Peroneus Longus Tendon Autograft for Anterior Cruciate Ligament Reconstruction: A Safe and Effective Alternative in Nonathletic Patients
Article Information
Rahaman SK1, Halder RC1, Tayaba T2, Mamun MBA1, Islam MS1, Khan MMR1, Rahman MM3, Hossain GMJ1
1Department of Orthopedics, National Institute of Traumatology and Orthopedic Rehabilitation (NITOR), Dhaka, Bangladesh
2Department of Obstetrics and Gynaecology, Bangabandhu Sheikh Mujib Medical College Hospital (BSMMCH), Faridpur, Bangladesh
3Department of Orthopedic Surgery, Bangabandhu Sheikh Mujib Medical University (BSMMU), Dhaka, Bangladesh
*Corresponding Author: Syed Khaledur Rahaman, Department of Orthopedics, National Institute of Traumatology and Orthopedic Rehabilitation (NITOR), Dhaka, Bangladesh.
Received: 02 March 2023; Accepted: 10 March 2023; Published: 14 March 2023
Citation:
Rahaman SK, Halder RC, Tayaba T, Mamun MBA, Islam MS, Khan MMR, Rahman MM, Hossain GMJ, Kamruzzaman M. Peroneus Longus Tendon Autograft for Anterior Cruciate Ligament Reconstruction: A Safe and Effective Alternative in Nonathletic Patients. Journal of Orthopedics and Sports Medicine. 5 (2023): 133-138.
View / Download Pdf Share at FacebookAbstract
Background: The Anterior Cruciate Ligament (ACL) is one of the most vital parts for sustaining knee joint stability. But, the frequency of ACL injuries is increasing alarmingly. The Peroneus Longus Tendon (PLT) is now considered to be a promising graft which is a safe and efficient alternative to other grafting methods.
Methods: This was a prospective interventional study conducted at a tertiary care orthopaedic teaching hospital, during the period of March, 2019-August, 2022. The sample size for this study was 64. For statistical analysis, SPSS version 20 was used as a statistical tool.
Result: There were 9(14.1%) respondents who were <18 years of age, followed by 22(34.4%) who were aged between 18-20 years, while the remaining 33(51.6%) were aged >20 years. The mean ± SD diameter (mm) was 8.3 ± 0.8, length (mm) was 8.5 ± 0.4, height (cm) was 174.1 ± 8.6, weight (kg) was 76.2 ± 13.2 and BMI was 25.0 ± 3.4. The majority of the patients (50%) were injured 1-3 months prior to the surgery. At the 6-month follow-up period, according to Lachman indicators after the surgery, 59(92.2%) of the respondents were graded 0, and the remaining 5(7.8%) were graded I. At the 12-month follow-up, the majority (93.8%) were graded 0, and 4(6.3%) graded I. At the 18-months follow-up, 59(92.2%) were graded 0 and 5(7.8%) were graded I. At the 6-month follow- up period by KT- 2000 indicators (mm) after the surgery, 57(89.1%) of the respondents were graded 0-2 mm, followed by 7(10.9%) graded 3-5 mm. At 12-months followed up the most 59(92.2%) were graded 0-2 mm and followed by 5(7.8%) graded 3-5 mm at the 18-month followed up, 57(89.1%) graded 0-2 mm, and followed by 7(10.9%) graded 3-5 mm.
Conclusion: Peroneus longus tendon autograft in ACL reconstruction is a safe procedure that has a satisfactory result which was proved by the Lachman’s Test and the IKDC (KT-2000) score. PLT can prove to be an effective alternative autograft for ACL reconstruction.
