Pediatric Non-Functional Retroperitoneal Paragangilioma: A Rare Case Report
Article Information
Abdishakur Mohamed Abdi*, Ismail Haki Gol, Abdullah yusuf Ali
Mogadishu Somali Turkish Training and Research Hospital; Mogadishu, Somalia
*Corresponding Author: Abdishakur Mohamed Abdi, Mogadishu Somali Turkish Training and Research Hospital; Mogadishu, Somalia
Received: 29 December 2021; Accepted: 14 January 2022; Published: 02 June 2022
Citation: Abdishakur Mohamed Abdi, Ismail Haki Gol, Abdullah yusuf Ali. Pediatric Non-Functional Retroperitoneal Paragangilioma: A Rare Case Report. Journal of Cancer Science and Clinical Therapeutics 6 (2022): 234-238.
View / Download Pdf Share at FacebookAbstract
Extra-adrenal paragangiliomas are uncommon neuroendocrine neoplasms with frequency 2-8 per million cases. They have an inclination to be malignant more than pheochromocytomas. Here we present a case of nonfunctional extra adrenal retroperitoneal paraganilioma occurring in 16-year-old male patient presented to with complaints of abdominal pain and heavens on the left hypochondria, CT scan revealed a retroperitoneal gross mass lesion measuring 114 × 99mm in the axial plane, extending from the upper quadrant level of the abdomen towards the inferior and containing necrotic areas in the central part. The mass was surgically removed successfully without intraoperative complications. Postoperative period was uneventful and patient discharged on day 7. Careful preoperative preparation and planning is mandatory as nature of tumor is endocrine tumor which secrete certain hormones and sudden rise or fall serum level of those hormones can result life threatening hypertension or hypotension. Full precaution must be taken to avoid these severe complications.
Keywords
Pediatric; Retroperitoneal; Paragangilioma; Neuroendocrine; Neoplasms
Case Report articles
Pediatric articles Pediatric Research articles Pediatric review articles Pediatric PubMed articles Pediatric PubMed Central articles Pediatric 2023 articles Pediatric 2024 articles Pediatric Scopus articles Pediatric impact factor journals Pediatric Scopus journals Pediatric PubMed journals Pediatric medical journals Pediatric free journals Pediatric best journals Pediatric top journals Pediatric free medical journals Pediatric famous journals Pediatric Google Scholar indexed journals Retroperitoneal articles Retroperitoneal Research articles Retroperitoneal review articles Retroperitoneal PubMed articles Retroperitoneal PubMed Central articles Retroperitoneal 2023 articles Retroperitoneal 2024 articles Retroperitoneal Scopus articles Retroperitoneal impact factor journals Retroperitoneal Scopus journals Retroperitoneal PubMed journals Retroperitoneal medical journals Retroperitoneal free journals Retroperitoneal best journals Retroperitoneal top journals Retroperitoneal free medical journals Retroperitoneal famous journals Retroperitoneal Google Scholar indexed journals Paragangilioma articles Paragangilioma Research articles Paragangilioma review articles Paragangilioma PubMed articles Paragangilioma PubMed Central articles Paragangilioma 2023 articles Paragangilioma 2024 articles Paragangilioma Scopus articles Paragangilioma impact factor journals Paragangilioma Scopus journals Paragangilioma PubMed journals Paragangilioma medical journals Paragangilioma free journals Paragangilioma best journals Paragangilioma top journals Paragangilioma free medical journals Paragangilioma famous journals Paragangilioma Google Scholar indexed journals Neuroendocrine articles Neuroendocrine Research articles Neuroendocrine review articles Neuroendocrine PubMed articles Neuroendocrine PubMed Central articles Neuroendocrine 2023 articles Neuroendocrine 2024 articles Neuroendocrine Scopus articles Neuroendocrine impact factor journals Neuroendocrine Scopus journals Neuroendocrine PubMed journals Neuroendocrine medical journals Neuroendocrine free journals Neuroendocrine best journals Neuroendocrine top journals Neuroendocrine free medical journals Neuroendocrine famous journals Neuroendocrine Google Scholar indexed journals Neoplasms articles Neoplasms Research articles Neoplasms review articles Neoplasms PubMed articles Neoplasms PubMed Central articles Neoplasms 2023 articles Neoplasms 2024 articles Neoplasms Scopus articles Neoplasms impact factor journals Neoplasms Scopus journals Neoplasms PubMed journals Neoplasms medical journals Neoplasms free journals Neoplasms best journals Neoplasms top journals Neoplasms free medical journals Neoplasms famous journals Neoplasms Google Scholar indexed journals chromaffin cells articles chromaffin cells Research articles chromaffin cells review articles chromaffin cells PubMed articles chromaffin cells PubMed Central articles chromaffin cells 2023 articles chromaffin cells 2024 articles chromaffin cells Scopus articles chromaffin cells impact factor journals chromaffin cells Scopus journals