Pharmacological Management of Acute Sleep Disorders During the First 48 hours of the Postoperative Period. A Narrative Review
Article Information
Jairo R Moyano A*, Jairo Urrego, Laura Camargo
Anesthesia Department, Pain Service, University Hospital Fundación Santa Fe de Bogotá, Bogotá, Colombia
*Corresponding Author: Jairo R Moyano A, MD, PhD, Anesthesia Department, Pain Service, University Hospital Fundación Santa Fe de Bogotá, Avenida 9 # 116-20 office 728, Postal code 110111, Bogotá, Colombia
Received: 16 August 2020; Accepted: 05 September 2020; Published: 11 September 2020
Citation: Jairo R Moyano A, Jairo Urrego, Laura Camargo. Pharmacological Management of Acute Sleep Disorders During the First 48 hours of the Postoperative Period. A Narrative Review. Journal of Pharmacy and Pharmacology Research 4 (2020): 67-78.
View / Download Pdf Share at FacebookAbstract
Abstract
Introduction: The positive effects of restorative sleep must be carefully considered during the early postoperative period. The literature on the treatment of acute sleep disorders taking place during the postoperative period is scarce. Most pharmacological therapies are based on the administration of benzodiazepines; however, a personalized approach is strongly recommended, due to their side effects. The objective of this narrative review was to evaluate rational pharmacological therapies for the management of acute sleep disorders during the first 48 hours of the postoperative period in patients undergoing scheduled surgery procedures.
Methods: A narrative review was conducted in the Embase, PubMed, and Cochrane databases. Only controlled randomized trials and systematic reviews were considered for inclusion.
Outcome: The primary outcome was the improvement of sleep patterns after pharmacological treatments for acute sleep disorders, its administration routes, and its impact on postoperative descents.
Results: The initial search yielded 271 studies, however only 7 met the eligibility criteria. Pharmacological therapies based on the administration of Zolpidem at a dose of 5 milligrams at night, Gabapentin at doses> 900 mg/day, and Dexmedetomidine intravenous infusion at a 0.05 mcg/kg/h dose were reported as being effective for the treatment of these disorders during the early postoperative period.
Conclusions: The oral administration of Zolpidem and Gabapentin and the intravenous administration of Dexmedetomidine are effective for the management of acute sleep disorders in carefully selected postoperative patients. Somehow, due to drug side effects, non-pharmacological management alone or combined with pharmacological therapy should be always considered.
Keywords
Acute Pain; Postoperative Period; Sleep Disorders; Hypnotics and Sedatives; Adrenergic α-Agonists
Acute Pain articles, Postoperative Period articles, Sleep Disorders articles, Hypnotics and Sedatives articles, Adrenergic ?-Agonists articles
Article Details
1.Introduction
Sleep disorders may occur during the postoperative period as a result of old age, surgery, anesthetics, concerns regarding the surgery outcomes, physical and psychological stressors [1-3] (Table 1). Usually, these disorders last for a few days and their symptoms disappear in less than three months, as they are no longer experienced when the stressor is solved or when the patient adapts to the stressor.