Keywords
Peroneus Longus Tendon; Autograft, Anterior Cruciate Ligament Reconstruction; Nonathletic Patients
Orthopedic rehabilitation articles Orthopedic rehabilitation Research articles Orthopedic rehabilitation review articles Orthopedic rehabilitation PubMed articles Orthopedic rehabilitation PubMed Central articles Orthopedic rehabilitation 2023 articles Orthopedic rehabilitation 2024 articles Orthopedic rehabilitation Scopus articles Orthopedic rehabilitation impact factor journals Orthopedic rehabilitation Scopus journals Orthopedic rehabilitation PubMed journals Orthopedic rehabilitation medical journals Orthopedic rehabilitation free journals Orthopedic rehabilitation best journals Orthopedic rehabilitation top journals Orthopedic rehabilitation free medical journals Orthopedic rehabilitation famous journals Orthopedic rehabilitation Google Scholar indexed journals Orthopedics articles Orthopedics Research articles Orthopedics review articles Orthopedics PubMed articles Orthopedics PubMed Central articles Orthopedics 2023 articles Orthopedics 2024 articles Orthopedics Scopus articles Orthopedics impact factor journals Orthopedics Scopus journals Orthopedics PubMed journals Orthopedics medical journals Orthopedics free journals Orthopedics best journals Orthopedics top journals Orthopedics free medical journals Orthopedics famous journals Orthopedics Google Scholar indexed journals Traumatology articles Traumatology Research articles Traumatology review articles Traumatology PubMed articles Traumatology PubMed Central articles Traumatology 2023 articles Traumatology 2024 articles Traumatology Scopus articles Traumatology impact factor journals Traumatology Scopus journals Traumatology PubMed journals Traumatology medical journals Traumatology free journals Traumatology best journals Traumatology top journals Traumatology free medical journals Traumatology famous journals Traumatology Google Scholar indexed journals Anterior Cruciate Ligament articles Anterior Cruciate Ligament Research articles Anterior Cruciate Ligament review articles Anterior Cruciate Ligament PubMed articles Anterior Cruciate Ligament PubMed Central articles Anterior Cruciate Ligament 2023 articles Anterior Cruciate Ligament 2024 articles Anterior Cruciate Ligament Scopus articles Anterior Cruciate Ligament impact factor journals Anterior Cruciate Ligament Scopus journals Anterior Cruciate Ligament PubMed journals Anterior Cruciate Ligament medical journals Anterior Cruciate Ligament free journals Anterior Cruciate Ligament best journals Anterior Cruciate Ligament top journals Anterior Cruciate Ligament free medical journals Anterior Cruciate Ligament famous journals Anterior Cruciate Ligament Google Scholar indexed journals Knee joint's stability articles Knee joint's stability Research articles Knee joint's stability review articles Knee joint's stability PubMed articles Knee joint's stability PubMed Central articles Knee joint's stability 2023 articles Knee joint's stability 2024 articles Knee joint's stability Scopus articles Knee joint's stability impact factor journals Knee joint's stability Scopus journals Knee joint's stability PubMed journals Knee joint's stability medical journals Knee joint's stability free journals Knee joint's stability best journals Knee joint's stability top journals Knee joint's stability free medical journals Knee joint's stability famous journals Knee joint's stability Google Scholar indexed journals ACL injuries articles ACL injuries Research articles ACL injuries review articles ACL injuries PubMed articles ACL injuries PubMed Central articles ACL injuries 2023 articles ACL injuries 2024 articles ACL injuries Scopus articles ACL injuries impact factor journals ACL injuries Scopus journals ACL injuries PubMed journals ACL injuries medical journals ACL injuries free journals ACL injuries best journals ACL injuries top journals ACL injuries free medical journals ACL injuries famous journals ACL injuries Google Scholar indexed journals Sports activities articles Sports activities Research articles Sports activities review articles Sports activities PubMed articles Sports activities PubMed Central articles Sports activities 2023 articles Sports activities 2024 articles Sports activities Scopus articles Sports activities impact factor journals Sports activities Scopus journals Sports activities PubMed journals Sports activities medical journals Sports activities free journals Sports activities best journals Sports activities top journals Sports activities free medical journals Sports activities famous journals Sports activities Google Scholar indexed journals Graft type articles Graft type Research articles Graft type review articles Graft type PubMed articles Graft type PubMed Central articles Graft type 2023 articles Graft type 2024 articles Graft type Scopus articles Graft type impact factor journals Graft