Pitfalls in Oncocardiology
Article Information
Tamás Kullmann1*, Nikolett Révész2, Adél Ambrus1, Dóra Füzi1, Tamás Pintér1, Csaba András Dézsi3
1Department of Oncoradiology, Petz Aladár County Teaching Hospital, Gy? r, Hungary
2Department of Pulmonology, Petz Aladár County Teaching Hospital, Gy? r, Hungary
3Department of Cardiology, Petz Aladár County Teaching Hospital, Gy? r, Hungary
*Corresponding Author: Tamás Kullmann, Department of Oncoradiology, Petz Aladár County Teaching Hospital, 9024 Gy? r, Vasvári Pál str. 2-4. Hungary
Received: 24 February 2020; Accepted: 26 March 2020; Published: 03 April 2020
Citation: Tamás Kullmann, Nikolett Révész, Adél Ambrus, Dóra Füzi, Tamás Pintér, Csaba András Dézsi. Pitfalls in Oncocardiology. Journal of Cancer Science and Clinical Therapeutics 4 (2020): 086-090.
View / Download Pdf Share at FacebookAbstract
Background: Onco-cardiology is a developing interdisciplinary field aiming to help oncologists to cope with the cardiovascular complications and comorbidities of patients followed for malignancies. Side effects of cytotoxic chemotherapies and targeted treatments are put into focus.
Methods: We selected from our database the most frequent cardiovascular complication and three cases that we found especially relevant from a clinical point of view.
Results: The establishment of the diagnosis of diastolic heart failure on a clinical basis is pointed out. The management of aortic valvulopathy, radiogenic myocarditis and a drug-induced conduction disorder is discussed.
Conclusions: The sensitisation of the oncologists to the evaluation of the cardiac status of their patients by their own is emphasised. Diastolic heart failure should be considered for cancer patients developing dyspnoea. The replacement of stenotic aortic valve should be considered for cancer patients with favourable prognosis.
Keywords
<p>Oncocardiology; Aortic Stenosis; Myocarditis; Anthracycline; Vinorelbine; Cardiac Arrest</p>
Oncocardiology articles, Aortic Stenosis articles, Myocarditis articles, Anthracycline articles, Vinorelbine articles, Cardiac Arrest articles
Oncocardiology articles Oncocardiology Research articles Oncocardiology review articles Oncocardiology PubMed articles Oncocardiology PubMed Central articles Oncocardiology 2023 articles Oncocardiology 2024 articles Oncocardiology Scopus articles Oncocardiology impact factor journals Oncocardiology Scopus journals Oncocardiology PubMed journals Oncocardiology medical journals Oncocardiology free journals Oncocardiology best journals Oncocardiology top journals Oncocardiology free medical journals Oncocardiology famous journals Oncocardiology Google Scholar indexed journals Aortic Stenosis articles Aortic Stenosis Research articles Aortic Stenosis review articles Aortic Stenosis PubMed articles Aortic Stenosis PubMed Central articles Aortic Stenosis 2023 articles Aortic Stenosis 2024 articles Aortic Stenosis Scopus articles Aortic Stenosis impact factor journals Aortic Stenosis Scopus journals Aortic Stenosis PubMed journals Aortic Stenosis medical journals Aortic Stenosis free journals Aortic Stenosis best journals Aortic Stenosis top journals Aortic Stenosis free medical journals Aortic Stenosis famous journals Aortic Stenosis Google Scholar indexed journals Myocarditis articles Myocarditis Research articles Myocarditis review articles Myocarditis PubMed articles Myocarditis PubMed Central articles Myocarditis 2023 articles Myocarditis 2024 articles Myocarditis Scopus articles Myocarditis impact factor journals Myocarditis Scopus journals Myocarditis PubMed journals Myocarditis medical journals Myocarditis free journals Myocarditis best journals Myocarditis top journals Myocarditis free medical journals Myocarditis famous journals Myocarditis Google Scholar indexed journals Anthracycline articles Anthracycline Research articles Anthracycline review articles Anthracycline PubMed articles Anthracycline PubMed Central articles Anthracycline 2023 articles Anthracycline 2024 articles Anthracycline Scopus articles Anthracycline impact factor journals Anthracycline Scopus journals Anthracycline PubMed journals Anthracycline medical journals Anthracycline free journals Anthracycline best journals Anthracycline top journals Anthracycline free medical journals Anthracycline famous journals Anthracycline Google Scholar indexed journals Vinorelbine articles Vinorelbine Research articles Vinorelbine review articles Vinorelbine PubMed articles Vinorelbine PubMed Central articles Vinorelbine 2023 articles Vinorelbine 2024 articles Vinorelbine Scopus articles Vinorelbine impact factor journals Vinorelbine Scopus journals Vinorelbine PubMed journals Vinorelbine medical journals Vinorelbine free journals Vinorelbine best journals Vinorelbine top