Table 1: Drug Induced sleep disorders
|
Drug |
Type |
Mechanism action |
Indication |
|
Metoprolol, Labetalol |
Β blockers |
Suppress endogenous nighttime melatonin secretion. |
Heart failure, hypertension, myocardial infarction, atrial fibrillation, migraine prophylaxis, intra-cerebral hemorrhage |
|
Clonidine |
α-2 adrenoceptor agonist |
Alter the NREM/REM sleep cycle by reducing REM sleep |
Hypertension, pain |
|
Methyldopa |
Central sympathetic agent, false neurotransmitter |
Stimulation of central inhibitory α adrenergic receptors |
Hypertension |
|
Losartan |
Angiotensin II receptor antagonist |
Blocking angiotensin II can raise potassium levels by blocking aldosterone secretion |
Hypertension, nephropathy in type 2 diabetes |
|
Atorvastatin, Simvastatin, Rosuvastatin |
Statin |
Inhibition of the synthesis of isoprene, a product formed in the biosynthesis of cholesterol |
Hypercholestelomia |
|
Sertraline, duloxetine, IMAO |
Antidepressants (SSRIs) |
Activation of serotonergic 5-HT2 receptors and increased noradrenergic and dopaminergic neurotransmission |
Major depressive disorder, generalized anxiety disorder, neuropathic pain, muscle skeletal pain |
|
Prednisone |
Corticosteroids |
Elevated afternoon plasma cortisol levels have been associated with insomnia. |
Allergic conditions, dermatologic diseases, endocrine conditions, hematologic diseases, neoplastic conditions, rheumatologic conditions, pulmonary diseases. |
Despite their relatively short duration, sleep disorders are a serious concern for both, patients and their relatives, and harm patients’ recovery, therefore a therapeutic intervention is needed in specific cases [4–6]. Sometimes, these disorders may last more than a few days and turn into chronic sleep disorder, which may be caused by the development of poor sleep habits during the postoperative period when the patient experiences said disorders. Indeed, a healthy sleep pattern and a healthy sleep cycle are fundamental to achieve psychological and physical well-being, and therefore a proper physiological and emotional functioning. In this regard, some studies have reported that sleep disturbances are associated with disorders that affect people in terms of their memory, mood, metabolic function, and inflammatory response [7].
Sleep-related changes during the early postoperative period include decreased total sleep time and decreased slow-wave sleep, limited REM (Rapid Eye Movement) sleep, and an increased duration of the second stage of non-REM sleep [8]. Also, it has been described that after a surgical procedure, patients frequently report having sleep disturbances and experiencing sleep deprivation in their early postoperative period [9].
There are many factors associated with the occurrence of sleep disorders during the postoperative period; somehow, it has been described that these disorders can be caused by multiple factors, including surgical stress, environmental factors, medical treatments [9-14] and comorbidities such as obesity, hypertension, diabetes, cardiovascular disease, and postoperative pain, the latter being a major risk factor for sleep disorders that acts in a bidirectional way since the administration of opioids for easing the pain also alters the sleep cycle [15,16] Therefore, for the proper management of these disorders during the early postoperative period a careful approach must be done and the effectiveness of the available treatments and their potential side effects must be considered, since sometimes drugs may be effective, but they can cause sedation so that patients are at risk of having respiratory distress, aspiration pneumonitis, and experiencing confusion, falls and delirium [7]. In non-surgical patients, Z-drugs, non-benzodiazepines hypnotic agents, (Zolpidem, Zopiclone, Eszopiclone, Zaleplon) and benzodiazepines have been reported to be effective in the short-term for the treatment of sleep disorders; additionally, it has been described that the off-label use of trazodone, diphenhydramine and gabapentinoids has shown some effectiveness in the management of sleep disorders [17], the use of melatonin has been suggested in a meta-analysis of 205 patients with secondary sleep disorders [18].
Taking the above into account, the objective of this literature review is to provide a comprehensive description of the several pharmacological options that can be used for the pharmacological management of acute sleep disorders taking place within 48 hours after surgery in hospitalized patients. It is worth noting than in the present study, acute sleep disorders are defined as those conditions that make patients in their postoperative period to experience difficulties for initiating or maintaining sleep, insufficient sleep duration, and quality, and early morning awakening, and in which pharmacological management should be considered.
