Perforated Neonatal Appendicitis with Massive Pneumoperitoneum: A Case Report
Article Information
Hysni J. Jashari¹*, Nexhmi Hyseni², Baton Kelmendi3, Fjolla Hyseni4, Ina Kola5, Valon Vokshi6, Barbara Martinez7, Loran Rakovica8, Ali Guy9, Juna Musa10
1Pediatric surgeon. Department of Pediatric Surgery HUCSK-Hospital and University Clinical Service of Kosovo
2Professor of Pediatric Surgery, Chief of Cathedra at Medical Faculty, Department of Pediatric Surgery, University of Pristina HUCSK
3Pediatric surgeon. Department of Pediatric Surgery HUCSK-Hospital and University Clinical Service of Kosovo
4Research Fellow, Department of Urology, NYU Langone Health, New York, USA
5Department of Burns and Plastic Surgery, Tirana, Albania
6Department of Anesthesiology, University Clinical Center Kosovo
7Department of Surgery, Universidad Autonoma de Bucaramanga, Colombia
8Obstetrics and Gynecology Department, General Hospital UK
9Physical Medicine and Rehabilitation, University School of Medicine, NYU, Medical Center, New York, USA
10Department of Surgery Physiology and Biomedical Engineering Mayo Clinic, Rochester, Minnesota
*Corresponding Author: Dr. Hysni J Jashari, Pediatric surgeon, Professor of Pediatric Surgery, Department of Pediatric Surgery HUCSK, Albania
Received: 07 July 2020; Accepted: 21 July 2020; Published: 03 September 2020
Citation: Hysni J. Jashari, Nexhmi Hyseni, Baton Kelmendi, Fjolla Hyseni, Ina Kola, Valon Vokshi, Barbara Martinez, Loran Rakovica, Ali Guy, Juna Musa. Perforated Neonatal Appendicitis with Massive Pneumoperitoneum: A Case Report. Archives of Clinical and Medical Case Reports 4 (2020): 754-759.
View / Download Pdf Share at FacebookAbstract
Neonatal appendicitis (NA) is a rare condition. It has a low incidence of 0.04-0.2% and is more common in premature male babies. NA should be considered in the differential diagnosis in cases when a newborn does not present with clinical signs of Hirschsprung's disease, Cystic Fibrosis and passes meconium normally. The causative etiology of neonatal perforated appendicitis (NPA) is a subject of debate and has not been elucidated. Although many etiologic theories exist, increasing evidence suggests a subset of NPA cases may represent a form of necrotizing enterocolitis (NEC) localized to the appendix. A 6 days old male-baby presented at the NICU with generalized abdominal tenderness, the patient was febrile, with tachycardia and mild respiratory distress. The X-ray showed massive pneumoperitoneum. Intraoperatively, perforated appendix was found and appendectomy was performed. The abdomen was washed with ample saline and closed in layers. Neonatal appendicitis usually presents with non-specific symptoms and signs. Because of its rarity and low index of suspicion, it poses a great diagnostic challenge pre-operatively.
Keywords
Acute Appendicitis; Neonate; Perforation; Pneumoperitoneum
Acute Appendicitis articles, Neonate articles, Perforation articles, Pneumoperitoneum articles
Acute Appendicitis articles Acute Appendicitis Research articles Acute Appendicitis review articles Acute Appendicitis PubMed articles Acute Appendicitis PubMed Central articles Acute Appendicitis 2023 articles Acute Appendicitis 2024 articles Acute Appendicitis Scopus articles Acute Appendicitis impact factor journals Acute Appendicitis Scopus journals Acute Appendicitis PubMed journals Acute Appendicitis medical journals Acute Appendicitis free journals Acute Appendicitis best journals Acute Appendicitis top journals Acute Appendicitis free medical journals Acute Appendicitis famous journals Acute Appendicitis Google Scholar indexed journals Cleft palate articles Cleft palate Research articles Cleft palate review articles Cleft palate PubMed articles Cleft palate PubMed Central articles Cleft palate 2023 articles Cleft palate 2024 articles Cleft palate Scopus articles Cleft palate impact factor journals Cleft palate Scopus journals Cleft palate PubMed journals Cleft palate medical journals Cleft palate free journals Cleft palate best journals Cleft palate top journals Cleft palate free medical journals Cleft palate famous journals Cleft palate Google Scholar indexed journals Neonate articles Neonate Research articles Neonate review articles Neonate PubMed articles Neonate PubMed Central articles Neonate 2023 articles Neonate 2024 articles Neonate Scopus articles Neonate impact factor journals Neonate Scopus journals Neonate PubMed journals Neonate medical journals Neonate free journals Neonate best journals Neonate top journals Neonate free medical journals Neonate famous journals Neonate Google Scholar indexed journals Perforation articles Perforation Research articles Perforation review articles Perforation PubMed articles Perforation PubMed Central articles Perforation 2023 articles Perforation 2024 articles Perforation Scopus