chromaffin cells PubMed journals chromaffin cells medical journals chromaffin cells free journals chromaffin cells best journals chromaffin cells top journals chromaffin cells free medical journals chromaffin cells famous journals chromaffin cells Google Scholar indexed journals adrenal retroperitoneal paraganilioma articles adrenal retroperitoneal paraganilioma Research articles adrenal retroperitoneal paraganilioma review articles adrenal retroperitoneal paraganilioma PubMed articles adrenal retroperitoneal paraganilioma PubMed Central articles adrenal retroperitoneal paraganilioma 2023 articles adrenal retroperitoneal paraganilioma 2024 articles adrenal retroperitoneal paraganilioma Scopus articles adrenal retroperitoneal paraganilioma impact factor journals adrenal retroperitoneal paraganilioma Scopus journals adrenal retroperitoneal paraganilioma PubMed journals adrenal retroperitoneal paraganilioma medical journals adrenal retroperitoneal paraganilioma free journals adrenal retroperitoneal paraganilioma best journals adrenal retroperitoneal paraganilioma top journals adrenal retroperitoneal paraganilioma free medical journals adrenal retroperitoneal paraganilioma famous journals adrenal retroperitoneal paraganilioma Google Scholar indexed journals hypochondria articles hypochondria Research articles hypochondria review articles hypochondria PubMed articles hypochondria PubMed Central articles hypochondria 2023 articles hypochondria 2024 articles hypochondria Scopus articles hypochondria impact factor journals hypochondria Scopus journals hypochondria PubMed journals hypochondria medical journals hypochondria free journals hypochondria best journals hypochondria top journals hypochondria free medical journals hypochondria famous journals hypochondria Google Scholar indexed journals intraoperative complications articles intraoperative complications Research articles intraoperative complications review articles intraoperative complications PubMed articles intraoperative complications PubMed Central articles intraoperative complications 2023 articles intraoperative complications 2024 articles intraoperative complications Scopus articles intraoperative complications impact factor journals intraoperative complications Scopus journals intraoperative complications PubMed journals intraoperative complications medical journals intraoperative complications free journals intraoperative complications best journals intraoperative complications top journals intraoperative complications free medical journals intraoperative complications famous journals intraoperative complications Google Scholar indexed journals pheochromocytomas articles pheochromocytomas Research articles pheochromocytomas review articles pheochromocytomas PubMed articles pheochromocytomas PubMed Central articles pheochromocytomas 2023 articles pheochromocytomas 2024 articles pheochromocytomas Scopus articles pheochromocytomas impact factor journals pheochromocytomas Scopus journals pheochromocytomas PubMed journals pheochromocytomas medical journals pheochromocytomas free journals pheochromocytomas best journals pheochromocytomas top journals pheochromocytomas free medical journals pheochromocytomas famous journals pheochromocytomas Google Scholar indexed journals
Article Details
1. Introduction
Extra-adrenal paragangiliomas are uncommon neuroendocrine neoplasms with frequency 2-8 per million cases [1]. They emerge from neural peak cells and are composed of primarily of chromaffin cells found within the Para aortic sympathetic chain, they synthesize, store and discharge catecholamine’s [1]. Patient may present with headache, diaphoresis and palpitation and high blood pressure. On the other hand they may remain unnoticed, nonfunctional or nonspecific symptoms such as abdominal pain due to periodic release of catecholamine’s. Wen J, et al. Reported that histologically and immunochemically no difference between silent and functional tumors [2]. Essential strategies of preoperative determination include incorporate imaging procedures which guides surgical arranging and preoperative planning. Silent tumors often failed to detect preoperatively and present complications intraoperative. In 95% of the cases of extra-adrenal paragangiliomas are located within the abdominal regions, but they will also occur within the head, neck and thoracic regions. McNicol AM. Reported that extra-adrenal paragangiliomas have an inclination to be malignant more than pheochromocytomas [3]. There are few case reports regarding non-functional extra-adrenal paragangiliomas; the literature is scarce for the early diagnosis and optimal preoperative and intraoperative management. This case report is aimed to highlight the clinical presenatation, diagnosis and treatment outcomes of a case of non-functional extra-adrenal retroperitoneal paraganilioma in 16-years male patient successfully managed with complete surgical resection.
