaging 2023 articles imaging 2024 articles imaging Scopus articles imaging impact factor journals imaging Scopus journals imaging PubMed journals imaging medical journals imaging free journals imaging best journals imaging top journals imaging free medical journals imaging famous journals imaging Google Scholar indexed journals Ultrasonography articles Ultrasonography Research articles Ultrasonography review articles Ultrasonography PubMed articles Ultrasonography PubMed Central articles Ultrasonography 2023 articles Ultrasonography 2024 articles Ultrasonography Scopus articles Ultrasonography impact factor journals Ultrasonography Scopus journals Ultrasonography PubMed journals Ultrasonography medical journals Ultrasonography free journals Ultrasonography best journals Ultrasonography top journals Ultrasonography free medical journals Ultrasonography famous journals Ultrasonography Google Scholar indexed journals treatment articles treatment Research articles treatment review articles treatment PubMed articles treatment PubMed Central articles treatment 2023 articles treatment 2024 articles treatment Scopus articles treatment impact factor journals treatment Scopus journals treatment PubMed journals treatment medical journals treatment free journals treatment best journals treatment top journals treatment free medical journals treatment famous journals treatment Google Scholar indexed journals laparoscopy articles laparoscopy Research articles laparoscopy review articles laparoscopy PubMed articles laparoscopy PubMed Central articles laparoscopy 2023 articles laparoscopy 2024 articles laparoscopy Scopus articles laparoscopy impact factor journals laparoscopy Scopus journals laparoscopy PubMed journals laparoscopy medical journals laparoscopy free journals laparoscopy best journals laparoscopy top journals laparoscopy free medical journals laparoscopy famous journals laparoscopy Google Scholar indexed journals surgery articles surgery Research articles surgery review articles surgery PubMed articles surgery PubMed Central articles surgery 2023 articles surgery 2024 articles surgery Scopus articles surgery impact factor journals surgery Scopus journals surgery PubMed journals surgery medical journals surgery free journals surgery best journals surgery top journals surgery free medical journals surgery famous journals surgery Google Scholar indexed journals interstitial pneumonia articles interstitial pneumonia Research articles interstitial pneumonia review articles interstitial pneumonia PubMed articles interstitial pneumonia PubMed Central articles interstitial pneumonia 2023 articles interstitial pneumonia 2024 articles interstitial pneumonia Scopus articles interstitial pneumonia impact factor journals interstitial pneumonia Scopus journals interstitial pneumonia PubMed journals interstitial pneumonia medical journals interstitial pneumonia free journals interstitial pneumonia best journals interstitial pneumonia top journals interstitial pneumonia free medical journals interstitial pneumonia famous journals interstitial pneumonia Google Scholar indexed journals AIDS-defining disease articles AIDS-defining disease Research articles AIDS-defining disease review articles AIDS-defining disease PubMed articles AIDS-defining disease PubMed Central articles AIDS-defining disease 2023 articles AIDS-defining disease 2024 articles AIDS-defining disease Scopus articles AIDS-defining disease impact factor journals AIDS-defining disease Scopus journals AIDS-defining disease PubMed journals AIDS-defining disease medical journals AIDS-defining disease free journals AIDS-defining disease best journals AIDS-defining disease top journals AIDS-defining disease free medical journals AIDS-defining disease famous journals AIDS-defining disease Google Scholar indexed journals
Article Details
1. Introduction
Since 9 March, 2020 the World Health Organization has declared Coronavirus Disease 2019 (COVID-19), caused by SARS-CoV-2, a global pandemic with relevant health public and clinicians concerns [1] leading to potential misdiagnoses. For instance, it might be difficult to distinguish COVID-19 pneumonia from other viral and bacterial etiologies because of overlapping radiological and clinical features.