2. Methods
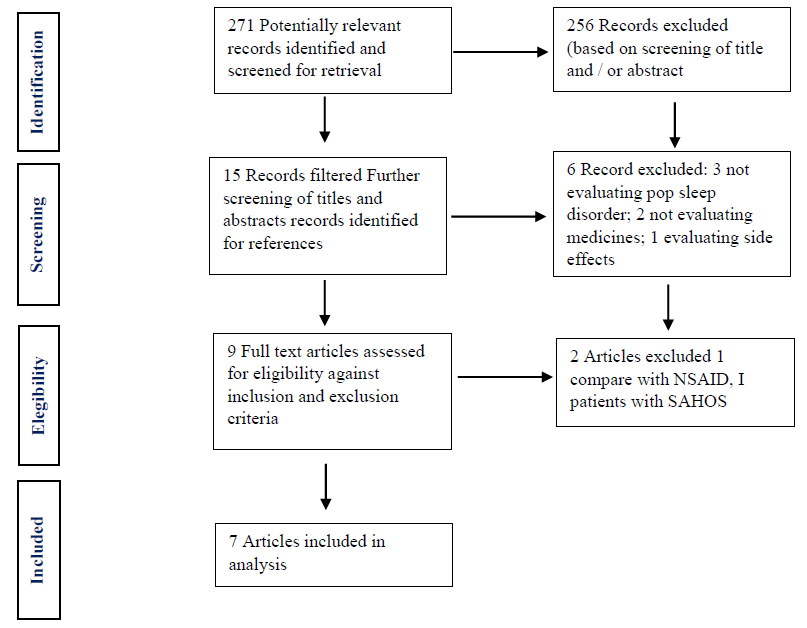
This is a narrative review. A literature search was conducted in the PubMed, EMBASE and COCHRANE databases using the following search terms and combinations: [“insomnia” OR “sleep disturbance” OR “sleep initiation”] AND [“maintenance disorders” OR “sleep deprivation” OR “sleep anxiety”] AND [“zolpidem” OR “eszopiclone” OR “zopiclone” OR “trazodone” OR “hydroxyzine” OR “diphenhydramine” OR “antihistamine” OR “amitriptyline” OR “lorazepam” OR “triazolam” OR “doxepin” OR “mirtazapine” OR “suvorexant” OR “ramelteon” OR “melatonin” OR “clozapine” OR “alprazolam” OR “gabapentin” OR “pregabalin” OR “escitalopram” OR “venlafaxine” OR “duloxetine”] AND [“postoperative” OR “postoperative period” OR “post-anesthesia” OR “post-anesthesia care” OR “postanesthetic” OR “post-surgery” OR “postoperative care” OR “postoperative pain” OR “postoperative sleep”] AND [“inpatient” or “hospital patient”]. Then, a manual search was carried out in gray literature sources (figure 1).
2.1 Inclusion Criteria
Randomized and controlled clinical trials conducted in postoperative care patients who underwent elective surgery and who were older than 18 years and had a postoperative follow-up ≥ 48 hour. Only studies published in English or Spanish and between 2010 and 2019 were considered for inclusion.
2.3 Exclusion criteria
The following studies were excluded:
- Studies on other types of sleep disorders like hypersomnia, obstructive sleep apnea, chronic insomnia.
- Studies conducted in patients with a history of pharmacological management for insomnia or in patients with sleep disorders caused by other conditions than being in a postoperative period.
- Case-series.
- Studies conducted in pediatric or obstetric patients.
- Case reports. (Table 2)
3. Results
The initial search yielded 271 studies. However, once they were fully reviewed; 7 articles met the inclusion criteria and were included for analysis (Table 2) [9,19–22,24,25].
Table 2: Main characteristics of the studies included in the review.
|
Study |
Population |
Intervention |
Comparison |
Methodology / Instrument |
|
Eloy et al. [19] |
29 patients who underwent orthopedic surgery of the lower limb |
Administration of 400 mg/day of Gabapentin on the day of surgery one day after surgery |
Placebo |
PSQI (7 categories of 0-3) |
|
Lunn et al. [20] |
300 patients who underwent total knee replacement |
Gabapentin was administered to 2 out of 3 groups in different doses: -Group A: 1300 mg/day -Group B: 900 mg/day -Group C: placebo was administered for 6 days after surgery |
Placebo |
Sleep quality was measured according to a subjective numerical scale (0 = no sleep problems at all and 10 = the worst experience regarding sleep) |
|
Spence et al. [21] |
70 patients who underwent shoulder arthroscopy |
Gabapentin was used every 12 hours for 2 days after surgery at doses between 300 and 600 mg/day |
Placebo |
Sleep quality was measured using a Likert scale (over 5 points). Total sleep duration was also measured (in hours) |
|
Gong et al. [22] |
148 patients who underwent total knee replacement |
A 5mg/day Zolpidem vs placebo was administered for 14 days |
Placebo |
Sleep efficiency was assessed during 14 days after surgery by means of polysomnographic studies |
|
Chen et al. [9] |
59 patients who underwent abdominal hysterectomy |
Administration of Dexmedetomidine + Sulfentanil IV 0.05 mcg/kg/h Dexmedetomidine infusion |
Sulfentanil IV |
Sleep efficiency was measured using polysomnography the first 2 nights after surgery |
|
Buvanendran et al. [24] |
240 patients who underwent total knee replacement |
300 mg of Pregabalin was administered before the surgery |
Placebo |
Sleep problems were measured according to a numerical scale (0 = no sleeping problems and 10 = facing the worst sleep problems) |
|
Andersen et al. [25] |
44 aged 18-70 who underwent laparoscopic cholecystectomy |
A 10 mg melatonin IV dose was administered to induce sleep 30 min after surgery |
Placebo |
Sleep quality was measured using the Karolinska scale (KSS, 1 = extremely alert, 9 = extremely asleep) from day 1 to day 3 of the postoperative period. |
Source: Own elaboration.