articles Perforation impact factor journals Perforation Scopus journals Perforation PubMed journals Perforation medical journals Perforation free journals Perforation best journals Perforation top journals Perforation free medical journals Perforation famous journals Perforation Google Scholar indexed journals Pneumoperitoneum articles Pneumoperitoneum Research articles Pneumoperitoneum review articles Pneumoperitoneum PubMed articles Pneumoperitoneum PubMed Central articles Pneumoperitoneum 2023 articles Pneumoperitoneum 2024 articles Pneumoperitoneum Scopus articles Pneumoperitoneum impact factor journals Pneumoperitoneum Scopus journals Pneumoperitoneum PubMed journals Pneumoperitoneum medical journals Pneumoperitoneum free journals Pneumoperitoneum best journals Pneumoperitoneum top journals Pneumoperitoneum free medical journals Pneumoperitoneum famous journals Pneumoperitoneum Google Scholar indexed journals treatment articles treatment Research articles treatment review articles treatment PubMed articles treatment PubMed Central articles treatment 2023 articles treatment 2024 articles treatment Scopus articles treatment impact factor journals treatment Scopus journals treatment PubMed journals treatment medical journals treatment free journals treatment best journals treatment top journals treatment free medical journals treatment famous journals treatment Google Scholar indexed journals CT articles CT Research articles CT review articles CT PubMed articles CT PubMed Central articles CT 2023 articles CT 2024 articles CT Scopus articles CT impact factor journals CT Scopus journals CT PubMed journals CT medical journals CT free journals CT best journals CT top journals CT free medical journals CT famous journals CT Google Scholar indexed journals surgery articles surgery Research articles surgery review articles surgery PubMed articles surgery PubMed Central articles surgery 2023 articles surgery 2024 articles surgery Scopus articles surgery impact factor journals surgery Scopus journals surgery PubMed journals surgery medical journals surgery free journals surgery best journals surgery top journals surgery free medical journals surgery famous journals surgery Google Scholar indexed journals Neonatal appendicitis articles Neonatal appendicitis Research articles Neonatal appendicitis review articles Neonatal appendicitis PubMed articles Neonatal appendicitis PubMed Central articles Neonatal appendicitis 2023 articles Neonatal appendicitis 2024 articles Neonatal appendicitis Scopus articles Neonatal appendicitis impact factor journals Neonatal appendicitis Scopus journals Neonatal appendicitis PubMed journals Neonatal appendicitis medical journals Neonatal appendicitis free journals Neonatal appendicitis best journals Neonatal appendicitis top journals Neonatal appendicitis free medical journals Neonatal appendicitis famous journals Neonatal appendicitis Google Scholar indexed journals Cystic Fibrosis articles Cystic Fibrosis Research articles Cystic Fibrosis review articles Cystic Fibrosis PubMed articles Cystic Fibrosis PubMed Central articles Cystic Fibrosis 2023 articles Cystic Fibrosis 2024 articles Cystic Fibrosis Scopus articles Cystic Fibrosis impact factor journals Cystic Fibrosis Scopus journals Cystic Fibrosis PubMed journals Cystic Fibrosis medical journals Cystic Fibrosis free journals Cystic Fibrosis best journals Cystic Fibrosis top journals Cystic Fibrosis free medical journals Cystic Fibrosis famous journals Cystic Fibrosis Google Scholar indexed journals
Article Details
1. Introduction
Neonatal Appendicitis (NA) is a rare clinical entity [1]. It accounts for an incidence of 40 per 100,000 live births and is more common in premature male babies [2]. NA presents most of the times with non-specific symptoms and signs, and is usually associated with prematurity or with certain comorbidities including Hirschsprung’s disease, cystic fibrosis, inguinal hernias and cardiopulmonary defects [3]. Most of the time the diagnosis is delayed and is made after perforation has occurred [4]. Neonatal perforated appendicitis (NPA) is uncommon and increasingly being recognized as a localized form of NEC involving the appendix [5]. NA it is a difficult surgical entity to diagnose especially in newborn babies that has passed meconium well and with no signs of Hirschsprung’s disease or Cystic Fibrosis [6]. However, most of the cases of neonatal appendicitis have occurred in preterm neonates, just a few cases have been reported in neonates with no comorbidities and born at term. We present a case of neonatal appendicitis in a 6-day old male born at term with apparently no underlying comorbidity who developed perforated appendicitis, this in order to promote awareness of the high morbidity and mortality that could be avoided by an early diagnosis and appropriate treatment.