journals Vinorelbine free medical journals Vinorelbine famous journals Vinorelbine Google Scholar indexed journals Cardiac Arrest articles Cardiac Arrest Research articles Cardiac Arrest review articles Cardiac Arrest PubMed articles Cardiac Arrest PubMed Central articles Cardiac Arrest 2023 articles Cardiac Arrest 2024 articles Cardiac Arrest Scopus articles Cardiac Arrest impact factor journals Cardiac Arrest Scopus journals Cardiac Arrest PubMed journals Cardiac Arrest medical journals Cardiac Arrest free journals Cardiac Arrest best journals Cardiac Arrest top journals Cardiac Arrest free medical journals Cardiac Arrest famous journals Cardiac Arrest Google Scholar indexed journals vascular malignancies articles vascular malignancies Research articles vascular malignancies review articles vascular malignancies PubMed articles vascular malignancies PubMed Central articles vascular malignancies 2023 articles vascular malignancies 2024 articles vascular malignancies Scopus articles vascular malignancies impact factor journals vascular malignancies Scopus journals vascular malignancies PubMed journals vascular malignancies medical journals vascular malignancies free journals vascular malignancies best journals vascular malignancies top journals vascular malignancies free medical journals vascular malignancies famous journals vascular malignancies Google Scholar indexed journals oncologists articles oncologists Research articles oncologists review articles oncologists PubMed articles oncologists PubMed Central articles oncologists 2023 articles oncologists 2024 articles oncologists Scopus articles oncologists impact factor journals oncologists Scopus journals oncologists PubMed journals oncologists medical journals oncologists free journals oncologists best journals oncologists top journals oncologists free medical journals oncologists famous journals oncologists Google Scholar indexed journals venous thromboembolism articles venous thromboembolism Research articles venous thromboembolism review articles venous thromboembolism PubMed articles venous thromboembolism PubMed Central articles venous thromboembolism 2023 articles venous thromboembolism 2024 articles venous thromboembolism Scopus articles venous thromboembolism impact factor journals venous thromboembolism Scopus journals venous thromboembolism PubMed journals venous thromboembolism medical journals venous thromboembolism free journals venous thromboembolism best journals venous thromboembolism top journals venous thromboembolism free medical journals venous thromboembolism famous journals venous thromboembolism Google Scholar indexed journals cytotoxic chemotherapies articles cytotoxic chemotherapies Research articles cytotoxic chemotherapies review articles cytotoxic chemotherapies PubMed articles cytotoxic chemotherapies PubMed Central articles cytotoxic chemotherapies 2023 articles cytotoxic chemotherapies 2024 articles cytotoxic chemotherapies Scopus articles cytotoxic chemotherapies impact factor journals cytotoxic chemotherapies Scopus journals cytotoxic chemotherapies PubMed journals cytotoxic chemotherapies medical journals cytotoxic chemotherapies free journals cytotoxic chemotherapies best journals cytotoxic chemotherapies top journals cytotoxic chemotherapies free medical journals cytotoxic chemotherapies famous journals cytotoxic chemotherapies Google Scholar indexed journals
Article Details
1. Introduction
Cardiovascular events and malignancies are leading causes of death worldwide. Smoking and obesity are common risk factors for both morbidities. Nevertheless, cardiac and vascular malignancies as well as losing a cancer patient of acute coronary syndrome or stroke happen rarely. Onco-cardiology is an interdisciplinary field helping oncologists to cope with cardiovascular complications, such as hypertension, coronary artery disease, arrhythmias, valvular heart disease, heart failure and venous thromboembolism [1]. According to a recent publication, taking into account the above conditions excepted hypertension, atrial fibrillation was the highest prevalent cardiovascular disease in cancer patients (4% in men and 1% in women) and the prevalence of all cardiovascular diseases increased progressively with age (12% in men and 7.5% in women over the age of 80) [2]. Cardiac complications or comorbidities may sometimes be life threatening. However, the possibility that a cancer patient be lost of another cause than his malignancy is not sufficiently taken into account. This paper reports a common and three rare situations when vital prognosis of cancer patients can be engaged by cardiac comorbidities or complications, including diastolic heart failure, aortic valvulopathy, radiogenic myocarditis, and drug-induced conduction disorder.