3.1 Zolpidem
Zolpidem is a GABAA receptor chloride channel agonist that increases GABA inhibitory effects leading to sedation, however, its the structure differs from that of benzodiazepines [26,27]. The study conducted by Gong (2015) [22] examined the effects of sleep quality on early recovery after total knee arthroplasty (n=148) demonstrated that improved sleep quality is beneficial to the patient’s recovery; patients on Zolpidem significantly improved knee pain from postoperative day 7 to 14. This drug is available in immediate-release and extended-release oral tablets, oral spray formulation, and sublingual tablets. Several side effects have been associated with the use of Zolpidem in adults, including headache, dizziness, drowsiness, nausea, diarrhea, myalgias, rebound insomnia, and memory and behavior disorders. Regarding its use for treating insomnia, it has been found that, compared to benzodiazepines, Zolpidem has similar effectiveness and has fewer side effects [28]. Also, Krenk et al. (2014) [29], in another randomized, double-blind study that compared the use of Zolpidem versus placebo in 20 patients (≥ 60 years) who underwent a hip and knee replacement under spinal anesthesia did not find a significant difference between groups following major surgery. Therefore, based on this information, it is possible to consider that the administration of 5mg of Zolpidem the first night of the postoperative period is useful for helping patients with their sleep disorders. Currently, Zolpidem is labeled for the short-term treatment of insomnia characterized by difficulties with sleep initiation, the recommended initial dose is 5 mg at bedtime.
3.2 Gabapentin
Gabapentin is a GABA alkylated derivative that is used in the management of postherpetic neuralgia in adults and as adjunctive therapy in the treatment of partial-onset seizures. Its mechanism of action consists of the direct inhibition of voltage-gated Ca2+ channels by binding to its α2-1 subunit, resulting in the reduction of presynaptic Ca2+ influx and the subsequent release of excitatory neurotransmitters such as glutamate, thus reducing the hyperexcitability of the nociceptive neurons, which decreases the transmission of pain and central sensitization. When Gabapentin is administered during the perioperative period, it reduces the consumption of opioids and their related side effects, as well as postoperative pain intensity. Its most frequent side effects include sedation and dizziness, but peripheral edema has also been described [30,31]. In healthy individuals, Gabapentin has shown to improve sleep by enhancing slow-sleep waves, decreasing early awakening episodes and maintaining REM sleep [32,33], in a study conducted in patients who underwent a total knee replacement, reported that the administration of Gabapentin in 900-1300 mg/day doses during the first two nights after of the postoperative period improved the sleep quality of these patients, Lo et al. [34] have described that the higher the dose, the higher the risk of experiencing sedation and visual disturbances.
Contrary to these findings, Eloy et al. [19], in a study conducted in patients with total hip or knee replacement to assess the effects of Gabapentin on postoperative pain and its effectiveness to improve sleep patterns using the Pittsburg Sleep Quality Index (PSQI), found that it does not produce any relieving effect on pain, nor does it improve sleep patterns [19]. Likewise, according to Spence et al. [21], using Gabapentin in patients who undergo shoulder arthroscopy does not improve their sleep duration or quality when compared to a placebo [21]. Gabapentin effects on sleep disorders have been studied employing polysomnographic studies. For example, in a study conducted in 18 patients with insomnia it was found that a 600mg/day dose showed the best results [18], although in another study up to 900mg/day were required (540mg/day average dose) [35]. However, it should be noted that in this study, Gabapentin was titrated for up to 3 weeks to adjust the appropriate dose, so doses described there may vary.