2. Case Report
We describe a case of a previously healthy man admitted to the emergency department after 5 days of fever, cough and dyspnea. On examination, he had tachypnea, tachycardia, normal blood pressure and the oxygen saturation was 96% while breathing ambient air at rest. On auscultation breath sounds were normal over the all lung areas, slightly decreased at the right basal segment. A chest high-resolution computed tomography (HRCT) scan (images not available) revealed multiple ground glass opacities (GGOs), bilateral, partially consolidated with interlobular septa thickness and with a tendency to spare the basal segments of the lungs. Laboratory test results and arterial blood gases are shown in Table 1.
|
Laboratory Data |
||||
|
Variable |
Reference Range |
Emergency Department |
COVID-Hospital |
|
|
Day 1 |
Day 4* |
Day 39* |
||
|
Hemoglobin (g/dl) |
13.5-17.5 |
9.9 |
9.2 |
11.2 |
|
Hematocrit (%) |
41.0-53.0 |
30.7 |
29.1 |
35.5 |
|
White-cell count (per mm3) |
4500-11000 |
4.06 |
6070 |
5860 |
|
Differential count (%) |
||||
|
Neutrophils |
40-70 |
60.1 |
85.7 |
66.9 |
|
Lymphocytes |
22-44 |
33.7 |
8.2 |
21.5 |
|
Monocytes |
04-Nov |
5.2 |
6.1 |
10.9 |
|
Basophils |
0-3 |
0.2 |
0 |
0.7 |
|
Platelet count (per mm3) |
150000-400000 |
171000 |
192000 |
453000 |
|
C Reactive protein (mg/dl) |
<1 |
34.5 |
0.72 |
0.25 |
|
Activated partial-thromboplastin time (aPTT, sec) |
22.0-35.0 |
29.2 |
26 |
23.5 |
|
International normalized ratio |
0.80-1.20 |
1.14 |
1.07 |
0.93 |
|
D-dimer (ng/ml) |
<500 |
319 |
317 |
250 |
|
Sodium |
136-145 |
138 |
140 |
137 |
|
Potassium |
3.50-5.10 |
4.3 |
3.7 |
3.6 |
|
Creatinine (mg/dl) |
0.6-1.3 |
0.8 |
0.65 |
0.61 |
|
Urea nitrogen (mg/dl) |
20-50 |
20 |
24 |
27 |
|
Glucose (mg/dl) |
70-110 |
73 |
67 |
43 |
|
Ferritin (ng/ml) |
20-300 |
- |
1179 |
- |
|
Lactate dehydrogenase (U/L) |
120-246 |
497 |
322 |
197 |
|
Aspartate aminotransferase (U/L) |
May-40 |
51 |
26 |
14 |
|
Alanine aminotransferase (U/L) |
May-40 |
25 |
24 |
73 |
|
Fraction of inspired oxygen |
21% |
35% |
21% |
|
|
pH |
7.48 |
7.45 |
7.48 |
|
|
Partial pressure of oxygen (mmHg) |
67 |
141 |
100 |
|
|
Partial pressure of carbon dioxide (mmHg) |
35 |
35 |
43 |
|
|
Oxygen saturation (%) |
96% |
100% |
99% |
|
|
PaO2/FiO2 (mmHg) |
319 |
402 |
595 |
|
*Day 4: admission at COVID hospital; day 39: weaning from oxygen therapy
Table 1: Laboratoristic and blood gases values.