type Scopus journals Graft type PubMed journals Graft type medical journals Graft type free journals Graft type best journals Graft type top journals Graft type free medical journals Graft type famous journals Graft type Google Scholar indexed journals Initial graft tension articles Initial graft tension Research articles Initial graft tension review articles Initial graft tension PubMed articles Initial graft tension PubMed Central articles Initial graft tension 2023 articles Initial graft tension 2024 articles Initial graft tension Scopus articles Initial graft tension impact factor journals Initial graft tension Scopus journals Initial graft tension PubMed journals Initial graft tension medical journals Initial graft tension free journals Initial graft tension best journals Initial graft tension top journals Initial graft tension free medical journals Initial graft tension famous journals Initial graft tension Google Scholar indexed journals Graft diameter articles Graft diameter Research articles Graft diameter review articles Graft diameter PubMed articles Graft diameter PubMed Central articles Graft diameter 2023 articles Graft diameter 2024 articles Graft diameter Scopus articles Graft diameter impact factor journals Graft diameter Scopus journals Graft diameter PubMed journals Graft diameter medical journals Graft diameter free journals Graft diameter best journals Graft diameter top journals Graft diameter free medical journals Graft diameter famous journals Graft diameter Google Scholar indexed journals Anatomic reconstruction articles Anatomic reconstruction Research articles Anatomic reconstruction review articles Anatomic reconstruction PubMed articles Anatomic reconstruction PubMed Central articles Anatomic reconstruction 2023 articles Anatomic reconstruction 2024 articles Anatomic reconstruction Scopus articles Anatomic reconstruction impact factor journals Anatomic reconstruction Scopus journals Anatomic reconstruction PubMed journals Anatomic reconstruction medical journals Anatomic reconstruction free journals Anatomic reconstruction best journals Anatomic reconstruction top journals Anatomic reconstruction free medical journals Anatomic reconstruction famous journals Anatomic reconstruction Google Scholar indexed journals Body Mass Index articles Body Mass Index Research articles Body Mass Index review articles Body Mass Index PubMed articles Body Mass Index PubMed Central articles Body Mass Index 2023 articles Body Mass Index 2024 articles Body Mass Index Scopus articles Body Mass Index impact factor journals Body Mass Index Scopus journals Body Mass Index PubMed journals Body Mass Index medical journals Body Mass Index free journals Body Mass Index best journals Body Mass Index top journals Body Mass Index free medical journals Body Mass Index famous journals Body Mass Index Google Scholar indexed journals Hamstring tendon articles Hamstring tendon Research articles Hamstring tendon review articles Hamstring tendon PubMed articles Hamstring tendon PubMed Central articles Hamstring tendon 2023 articles Hamstring tendon 2024 articles Hamstring tendon Scopus articles Hamstring tendon impact factor journals Hamstring tendon Scopus journals Hamstring tendon PubMed journals Hamstring tendon medical journals Hamstring tendon free journals Hamstring tendon best journals Hamstring tendon top journals Hamstring tendon free medical journals Hamstring tendon famous journals Hamstring tendon Google Scholar indexed journals Ankle stability articles Ankle stability Research articles Ankle stability review articles Ankle stability PubMed articles Ankle stability PubMed Central articles Ankle stability 2023 articles Ankle stability 2024 articles Ankle stability Scopus articles Ankle stability impact factor journals Ankle stability Scopus journals Ankle stability PubMed journals Ankle stability medical journals Ankle stability free journals Ankle stability best journals Ankle stability top journals Ankle stability free medical journals Ankle stability famous journals Ankle stability Google Scholar indexed journals Bio-absorbable screw articles Bio-absorbable screw Research articles Bio-absorbable screw review articles Bio-absorbable screw PubMed articles Bio-absorbable screw PubMed Central articles Bio-absorbable screw 2023 articles Bio-absorbable screw 2024 articles Bio-absorbable screw Scopus articles Bio-absorbable screw impact factor journals Bio-absorbable screw Scopus journals Bio-absorbable screw PubMed journals Bio-absorbable screw medical journals Bio-absorbable screw free journals Bio-absorbable screw best journals Bio-absorbable screw top journals Bio-absorbable screw free medical journals Bio-absorbable screw famous journals Bio-absorbable screw Google Scholar indexed journals
Article Details
1. Introduction