2. Diastolic Heart Failure
Although shortness of breath is one of the leading complications of cancer patients, there are no studies to systematically investigate the epidemiology and the impact of dyspnoea on the outcome [3]. The potential causes of dyspnoea are summarised in Table 1. The most frequent cause of dyspnoea is left ventricular failure. Hence, iatrogenic hyperhydration and parenteral nutrition may aggravate subclinical cardiac failure. However, the evaluation of the diastolic function by echocardiography is problematic. The ejection fraction being in the correct range does not rule out the possibility of diastolic heart failure.
|
Cardiovascular |
|
Left ventricular heart failure |
|
Pulmonary embolism |
|
Tumoral compression of the pulmonary artery |
|
Respiratory |
|
Pneumonia |
|
Pleural effusion |
|
Atelectasis |
|
Carcinomatous lymphangitis |
|
Multiple pulmonary metastases |
|
Laryngeal occlusion |
|
Haematological |
|
Anaemia |
|
Psychological |
|
Anxiety |
Table 1: Causes of shortness of breath in patients followed for a malignancy.
Indeed, up to the half of all heart failures may be of diastolic origin [4]. These patients typically develop dyspnoea during hospitalisation still physicians may fail to consider the prescribed treatment as a source of their symptoms. The presence of orthopnoea is an important anamnestic element of orientation. The favourable response to diuretic treatment or to the decrease of intravenous volume administration may confirm the hypothesis and sometimes even be lifesaving. Since the cumulative limits of 450 mg for adriamycine and 900 mg for epirubicine have been respected, chemotherapy induced systolic heart failure has had less clinical impact [5]. Docetaxel and trastuzmab induced systolic cardiac failure is usually reversible [6] (Table 2).
|
Drug |
Cardiovascular side effect |
|
anthracyclines |
heart failure +++ |
|
docetaxel |
heart failure ++ |
|
trastuzumab |
heart failure + |
|
5-fluoro-uracil |
coronary spasm |
|
LHRH agonists |
arrhytmia |
|
bevacizumab |
hypertension |
|
sunitinib |
hypertension |
|
axitinib |
hypertension |
|
pazopanib |
hypertension |
|
sorafenib |
hypertension |
Table 2: The most frequent cardiovascular toxicities of anticancer agents.
3. Valvulopathy
A 70-year-old male patient was treated with adjuvant chemotherapy, following resection of a non-metastatic sigmoid colic cancer (adenocarcinoma, grade 1, 0N+/3N). He had a history of type 2 diabetes, hypertension, ischaemic heart disease, CABG intervention, aortic stenosis with a systolic gradient of 20 mmHg, dominant hemispheric TIA and controlateral carotid endarterectomy. A 4/6 ejection murmur was detected on the initial physical examination. The patient did not report any chest pain or dyspnoea. Before the 11th cycle of chemotherapy he had a loss of consciousness upon an effort at home. Control echocardiography showed a systolic gradient of 80 mmHg. Aortic valve replacement was decided and a biologic valve was implanted 16 months after the removal of the colic tumour. The patient is symptom free 3 years after the cardiac surgery. The control examinations including colonoscopy and CT scan did not show any sign of recurrence. Aortic stenosis is the clinically most important valvulopathy. In case it becomes symptomatic or the systolic gradient reaches 80 mmHg its replacement may be indicated even in case of comorbidities. According to a survey a quarter of metastatic cancer patients having severe aortic stenosis were lost because of cardiac complications and not the progression of their malignancy [7]. On the other hand, the presence of a cancer does not raise the risk of valve replacement as compared to patients without malignant disease [8]. For our patient it took several months until the decision was finally done. His favourable cancer-free prognosis was taken into account. The choice of a biologic valve allowing the skipping of anticoagulant treatment would guarantee more safety even in case of local recurrence.