Based on the findings described above, the use of Gabapentin regularly for the management of sleep disorders during the postoperative period should not be recommended since there is not enough evidence to determine the appropriate dose and the type of surgical procedure in which it may be used.
3.3 Pregabalin
Pregabalin, like Gabapentin, acts through voltage-dependent calcium channels [30], it is indicated for the treatment of painful diabetic peripheral neuropathy, postherpetic neuralgia, partial-onset seizures, fibromyalgia, neuropathic pain associated with spinal cord injury. There is not much information on the use of Pregabalin in patients with sleep disorders. However, based on polysomnographic studies it has been revealed that it affects sleep-maintenance insomnia and has benefits for the management of sleep disorders caused by multiple conditions, including as fibromyalgia, generalized anxiety disorder, neuropathic pain and postherpetic neuralgia [36,37].
Buvanendran et al. [24]., in a randomized, placebo-controlled, double-blind trial of pregabalin 300 mg administered before Total Knee Arthroplasty reported that Pregabalin was effective to achieve a decrease in the frequency of sleep disturbances, in the first postoperative night. The pregabalin patients had highly significant (P< 0.0001) less sleep interference compared with placebo patients.
3.4 Melatonin
Melatonin is an endogenous hormone produced by the pineal gland. The correlation between the nocturnal elevation of melatonin secretion and its increased levels at the beginning of nights is evidence of the role this hormone plays in sleep regulation [38,39]. The use of melatonin for treating sleep disorders is considered a complementary and alternative therapy and is not regulated by the FDA.
The use of melatonin has been described in patients with sleep disorders associated with their circadian rhythm and in elderly patients, but it has also been recommended for the management of acute sleep disorders [39]. Kirksey et al. [40], in a randomized, double-blind pilot study that evaluated the effects of melatonin on postoperative sleep and pain in patients who underwent a total knee arthroplasty, found that, when compared to the use of placebo, melatonin administration did not show a difference in sleep efficiency (p = 0.15) or total sleep time (p=0.067) [36].
Andersen et al. [25] in a randomized, placebo-controlled, double-blinded study in 44 patients who underwent cholecystectomy showed that the administration of a 10mg melatonin dose was ineffective to improve sleep quality during the three first days of the postoperative period. The most widely known side effects of this drug are headache and dizziness, yet a decrease in subjective sleep latency has also been reported. Gögenur et al. [41] described that the administration of 5mg/day melatonin doses in patients who underwent a laparoscopic cholecystectomy did not show any difference in terms of sleep quality improvement when compared to the use of placebos [41]. Therefore, based on these findings, melatonin is not recommended for the management of sleep disorders in postoperative care patients.
3.5 Dexmedetomidine
Dexmedetomidine is a drug with sedative, analgesic, and anxiolytic properties that acts as a highly selective agonist of α-2 adrenergic receptors, without producing effects on the respiratory rate. It has a 1610:1 affinity ratio for α-2 receptors compared to α-1 receptors [42]. Regarding its action mechanism about sleep physiology, when it binds to α-2 adrenergic receptors, the activity of neurons in the locus coeruleus decreases, exerting a function in the initiation and maintenance of sleep by decreasing the adrenergic inputs that promote awakening in the cortex, the basal forebrain, the thalamus, and the hypothalamus. Also, they modulate non-adrenergic neurons in the thalamus and the forebrain to induce sleep [43]. Unlike other sedative agents, dexmedetomidine exerts its sedative effects through an endogenous sleep-promoting pathway and produces an N2 sleep-like state.
The use of Dexmedetomidine in patients put on ventilators at intensive care units helps them maintain their sleep cycle and increases their sleep efficiency. Also, it has been reported that in postoperative care elderly patients who are not on ventilators, the infusion of this drug increases total sleep time [44]. Furthermore, Akeju et al. [43], in a prospective, randomized, and crossover pilot study conducted in 10 patients, compared the effects of Dexmedetomidine and Zolpidem in terms of sleep induction, finding that dexmedetomidine promotes N3 stage sleep in a dose-dependent manner without altering the psychomotor vigilance test scores [43].