The Anterior Cruciate Ligament (ACL) is one of the most vital parts for sustaining the knee joint's stability [1]. But, the frequency of ACL injuries is raising alarmingly [2]. Hence, ACL Reconstruction (ACLR) has been known as the most frequently practiced procedure for restoring knee stability [3]. A report claimed that in the United States, each year approximately 200,000 injuries account only for ACL [4]. For ACLR, the widely used reconstruction methods are silver wire, fascia lata, and Iliotibial band [5-7]. There are several techniques available from the open procedure to the arthroscopic procedure [8]. However, the outcomes of ACLR surgery can be influenced by several factors, such as age, sports activities, graft type, initial graft tension, graft diameter, and anatomic reconstruction [9-11]. The diameter of the graft also plays an important role among those factors [12]. There are several anthropometric parameters related to hamstring tendon diameters like height, weight, and Body Mass Index (BMI) of patients [13- 15]. The hamstring tendon is one of the most commonly used grafts for ACLR, but complications like internal rotation strength deficit and sensory deficit were reported in some studies [16,17]. Hence, ideal alternative grafts should be acknowledged for safe and effective ACLR [18-20]. The Peroneus Longus Tendon (PLT) is now considered to be a promising graft which is a safe and efficient alternative to the existing grafting methods [21-23]. PLT is currently used in some orthopedic procedures like deltoid ligament reconstruction and Medial Patellofemoral Ligament (MPFL) reconstruction [24-25]. It has proven to fill the necessary criterion with promising results [26]. There are various requirements for an excellent autograft donor, such as appropriate strength, size, and the convenience and safety of graft harvesting. PLT fulfills the majority of such criteria. Furthermore, PLT is large and strong enough to be used as an autograft in an ACL reconstruction [27]. Additionally, it has no effect on gait and ankle stability when the PLT is removed entirely. Therefore, PLT is thought to be an effective and safe autograft option for ACL reconstruction with respect to its strength, safety, and donor site morbidity [28]. Hence, the aim of this study was to evaluate the stability and the functional outcome of arthroscopic ACL reconstruction by PLT as an effective and safe alternative graft option for ACL reconstruction.
2. Objectives
The objective of this prospective observational study was to evaluate the stability and the functional outcome of arthroscopic ACL reconstruction in nonathletic patients by PLT as an effective and safe alternative graft option for ACL reconstruction.
3. Methods
This prospective study, held between March 2019-January, 2022., observed patients who underwent arthroscopic ACL reconstruction by the same operating surgeon at a tertiary care orthopaedic teaching hospital in the nation's capital. Using consecutive sampling, 78 patients were identified at the emergency and casualty department, 14 were excluded following exclusion criteria, and finally, 64patients were analyzed. Patients were recruited after a comprehensive clinical evaluation to confirm ACL injury. Further, clinical examinations were performed to rule out any injuries to the Posterior Cruciate Ligament (PCL) or the Posterolateral Corner (PLC). Anteroposterior and lateral view radiographs of the afflicted joint were taken, and the case was subsequently confirmed using Magnetic Resonance Imaging (MRI). Inclusion criteria were clinically diagnosed and MRI-confirmed nonathletic patients with only ACL injury and aged between 16 and 45 years. Patients with a pathological condition in the lower extremity and fracture around the knee or associated ligament injury, meniscal injury, chondral damage, and any abnormality of the contralateral knee joint were excluded. Revision cases and patients who refused to provide consent were also excluded. The study was approved by the tertiary care center's Institutional Review Board and informed written consent as per the Declaration of Helsinki was obtained from all the participants. For statistical analysis, SPSS version 20 was used as a statistical tool. The patients have undergone an operation according to the standard protocol of the institution. The PLT and peroneus brevis tendons were identified as dividing through the subcutaneous tissue and superficial fascia. Then to prevent peroneal nerve injury, the PLT was stripped until 5 cm below the fibular head. The donor site was closed, and the graft length was recorded. After this, the ACL repair was done arthroscopically. To simplify the visualization, the intercondylar notch was cleared of fibrous tissue. After implementing the graft with an appropriate tensioner which was protected on the femoral edge of the tunnel by a button and tibial end with a bio-absorbable screw. The patients were observed till 18 months after the surgery.