The patient was referred to our institution after 3 days with the clinical and radiological suspicion of COVID-19 pneumonia. SARS-CoV-2 RNA was not detected by real-time PCR (RT-PCR) of two nasopharyngeal swabs. Investigations for other respiratory pathogens were also negative. Blood was tested for Human Immunodeficiency Virus (HIV), as per routine care, which came back reactive. Given the overall picture, a presumptive diagnosis of Pneumocistis jiroveci pneumonia (PJP) was made and promptly, a specific therapy with cotrimoxazole double strength was initiated at therapeutic dosage (Trimetoprim 15 mg/kg/die IV divided q6h) plus tapering prednisone IV for 21 days. No allergic reactions were evident. The patient agreed for bronchoscopy; bronchial washings were taken from the lower lobes bilaterally: Pneumocistis jiroveci etiology was confirmed by RT-PCR, acid fast bacilli smear, PCR for Mycobacterium tuberculosis, bacterial culture and RT-PCR for SARS-CoV-2 were negative, and cytology ruled out malignancy. Moreover, ganciclovir was started as for disseminated CMV disease (sero-positivity of anti-CMV IgG, CMV DNA 270390 IU/mL, CMV antigen as 29 positive cells). Anti-Toxoplasma gondii IgG, Quantiferon test and Cryptococcus neoformans antigen resulted negative, HHV-8 DNA was undetectable. HIV-RNA was 1.454.246 copies/ml, CD4 count 19/mm3 (2,5 %), CD8 515/mm3 (65%) and CD4/CD8 ratio 0,04.
On day 6 after admission antiretroviral therapy with Bictegravir/Emtricitabine/Tenofovir alafenamide was initiated, it was well tolerated and the chest HRCT performed after 21 days of treatment showed a clear improvement (Figure 1a). On day 30 from the start of symptoms, the patient presented high fever with a progressive deterioration of respiratory function, requiring non-invasive mechanical ventilation. A chest HRCT scan revealed a worsening of GGOs which appeared much more diffuse (Figure 1b) compared with the previous HRCT exam (Figure 1a). The patient underwent a new bronchoscopy showing still the presence of Pneumocistis jiroveci by means RT-PCR, ruling out an unmasked TB and, again, SARS-CoV-2 infection. Serology testing for SARS-CoV-2 was negative. Viro-immunological reassessment showed HIV RNA 640 cps/ml with CD4 count 14/mm3 (4%). We considered the clinical and radiological worsening as a treatment failure and a second-line salvage treatment with Clindamycin IV and Primaquine per os was started plus high doses of prednisone. Rapidly, we observed an improvement of clinical conditions with resolution of fever and dyspnea and weaning from oxygen therapy.
PJP is a main issue in HIV immunocompromised hosts that exposes patients to high mortality rates, especially when the diagnosis is delayed. Since microbiological confirmation of PJP is difficult to obtain and not instantaneous, the diagnosis is often presumptive based on clinical, laboratoristic and radiological suspicion. PJP is a potential differential diagnosis for COVID-19 pneumonia, but in the context of this pandemic, it chances being missed, especially in case of unknown HIV infection. Peculiar radiological pattern of COVID-19 pneumonia have been already demonstrated [2-9] and radiologists must be aware that PJP at HRCT is a multifaceted process, with a variety of findings, along with a broad spectrum of infectious (e.g., viral, fungal, bacterial pneumonias) and non-infectious (e.g., pulmonary oedema, diffuse alveolar haemorrhage, and drug toxicity) differential diagnoses [10]. Nevertheless, the GGOs observed in the context of PJP might have a diffuse symmetric predominant distribution in the perihilar regions and the apices with peripheral sparing [11,13].
Although typical chest HRCT patterns of COVID-19 viral pneumonia include multifocal bilateral peripheral ground-glass areas associated with an interlobular septa thichkness (crazy paving pattern) subsegmental patchy consolidations, mostly subpleural, and predominantly involving lower lung lobes and posterior segments (Figure 1c) [2-9].
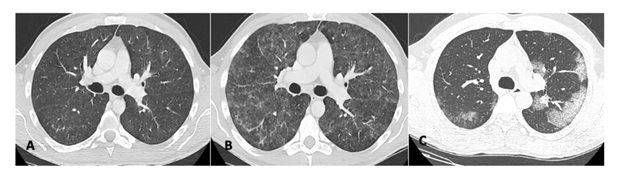
Figure 1A-1C: (1A) CT scan shows bilateral slight GGO areas with periferical sparing; (1B) Same patient as 1A with a severe progression of the interstitial impairment showing diffuse GGO; (1C) Image shows multiple ground-glass opacities with interlobular septal thickening showing a “crazy paving” pattern in the posterior segment of the upper left lobe and in the superior segments of both inferior lobes. The bilateralism of the peripheral lung opacities, without subpleural sparing, are common CT findings of the 2019 novel coronavirus pneumonia.