Chen et al. [45], evaluated the effects of postoperative dexmedetomidine infusion on sleep quality in 60 patients undergoing abdominal hysterectomy; it was found that the administration of dexmedetomidine infusion plus sufentanil to patients who underwent an abdominal hysterectomy, compared with the administration of sufentanil alone, led to a significant improvement in the efficiency of sleep and fewer of early awakening episodes. Also, these patients showed better pain control. Finally, in a similar study, Qin et al. [36] reported that in patients who underwent partial laryngectomy and were administered Dexmedetomidine and sufentanil had fewer sleep problems during the postoperative period than those who were only administered sufentanil.
4. Discussion
There is limited evidence on the efficacy of pharmacological management of acute sleep disorders in postoperative care patients. In the study by Eloy et al. results indicate that gabapentin does not improve sleep habits in patients after orthopedic surgery. In the study by Lunn et al, sleep quality was better during the first 2 nights after surgery in groups treated with gabapentin vs placebo, but it was a secondary outcome. In the study by Spence et al. in 2011 in shoulder surgery, sleep patterns were similar between gabapentin and placebo groups (300 mg of gabapentin or placebo 1 hour before surgery) [21]. In the study by Gong L et al. [22] it was found that patients taking zolpidem achieved greater improvement in quality of life, and a significant correlation between sleep quality and range of motion was detected. These results demonstrated that improved sleep quality is beneficial to patients’ post-TKA recovery. In the study by Chen et al. [9] postoperative administration of dexmedetomidine significantly improved the subjective sleep quality. In the study by Buvanendran et al. [24] the pregabalin patients had less sleep interference compared with placebo patients while in the hospital. In the study by Anderson et al. [25] no significant differences were found between placebo and intravenous melatonin with respect to sleep quality. Therefore, based on the information reviewed here, non-pharmacological measures such as earplugs and masks [46], as well as complementary measures commonly known as sleep hygiene, should be considered as the first options for the management of these disorders; however, they are time-consuming and sometimes the rapid discharge of these patients does not allow their implementation. Likewise, it is usual that some adult patients without a history of sleep disorder report having poor sleep patterns after undergoing surgery, since acute sleep disorders may be triggered by the stress experienced by them during the preoperative period. Somehow, these disorders are usually a transient situation that disappears after the stressor is gone. Taking this into account, the goal of pharmacologic interventions in postoperative care patients is to minimize the additional psychological and physical stress that sleeplessness produces in them. Also, appropriate treatment of short-term sleep disorders may reduce the risk of developing dysfunctional cognitive and behavioral responses to sleeplessness that could otherwise increase the risk of developing chronic sleep disorders. So, after considering the implementation of non-pharmacological measures, hypnotic drug therapy should be considered for the management of severe sleep disorders interfering with these patients’ daily life and their recovery, somehow hypnotics should only be prescribed for short periods. Several hypnotics have been approved for the treatment of insomnia, including benzodiazepines, and zaleplon, zolpidem, and zopiclone (Z-drugs).
5. Conclusions
Gabapentin at doses greater than 900 mg/day and Zolpidem at a dose of 5 mg at night may have a positive impact on sleep efficacy during the early postoperative period, patients hospitalized at ICUs or with postoperative delirium are suitable candidates for the management of sleep disorders through the intravenous administration of Dexmedetomidine. However, due to the side effects of hypnotics, non-pharmacological methods are highly recommended. More studies are required to establish how to measure sleep quality in postoperative care patients and to determine the most appropriate pharmacological treatment.
References
- Kushikata T. Sleep science in anesthesiology. Journal of Anesthesia 33 (2019): 351-353.
- Su X, Wang DX. Improve postoperative sleep: what can we do?. Current Opinion in Anaesthesiology 31 (2018): 83.
- Long G, Suqin S, Hu Z, et al. Analysis of patients' sleep disorder after total knee arthroplasty-A retrospective study. Journal of Orthopaedic Science: Official Journal of the Japanese Orthopaedic Association 24 (2018): 116-120.
- Gaspar MP, Kane PM, Jacoby SM, et al. Evaluation and management of sleep disorders in the hand surgery patient. The Journal of Hand Surgery 41 (2016): 1019-1026.