4. Results
Figure 1 shows the age distribution of the respondents. There were 9(14.1%) respondents who were <18 years and followed by 22(34.4%) were aged between 18-20 and the most 33(51.6%) were >20 years.
Table 1 denotes the baseline characteristics of the respondents. The mean ±SD diameter (mm) was 8.2 ± 0.8, length (mm) was 8.4 ± 0.4, height (cm) was 173.1 ± 8.6, weight (kg) was 75.2 ± 13.2 and BMI was 24.0 ± 3.4.
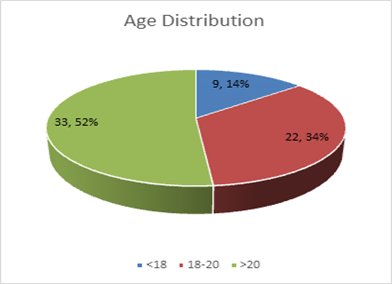
Figure 1: Age Distribution of the Respondents.
|
Baseline Characteristics |
Mean ± SD |
|
Diameter (mm) |
8.2 ± 0.8 |
|
Length (mm) |
8.4 ± 0.4 |
|
Height (cm) |
173.1 ± 8.6 |
|
Weight (kg) |
75.2 ± 13.2 |
|
BMI |
24.0 ± 3.4 |
Table 1: Baseline characteristics of the respondents.
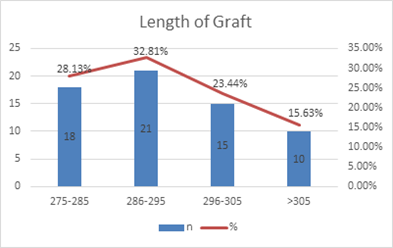
Figure 2: Length of Graft (mm).
Figure 2 describes the length of graft (mm), where 18(28%) patients had grafts of length between 275-285 mm, followed by 21(33%) patients who had grafts between 286-295 mm, 15(23%) between 296-305 mm, and 10(16%) had graph length of >305 mm.
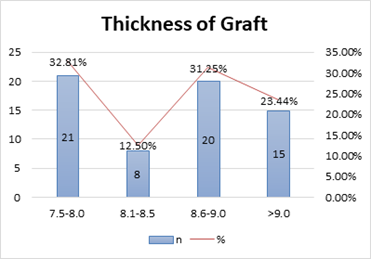
Figure 3: Thickness of graft (mm).
Figure 3 shows the thickness of graft (mm), where the majority of patients (33%) thickness graft ranged between 7.5-8 mm, followed by 8(13%) in between 8.1-8.5 mm, 20(31%) in between 8.6-9 mm and 15(23%) was >9 mm.
|
Time duration from the injury to surgery (months) |
N=64 |
% |
|
Before 1 |
8 |
12.5 |
|
44986 |
32 |
50 |
|
45080 |
16 |
25 |
|
>6 |
8 |
12.5 |
Table 2: Duration of injury before surgery.
Table 2 shows the time duration from the injury to surgery (months) where 8(12.5%) got injured 1 month before the surgery and followed by the most 32(50%) injured before 1-3 months, 16(25%) before 3-6 months and 8(12.5%) before >6 months.
Figure 4 shows the follow-up period at Lachman indicators after the surgery. At the 6-month follow-up, 59(92.2%) of the respondents graded 0 and followed by 5(7.8%) grade I. At 12-months follow up the most 60(93.8%) were graded 0 where 4(6.3%) graded I and at the 18-months follow up, 59(92.2%) graded 0 where 5(7.8%) graded I.
Figure 5 shows the follow-up period at KT-2000 indicators (mm) after the surgery. At the 6-month follow-up, 57(89.1%) of the respondents graded 0-2 mm, followed by 7(10.9%) graded 3-5 mm. At the 12-month follow-up, the majority (92.2%) were graded 0-2 mm, followed by 5(7.8%) graded 3-5 mm at the 18-month follow-up, 57(89.1%) graded 0-2 mm, and followed by 7(10.9%) graded 3-5 mm.
Figure 6 shows that at the final follow-up of 18 months, 92% of participants had a Lachman test score of Grade 0, while 89% of participants had a KT-2000 score between 0-2.