4. Myocarditis
A 55-year-old male patient was treated by palliative chemotherapy for right sided central small-cell lung cancer. The treatment was completed by radiotherapy. He had a history of myocardial infarction and coronary stent implantation. Constricting retrosternal pain occurred after the delivery of 24 Gy. The ECG showed elevated ST segments in the infero-lateral regions (Figure 1). Emergency echocardiography did not show pericardial effusion, coronarography did not detect any significant stenosis. The diagnosis of radiogenic myocarditis was retained. The patient’s complaints and ECG alterations disappeared after stopping radiotherapy. He was lost 6 months later for cerebral progression of the pulmonary malignancy. Radiogenic myocarditis was a more frequent complication of radiotherapy before the era of conformational radiotherapy. We retrospectively verified the planning of our patient and less than 20% of the heart was exposed to a maximal dose of 28 Gy, nevertheless the infero-lateral region received a relatively higher dose. This planning was prepared during the learning period after the installation of a conformational linear accelerator at our department.

Figure 1: ECG showing elevation of the ST segments in non-related derivations, compatible with myocarditis.
5. Atrioventricular Block
A 64-year-old female patient was diagnosed thirteen months earlier with cT4N1M0, hormone sensitive left sided mammal carcinoma (CDI, ER+, PR+, HER2-, Mib1:10%). She progressed after 12 months of letrozole and immediately after the first injection of fulvestrant. She refused the proposed intravenous chemotherapy. Due to the local extension of the disease the realisation of a hygienic mastectomy was not possible. Oral chemotherapy by vinorelbine was offered and finally accepted by the patient. An asymptomatic bradycardia with a ventricular rhythm around 40/min was noticed in the days following introduction of vinorelbine by blood pressure auto-measuring. An ECG was realised before the 4th weekly dose and showed 3rd degree atrio-ventricular block (Figure 2). The patient was authorised to take the 4th dose of vinorelbine. The next morning she had a cardiac arrest at home. Drug induced conduction disorder has not yet been described with vinorelbine. The stopping of the β-antagonist taken for years proposed by the cardiology consultation did not prevent the fatal outcome.
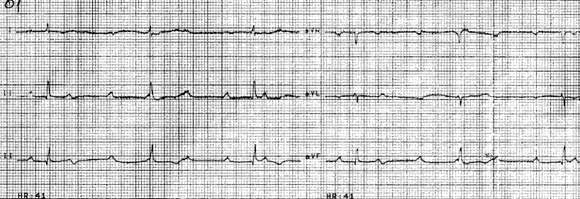
Figure 2: ECG showing 3rd degree atrio-ventricular block.
6. Conclusions
The sensitisation of the oncologists to the evaluation of the cardiac status of their patients by their own is emphasised. Diastolic heart failure should be considered for cancer patients developing dyspnoea. The replacement of stenotic aortic valve should be considered for cancer patients with favourable prognosis.
Conflict of Interest
The authors declare having no conflict of interest in connection with the publication of this paper.
References
- Totzeck M, Schuler M, Stuschke M, et al. Cardio-oncology - strategies for management of cancer-therapy related cardiovascular disease. Int J Cardiol 280 (2019): 163-175.
- Okura Y, Takayama T, Ozaki K, et al. Burden of cardiovascular disease in Japanese cancer patients and survivors: a single cancer-center study in Niigata City. Int J Clin Oncol 24 (2019): 196-210.
- Meriggi F. Dyspnea in Cancer Patients: A Well-Known and Neglected Symptom. Rev Recent Clin Trials 13 (2018): 84-88.
- Røe ÅT, Sjaastad I, Louch WE. Heart failure with preserved ejection fraction. Tidsskr Nor Laegeforen 137 (2017).
- Trédaniel J. Les médicaments du cancer. Groupe CFI-ZI Petite Montagne Sud, Évry, (2009).
- Fogarassy G, Vathy-Fogarassy Á, Kenessey I, et al. Risk prediction model for long-term heart failure incidence after epirubicin chemotherapy for breast cancer - A real-world data-based, nationwide classification analysis. Int J Cardiol 285 (2019): 47-52.
- Okura Y, Ishigaki S, Sakakibara S, et al. Prognosis of Cancer Patients with Aortic Stenosis Under Optimal Cancer Therapies and Conservative Cardiac Treatments. Int Heart J 59 (2018): 750-758.
- Mangner N, Woitek FJ, Haussig S, et al. Impact of active cancer disease on the outcome of patients undergoing transcatheter aortic valve replacement. J Interv Cardiol 31 (2018): 188-196.