- Tobaldini E, Fiorelli EM, Solbiati M, et al. Short sleep duration and cardiometabolic risk: from pathophysiology to clinical evidence. Nature Reviews Cardiology 16 (2019): 213-224.
- Javaheri S, Redline S. Insomnia and risk of cardiovascular disease. Chest 152 (2017): 435-444.
- Hillman DR. Postoperative Sleep Disturbances: Understanding and Emerging Therapies. Advances in Anesthesia 35 (2017): 1-24.
- Mehra R. Sleep apnea and the heart. Cleve Clin J Med 86 (2019): 10-18.
- Chen Z, Tang R, Zhang R, et al. Effects of dexmedetomidine administered for postoperative analgesia on sleep quality in patients undergoing abdominal hysterectomy. Journal of Clinical Anesthesia 36 (2017):118-122.
- Lee A, O'Loughlin E, Roberts LJ. A double-blinded randomized evaluation of alfentanil and morphine vs fentanyl: analgesia and sleep trial (DREAMFAST). British Journal of Anaesthesia 110 (2013): 293-298.
- Riemann D, Baglioni C, Bassetti C, et al. European guideline for the diagnosis and treatment of insomnia. Journal of Sleep Research 26 (2017): 675-700.
- Barichello E, Sawada NO, Sonobe HM, et al. La calidad del sueño en pacientes sometidos a cirugía oncológica. Revista Latino-Americana de Enfermagem 17 (2009): 481-488.
- Miller A, Roth T, Roehrs T, et al. Correlation between sleep disruption on postoperative pain. Otolaryngology--Head and Neck Surgery 152 (2015): 964-968.
- Klemann N, Hansen MV, Gögenur I. Factors affecting post-operative sleep in patients undergoing colorectal surgery–a systematic review. Danish Medical Journal 62 (2015): A5053.
- Chouchou F, Khoury S, Chauny JM, et al. Postoperative sleep disruptions: a potential catalyst of acute pain?. Sleep Medicine Reviews 18 (2014): 273-282.
- Krenk L, Jennum P, Kehlet H. Sleep disturbances after fast-track hip and knee arthroplasty. British Journal of Anaesthesia 109 (2012): 769-775.
- Zamponi GW, Striessnig J, Koschak A, et al. The physiology, pathology, and pharmacology of voltage-gated calcium channels and their future therapeutic potential. Pharmacological Reviews 67 (2015): 821-870.
- Li T, Jiang S, Han M, et al. Exogenous melatonin as a treatment for secondary sleep disorders: A systematic review and meta-analysis. Frontiers in Neuroendocrinology 52 (2019): 22-28.
- Eloy JD, Anthony C, Amin S, et al. Gabapentin does not appear to improve postoperative pain and sleep patterns in patients who concomitantly receive regional anesthesia for lower extremity orthopedic surgery: a randomized control trial. Pain Research and Management 2017 (2017).
- Lunn TH, Husted H, Laursen MB, et al. Analgesic and sedative effects of perioperative gabapentin in total knee arthroplasty: a randomized, double-blind, placebo-controlled dose-finding study. Pain 156 (2015): 2438-2448.
- Spence D, Goff J, Mohan E, et al. Perioperative administration of gabapentin for shoulder arthroscopy: a prospective, randomized, double-blind, placebo-controlled study. AANA Journal 79 (2011).
- Gong L, Wang Z, Fan D. Sleep quality effects recovery after total knee arthroplasty (TKA)—a randomized, double-blind, controlled study. The Journal of Arthroplasty 30 (2015): 1897-1901.
- Lee HY, Li JH, Wu LT, et al. Survey of methadone-drug interactions among patients of methadone maintenance treatment program in Taiwan. Substance Abuse Treatment, Prevention, and Policy 7 (2012): 11.
- Buvanendran A, Kroin JS, Della Valle CJ, et al. Perioperative oral pregabalin reduces chronic pain after total knee arthroplasty: a prospective, randomized, controlled trial. Anesthesia & Analgesia 110 (2010): 199-207.
- Andersen LP, Kücükakin B, Werner MU, et al. Absence of analgesic effect of intravenous melatonin administration during daytime after laparoscopic cholecystectomy: a randomized trial. Journal of Clinical Anesthesia 26 (2014): 545-550.