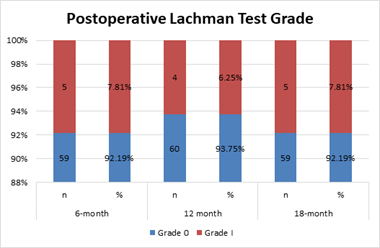
Figure 4: Postoperative Lachman Test.
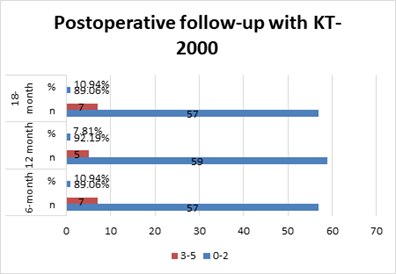
Figure 5: Postoperative KT-2000 measurements.
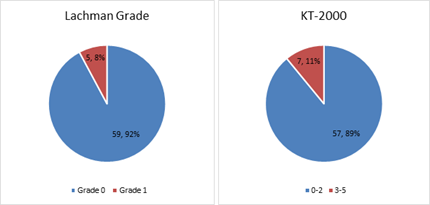
Figure 6: Lachman Grade and KT-2000 scoring at final follow-up at 18 months.
5. Discussion
In the present study, 14.1% of respondents were <18 years of age, followed by 34.4% who were aged between 18- 20, and the majority (51.6%) were >20 years [Figure 1]. In the study of Kumar et al. [29] peroneus longus grafts were used in 15 patients, and semitendinosus was used in 15 patients, with 27.7% and 13.3% from both groups respectively in the age group of <18 years, followed by 20% and 33.3% respectively in the age group of 18-20 years, and 53.3% of both groups participants from the age group >20 years.29 The mean ± SD diameter (mm) was
8.2 ± 0.8, length (mm) was 8.4 ± 0.4, height (cm) was 173.1 ± 8.6, weight (kg) was 75.2 ± 13.2 and BMI was 24.0 ±
3.4 [Table 1]. The study of Song et al. [30] found the mean ± SD diameter (mm) was 8.3 ± 0.8, length (mm) was 8.5
± 0.4, height (cm) was 174.1 ± 8.6, weight (kg) was 76.2 ± 13.2 and BMI was 25.0 ± 3.4.30 28% of participants had graft length between 275-285 mm, followed by the 33% who had between 286-295 mm, 23% in between 296-305 mm and 16% with >305 mm [Figure 2]. Kumar et al. [31] in their study found that 28% of participants had graft lengths between 275-285 mm, followed by the 32% was in between 286-295 mm, 24% in between 296-305 mm and 16% was >305 mm. The majority of the patients' graft thickness ranged between 7.5-8 mm, followed by 13% in between 8.1-8.5 mm, 31% between 8.6-9 mm, and 23% with graft thickness >9 mm [Figure 3]. In a related study, the majority had graft thickness between 7.5-8 mm, followed by 12% in between 8.1-8.5 mm, 32% in between 8.6-9 mm, and 24% was >9 mm. 3112.5% got injured before 1 month to the surgery, followed by half the study population injured before 1-3 months, 25% before 3-6 months and 12.5% before >6 months [Table 2]. The study of Joshi et al.
[32] reported 6% of the respondents got injured 1 month before the surgery, followed by the most 24% injured before 1-3 months, 12% before 3-6 months, and 6% before >6 months [32]. At the 6-month follow-up period at Lachman indicators after the surgery, 92.2% of the respondents graded 0, followed by 7.8% at grade I. At the 12- month follow- up, 93.8% were graded 0, whereas 6.3% were graded I. At the 18-month follow-up, 92.2% graded 0 whereas 7.8% graded I [Figure 4]. Joshi et al. [32] in their study observed that at the 6-month follow-up period at Lachman indicators after the surgery, 91.67% of the respondents were graded 0, followed by 8.37% at grade I. At the 12-month follow- up, 93.75% were graded 0, while 6.25% were graded I, and at the 18-month follow-up, 91.67% were graded 0, and 8.37% were graded I [32]. At the 6-month follow-up period, at KT-2000 indicators (mm) after the surgery, 89.1% of the respondents were graded 0-2 mm, followed by 10.9% who were graded 3-5 mm. At the 12- month follow-up, 92.2% were graded 0-2 mm, followed by 7.8% with a grade of 3-5 mm. At the 18-month follow- up, 89.1% grade 0-2 mm, followed by 10.9% grade 3-5 mm [Figure 5]. Joshi, et al. [32] in their study also reported that at the 6-month follow-up period at KT-2000 indicators (mm) surgery, 89.58% of the respondents graded 0-2 mm, followed by 10.41% grade 3-5 mm. At 12-months followed up the most (91.67%) were graded 0-2 mm and followed by 8.37% graded 3-5 mm and at the 18-month followed up, 89.58% were graded 0-2 mm and followed by 10.41% grade 3-5 mm [32].