2. Case Presentation
A 6-day old full-term male baby was admitted to Neonatal Intensive Care Unit with clinical signs of progressive abdominal distention, irritability and reluctance to feed. Weight at birth was 3.2 kg and had passed meconium within 24 hours of birth. There were no significant perinatal events. Physical examination showed that the boy was lethargic, febrile (38ºC), with tachycardia (146/min) and mild respiratory distress. Abdomen was distended, tense and tender.
Laboratory investigations indicated neutrophilic leukocytosis ((WB count 19.800/mm3, neutrophils 82%). Urine analysis was normal. Ultrasound of the abdomen showed free fluid in the abdominal cavity and the X-ray of the abdomen showed significant pneumoperitoneum (Figure 1). The clinical, laboratory and radiological evaluation suggested the presence of acute abdominal pathology.
The patient got admitted to the Neonatal Intensive Care Unit where he was stabilized with IV fluids and broad-spectrum antibiotics. With a clinical diagnosis of acute abdomen, patient underwent exploratory laparotomy. Intraoperative findings revealed free fluid in the abdominal cavity, perforated appendicitis with a big perforation present at the base of the appendix (Figure 2). During exploration, there were no ischemic patches on the small bowels and the large bowel was of normal caliber, (Figure 3 and Figure 4). Appendectomy was performed and the appendix was sent for histopathological examination. Gentle peritoneal lavage was done and abdomen was closed in layers. 7 days after operation laboratory results revealed normal WBC=7.5/mm3 and PLT=164 × 109/L. The baby subsequently having a smooth and uneventful postoperative recovery. The histopathological report confirmed the gangrenous nature of the removed appendix, with acute inflammatory changes and lymphatic hyperplasia. The outcome was favorable. The patient was on regular follow up for six months and did well.
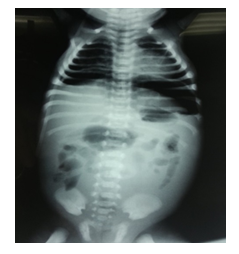
Figure 1: X-ray of abdomen showing dilated bowel loops and abdominal wall edema signifying generalized peritonitis.

Figure 2: The site of perforation of the appendix intraoperative view.

Figure 3: The site of perforation-frontal view.

Figure 4: Intraoperative view, healthy bowls.
3. Discussion
Acute appendicitis is a rare surgical condition in neonates. The incidence of appendicitis in neonates varies from 0.04% to 0.2% and is more common in premature neonates [1, 7]. NA occurs in males approximately 75% of the time and 25 to 50% of all reported cases involve premature babies [8]. The delay in diagnosis and its complications like perforation and septicemia confers a high mortality rate of 28% [9]. Although the clinical signs are nonspecific, the most common findings are abdominal distension, tenderness, feeding intolerance, and fever [10]. Results of laboratory tests have less value for diagnosis in the neonatal period than for older patients [11]. The presentation of neonatal appendicitis can be similar to necrotizing enterocolitis and Hirschsprung’s disease thus leading to misdiagnosis and a significant morbidity and mortality in neonates [12]. Neonatal appendicitis does not appear to have any causal relationship with Hirschsprung’s disease or cystic fibrosis. Although many etiologic theories exist, increasing evidence suggests a subset of NPA cases may represent a form of necrotizing enterocolitis (NEC) localized to the appendix [8]. Association between NA and NEC deserves further investigations because both share the same spectrum of risk factors [13].
The vague clinical features along with low index of suspicion usually result in delay of diagnosis, predisposing to risk of perforation which is reported to be as high as 80% [14]. The perforation could be due to inflammation of the appendix or it could be the results of another disease process for example Hirschsprung's disease, necrotizing enterocolitis, meconium plug syndrome, cystic fibrosis and gastroenteritis. A thin appendicular wall and no distensible caecum predisposes to appendicular perforation in neonatal appendicitis. In neonates, the relatively small size and under developed peritoneal space with lower physiological reserve are possible explanations of the rapid spread of infection. These factors may contribute to high mortality rate due to perforation and peritonitis [15]. Even in the absence of correct clinical diagnosis, perforation - as indicated by pneumoperitoneum - appears to have prompted surgical exploration [16]. Consequently, the prognosis depends on the rapidity between diagnosis and surgical intervention, since the incidence of perforation is high [17].