In the case we describe, not only radiological features mimicked the SARS-CoV-2 etiology, but also hematological findings of both pathologies overlapped. Lymphopenia may be considered as a cardinal laboratory finding of SARS-CoV-2 infection and AIDS-related diseases, with a potential prognostic value, together with longitudinal evaluation of lymphocyte count dynamics and inflammatory indexes, including Lactate dehydrogenase, C Reactive Protein and ferritin [14].
With this case report, we would like to highlight the similarities of COVID-19 with PJP but we are not able to provide clues for the differential diagnosis. When treating a patient with suspected COVID-19 pneumonia, clinicians should consider other causative agents and HIV testing should be always offered.
Funding
Not applicable.
Conflicts of Interest
There is no conflict of interests.
Author’s Statement
All the authors gave a substantial contribution to the manuscript.
References
- Bernheim A, Mei X, Huang M, et al. Chest CT Findings in Coronavirus Disease-19 (COVID-19): Relationship to Duration of Infection. Radiology (2020): 200463.
- Chung M, Bernheim A, Mei X, et al. CT Imaging Features of 2019 Novel Coronavirus (2019-nCoV). Radiology 295 (2020): 202-207.
- Ye Z, Zhang Y, Wang Y, et al. Chest CT manifestations of new coronavirus disease 2019 (COVID-19): a pictorial review. Eur Radiol (2020): doi: 10.1007/s00330-020-06801-0.
- Salehi S, Abedi A, Balakrishnan S, et al. Coronavirus Disease 2019 (COVID-19): A Systematic Review of Imaging Findings in 919 Patients. AJR Am J Roentgenol 14 (2020): 1-7.
- Zhou S, Wang Y, Zhu T, et al. CT Features of Coronavirus Disease 2019 (COVID-19) Pneumonia in 62 Patients in Wuhan, China. AJR Am J Roentgenol 5 (2020): 1-8.
- Albarello F, Pianura E, Di Stefano F, et al. 2019-novel Coronavirus severe adult respiratory distress syndrome in two cases in Italy: An uncommon radiological presentation. Int J Infect Dis 93 (2020): 192-197.
- Zhao D, Yao F, Wang L, et al. A comparative study on the clinical features of COVID-19 pneumonia to other pneumonias. Clin Infect Dis (2020): pii: ciaa247.
- Pan Y, Guan H, Zhou S, et al. Initial CT findings and temporal changes in patients with the novel coronavirus pneumonia (2019-nCoV): a study of 63 patients in Wuhan, China. Eur Radiol (2020): 10.1007/s00330-020-06731-x.
- Cereser L, Dallorto A, Candoni A, et al. Pneumocystis jirovecii pneumonia at chest High-resolution Computed Tomography (HRCT) in non-HIV immunocompromised patients: Spectrum of findings and mimickers. Eur J Radiol 116 (2019): 116-127.
- Bai HX, Hsieh B, Xiong Z, et al. Performance of radiologists in differentiating COVID-19 from viral pneumonia on chest CT. Radiology (2020).
- Kuhlman JE, Kavuru M, Fishman EK, Siegelman SS. Pneumocystis carinii pneumonia: spectrum of parenchymal CT findings. Radiology 175 (1990): 711-714.
- Zhao D, Yao F, Wang L, et al. A comparative study on the clinical features of COVID-19 pneumonia to other pneumonias. Clin Infect Dis (2020): pii: ciaa247.
- Terpos E, Ntanasis-Stathopoulos I, Elalamy I, et al. Hematological findings and complications of COVID-19. Am J Hematol (2020): 10.1002/ajh.25829.