6. Conclusion
According to studies, the use of peroneus longus tendon autograft in ACL reconstruction is a safe treatment with a satisfactory outcome, as demonstrated by the Lachman’s test and the IKDC (KT-2000) scores. Peroneus longus tendon may be a viable alternative autograft for ACL restoration. PLT is easy to harvest and takes less time to harvest, has adequate size, a higher ultimate tensile load, more thickness and length, almost no donor site morbidity, and a satisfactory functional outcome and knee stability scores, and after removal, the peroneus longus tendon has no effect on gait parameters and does not cause ankle instability. Furthermore, its excision has no discernible effect on the ankle joint. PLT is an effective and safe autograft option for ACL reconstruction due to all of these characteristics.
References
- Beyzadeoglu T, Akgun U, Tasdelen N, et al. Prediction of semitendinosus and gracilis autograft sizes for ACL reconstruction. Knee Surg Sports Traumatol Arthrosc 20 (2012): 1293-1297.
- Conte EJ, Hyatt AE, Gatt CJJr, et al. Hamstring autograft size can be predicted and is a potential risk factor for anterior cruciate ligament reconstruction failure. Arthroscopy 30 (2014): 882-890.
- Xie G, Huangfu X, Zhao J. Prediction of the graft size of 4-stranded semitendinosus tendon and 4-stranded gracilis tendon for anterior cruciate ligament reconstruction: a Chinese Han patient study. Am J Sports Med 40 (2012): 1161-1166.
- Hootman JM, Dick R, Agel J: Epidemiology of collegiate injuries for 15 sports: summary and recommendations for injury prevention initiatives. J Athl Train 42 (2007): 311-319.
- Gwinn DE, Wilckens JH, McDevitt ER, et The relative incidence of anterior cruciate ligament injury in men and women at the United States Naval Academy. Am J Sports Med 28 (2000): 98-102.
- Vaishya R , Hasija R: Joint hypermobility and anterior cruciate ligament injury . J Orthop Surg (Hong Kong) 21 (2013): 182-184.
- Shultz SJ, Schmitz RJ, Benjaminse A, et al. ACL Research Retreat VI: an update on ACL injury risk and prevention. J Athl Train 47 (2012): 591-603.
- Evans S, Shaginaw J, Bartolozzi ACL reconstruction - it's all about timing . Int J Sports Phys Ther 9 (2014): 268-273.
- Di Benedetto P, Di Benedetto E, Fiocchi A, et Causes of failure of anterior cruciate ligament reconstruction and revision surgical strategies. Knee Surg Relat Res 28 (2016): 319-324.
- Marchand JB, Ruiz N, Coupry A, et Do graft diameter or patient age influence the results of ACL reconstruction? Knee Surg Sports Traumatol Arthrosc 24 (2016): 2998-3004.
- Parkinson B, Robb C, Thomas M, et al. Factors that predict failure in anatomic single-bundle anterior cruciate ligament reconstruction. Am J Sports Med 45 (2017): 1529-1536.
- Magnussen RA, Lawrence JT, West RL, et Graft size and patient age are predictors of early revision after anterior cruciate ligament reconstruction with hamstring autograft. Arthroscopy 28 (2012): 526-531.
- Goyal S, Matias N, Pandey V, et al. Are pre-operative anthropometric parameters helpful in predicting length and thickness of quadrupled hamstring graft for ACL reconstruction in adults? A prospective study and literature Int Orthop 40 (2016): 173-181.