4. Diagnostic Evaluation and Management
Vital signs and laboratory assessment remain critical components of patient evaluation. Various abdominal radiographs are often the initial imaging study obtained in suspected necrotizing enterocolitis (NEC) but they fail to detect intraperitoneal free air in the setting of NPA [8]. However, according different authors, the presence of free air on plain abdominal radiograph may confer a more favorable prognosis by leading to early surgical intervention [10]. Computed tomography should not be used routinely in neonate due to poor quality and unnecessary radiation. Many authors recommend ultrasonic as the initial image in suspected neonates with appendicitis [18]. Given the rarity of NPA, management is currently driven by anecdotal experience and isolated case reports [19]. Management consists of simple appendectomy and peritoneal lavage with warm saline [20].
5. Conclusion
Although acute appendicitis is the most common surgical condition of childhood, it is seldom evoked in the neonatal period. Neonatologists and pediatric surgeons involved should be alert of variable presentation of this potentially lethal surgical condition, due to anatomical characteristics, inflammation and perforation of the appendix often occur rapidly. We should keep a high level of clinical suspicion, team work and include this entity in differential diagnosis of acute abdominal conditions in neonates, especially in newborns with no clinical signs of Hirschsprung’s disease, Cystic Fibrosis and those that have passed meconium well. A timely diagnosis contributes to a lower morbidity and mortality in newborn period.
References
- Khan RA, Menon P, Rao K. Beware of neonatal appendicitis. J Indian Assoc Pediatr Surg 15 (2010): 67-69.
- Karaman A, Cavusoglu YH, Karaman I, et al. Seven cases of neonatal appendicitis with a review of the English language literature of the last century. Pediatr Surg Int 19 (2003): 707-709.
- Saeki I, Yamanouchi T, Tanaka S, et al. Neonatal appendicitis mimicking intestinal duplication: a case report. J Med Case Rep 6 (2012): 286.
- Haider et al. Perforated acute appendicitis with no peritonitis in a premature baby: a case report. Journal of Medical Case Reports 11 (2017): 125.
- Bax NM, Pearse RG, Dommering N, et al. Perforation of the appendix in the neonatal period. J Pediatr Surg 15 (1980): 200-202.
- Stifle D, Stallmach T, Sachet P. Acute appendicitis in neonates: complication or morgues sui generis? Pediatr Surg Int 14 (1998): 122-123.
- El-Gohary Mohamed Amin, jubouri Salam AL. Neonatal appendicitis with perforation: a case report. J Pediatr Surg Case Rep 2 (2014): 353-354.
- Raveenthiran V. Neonatal appendicitis (part 1): A Review of 52 cases with abdominal manifestation. J Neonatal Surg 4 (2001): 4.
- Karaman A, Cavusoglu YH, Karaman I, et al. Seven cases of neonatal appendicitis with a review of the English language literature of the last century. Pediatr Surg Int 19 (2003): 707-709.
- Schwartz KL, Gilad E, Sigalet D, et al. Neonatal acute appendicitis: a proposed algorithm for timely diagnosis. J Pediatr Surg 46 (2011): 2060-2064.
- Karunakara BP, Ananda Babu MN, Maiya PP, et al. Appendicitis with perforartion in a neonate. Indian J Pediatr 71 (2004): 355-356.
- Jancelewicz T, Kim G, Miniati D. Neonatal appendicitis: a new look at an old zebra.J Pediatr Surg 43 (2008): 1-5.
- Andrew Tumen, Pranit N. Chotai, John Matthew Williams, et al. Neonatal Perforated Appendicitis Attributed to Localized Necrotizing Enterocolitis of the Appendix: J Neonatal Surg 6 (2017): 60.
- Kayastha K. Neonatal perforated appendicitis. J Neonat Surg 1 (2012): 10.
- Sabrinaa JD, Tanb CW, Nallusamy M, et al. Neonatal Perforated Appendicitis. Journal of Pediatric Surgery Case Reports 38 (2018): 66-68.
- Raveenthiran V. Neonatal Appendicitis (Part 1): A Review of 52 cases with Abdominal Manifestation. J Neonatal Surg 4 (2015): 4.
- López-Valdés JC, Escarcega-Servin R. Apendicitis neonatal (AN) en un paciente con enterocolitis necrosante (ECN) secundaria a sepsis in utero. Gac Med Mex 152 (2016): 419-423.
- Howell JM, Eddy OL, Lukens TW, et al. American College of Emergency Physicians. Clinical policy: critical issues in the evaluation and management of emergency department patients with suspected appendicitis. Ann Emerg Med 55 (2010): 71-116.
- Tumen A, et al. Neonatal Perforated Appendicitis Attributed to Localized Necrotizing Enterocolitis of the Appendix: A Review. Journal of Neonatal Surgery 6 (2017): 60.
- Mammou S, Ayadi I, Hamida E, et al. Acute neonatal appendicitis in a preterm. Afr J Paediatr Surg 12 (2015): 294-295.