- MacFarlane J, Morin CM, Montplaisir J. Hypnotics in insomnia: the experience of zolpidem. Clinical Therapeutics 36 (2014): 1676-1701.
- Valente KD, Hasan R, Tavares SM, et al. Lower doses of sublingual Zolpidem are more effective than oral Zolpidem to anticipate sleep onset in healthy volunteers. Sleep Medicine 14 (2013): 20-23.
- Schroeck JL, Ford J, Conway EL, et al. Review of safety and efficacy of sleep medicines in older adults. Clinical Therapeutics 38 (2016): 2340-2372.
- Krenk L, Jennum P, Kehlet H. Postoperative sleep disturbances after zolpidem treatment in fast-track hip and knee replacement. Journal of Clinical Sleep Medicine 10 (2014): 321-326.
- Kumar AH, Habib AS. The role of gabapentinoids in acute and chronic pain after surgery. Current Opinion in Anesthesiology 32 (2019): 629-634.
- Quintero GC. Review about gabapentin misuse, interactions, contraindications and side effects. Journal of Experimental Pharmacology 9 (2017): 13.
- Rosenberg RP, Hull SG, Lankford DA, et al. A randomized, double-blind, single-dose, placebo-controlled, multicenter, polysomnographic study of gabapentin in transient insomnia induced by sleep phase advance. Journal of Clinical Sleep Medicine 10 (2014): 1093-1100.
- Ayala-Guerrero F, Mexicano G, Gutiérrez-Chávez CA, et al. Effect of gabapentin on sleep patterns disturbed by epilepsy. Epilepsy & Behavior 92 (2019): 290-296.
- Lo HS, Yang CM, Lo HG, et al. Treatment effects of gabapentin for primary insomnia. Clinical Neuropharmacology 33 (2010): 84-90.
- Foldvary-Schaefer N, De Leon Sanchez I, Karafa M, et al. Gabapentin increases slow-wave sleep in normal adults. Epilepsia 43 (2002): 1493-1497.
- Qin M, Chen K, Liu T, et al. Dexmedetomidine in combination with sufentanil for postoperative analgesia after partial laryngectomy. BMC Anesthesiology 17 (2017): 66.
- Roth T, Arnold LM, Garcia-Borreguero D, et al. A review of the effects of pregabalin on sleep disturbance across multiple clinical conditions. Sleep Medicine Reviews 18 (2014): 261-271.
- Kim TW, Jeong JH, Hong SC. The impact of sleep and circadian disturbance on hormones and metabolism. International Journal of Endocrinology 2015 (2015).
- Zisapel N. New perspectives on the role of melatonin in human sleep, circadian rhythms and their regulation. British Journal of Pharmacology 175 (2018): 3190-3199.
- Kirksey MA, Yoo D, Danninger T, et al. Impact of melatonin on sleep and pain after total knee arthroplasty under regional anesthesia with sedation: a double-blind, randomized, placebo-controlled pilot study. The Journal of Arthroplasty 30 (2015): 2370-2375.
- Gögenur I, Kücükakin B, Bisgaard T, et al. The effect of melatonin on sleep quality after laparoscopic cholecystectomy: a randomized, placebo-controlled trial. Anesthesia & Analgesia 108 (2009): 1152-1156.
- Yu X, Franks NP, Wisden W. Sleep and sedative states induced by targeting the histamine and noradrenergic systems. Frontiers in Neural Circuits 12 (2018): 04.
- Akeju O, Hobbs LE, Gao L, et al. Dexmedetomidine promotes biomimetic non-rapid eye movement stage 3 sleep in humans: A pilot study. Clinical Neurophysiology 129 (2018): 69-78.
- Lu W, Fu Q, Luo X, et al. Effects of dexmedetomidine on sleep quality of patients after surgery without mechanical ventilation in ICU. Medicine 96 (2017).
- Chen AF, Orozco FR, Austin LS, et al. Prospective evaluation of sleep disturbances after total knee arthroplasty. The Journal of Arthroplasty 31 (2016): 330-332.
- Hu RF, Jiang XY, Chen J, et al. Non-pharmacological interventions for sleep promotion in the intensive care unit. Cochrane Database of Systematic Reviews (2015).