- Gupta R, Malhotra A, Masih GD, et al. Equation-based precise prediction of length of hamstring tendons and quadrupled graft diameter by various anthropometric variables for knee ligament reconstruction in Indian population. J Orthop Surg (Hong Kong) 25 (2017): 23094990-17690997.
- Ho SW, Tan TJ, Lee Role of anthropometric data in the prediction of 4-stranded hamstring graft size in anterior cruciate ligament reconstruction. Acta Orthop Belg 82 (2016): 72-77.
- Hardy A, Casabianca L, Andrieu K, et Complications following harvesting of patellar tendon or hamstring tendon grafts for anterior cruciate ligament reconstruction: systematic review of literature. Orthop Traumatol Surg Res 103 (2017): S245-S248.
- Haviv B, Bronak S, Rath E, et al. Nerve injury during anterior cruciate ligament reconstruction: a comparison between patellar and hamstring tendon grafts harvest. Knee 24 (2017): 564-569.
- Kim W, McQueen P, Watson JN, et al. Anterior cruciate ligament reconstruction with bone-patellar tendon- bone autograft and a medial parapatellar portal. Arthrosc Tech 5 (2016): e827-e831.
- Mohtadi NG, Chan DS, Dainty KN, et al. Patellar tendon versus hamstring tendon autograft for anterior cruciate ligament rupture in adults. Cochrane Database Syst Rev 7 (2011): CD005960.
- Zhao J, Huangfu X. The biomechanical and clinical application of using the anterior half of the peroneus longus tendon as an autograft source. Am J Sports Med 40 (2012): 662-671.
- Cao HB, Liang J, Xin Treatment of anterior cruciate ligament injury with peroneus longus tendon. Zhonghua Yi Xue Za Zhi 92 (2012): 2460-2462.
- Kerimoglu S, Aynaci O, Saracoglu M, et al. Anterior cruciate ligament reconstruction with the peroneus longus tendon. Acta Orthop Traumatol Turc 42 (2008): 38-43.
- Nazem K, Barzegar M, Hosseini A, et Can we use peroneus longus in addition to hamstring tendons for anterior cruciate ligament reconstruction? Adv Biomed Res 3 (2014): 115.
- Wagshul AD, Williams BR, Ellis SJ, et Deltoid ligament reconstruction with peroneus longus autograft in flatfoot deformity. Foot Ankle Int 31 (2010): 781-789.
- Xu C, Zhao J, Xie ScienceDirect Medial patella-femoral ligament reconstruction using the anterior half of the peroneus longus tendon as a combined procedure for recurrent patellar instability. Asia Pac J Sport Med Arthrosc Rehabil Technol 4 (2016): 21-26.
- Nazem K, Barzegar M, Hosseini A, et al. Can we use peroneus longus in addition to hamstring tendons for anterior cruciate ligament reconstruction? Adv Biomed Res 3 (2014): 115.
- Kerimoglu S, Aynaci O, Saraçoglu M, et al. Anterior cruciate ligament reconstruction with the peroneuslongus tendon. Acta Orthop Traumatol Turcica 42 (2008): 38-43.
- Nazem K, Barzegar M, Hosseini A, et al. Can we use peroneus longus in addition to hamstring tendons for anterior cruciate ligament reconstruction? Adv Biomed Res 3 (2014):115.
- Kumar PM, Shevte I, Phalak M, et al. Arthroscopic anterior cruciate ligament reconstruction with semitendinosus graft versus peroneus longus tendon graft. Int J Res Orthop 6 (2020): 386-392.
- Song X, Li Q, Wu Z, et al. Predicting the graft diameter of the peroneus longus tendon for anterior cruciate ligament reconstruction, Medicine 97 (2018): e12672.
- Kumar VK, Narayanan SK, Vishal RB. A study on peroneus longus autograft for anterior cruciate ligament reconstruction. Int J Res Med Sci 8 (2020): 183-188.
- Joshi S, Shetty UC, Salim MD, et al. Peroneus longus tendon autograft for anterior cruciate ligament reconstruction: a safe and effective alternative in nonathletic patients. Niger J Surg 27 (2021): 42-47.