2. Case Report
A 16-year-old male patient presented to pediatric surgery department with complaints of abdominal pain and heavens on the left hypochondria. There was no history of vomiting or altered bowel habits or previous history of similar attacks. The patient was not a known hypertensive and was not on any medication. Per abdominal examination revealed tenderness and a mass in the left hypochondriac region which did not move with respiration. Bowel sounds and rectal examination were normal, contrast ct scan revealed a retroperitoneal gross mass lesion measuring 114 × 99mm in the axial plane, extending from the upper quadrant level of the abdomen towards the inferior and containing necrotic areas in the central part, mass lesion extends to the mid abdomen, there is no calcification in it. There is heterogeneous contrast enhancement in post contrast images. The lesion is hypervascular Figure 1. Laboratory profiles were normal. Transverse left subcostal incision was undertaken for exploration. a retroperitoneal mass was found inferior to the renal vein on the left side of aorta occupying 2nd, 3rd and 4th lumbar vertebral levels. The tumour was adjacent tp the aorta. The ureter was pushed anteriorly while the inferior mesenteric vessels were pushed laterally. There was abundant direct vascular connection from aorta supplying the mass. The mass was found located ventral to the sympathetic and lymphatic chain. During dissection of the mass several veins brusted and ligated. With careful dissection the mass was completely resected (Figure 2).
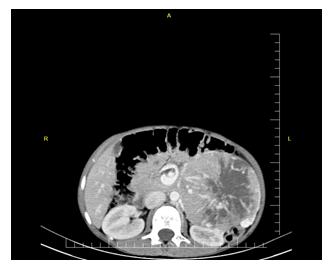
Figure 1: Gross mass lesion measuring 114 × 99mm in the axial plane, with central necrosis.
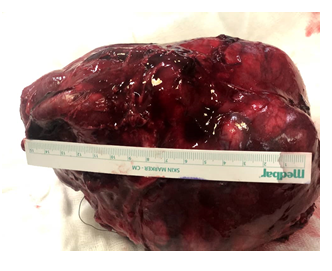
Figure 2: Completely resected paragangilioma.
Histopathological Findings
Gross examination
Consistent cut surface prefer grey white centrally pinkish soft with focal myxoid hemorrhagic changes.
Microscopy
Procedure: Borderline resection
Tumor Site: Retro peritoneum
Tumor Size: 13x10x7 cm
Histologic Type: Paraganglioma
Mitotic Rate: 3/10 HPF
Necrosis: Present (<5%)
Histologic Grade: Intermediate Behavior
Margins: All margins negative for tumor but borderline appearance.
Lymphovascular Invasion: Not identified
Histopathologic diagnosis: retroperitoneal paragangilioma, intermittent behavior.
3. Discussion
Paragangiliomas can develop anywhere along the midline of the retro peritoneum. The precise incidence of retroperitoneal paragangiliomas is unknown, although male are typically affected more than females. Additionally most patients are diagnosed between 30 and 45 years old Masahiro Shibata. Reported A 24-year-old female presented to the regional hospital with complaints of hyperhidrosis and hypertension [4]. In the current case we report a case of non-functional extra-adrenal retroperitoneal paraganilioma in a 16-years male patient successfully managed with complete surgical resection. Clinically, patients with retroperitoneal paragangilioms often present with back pain or palpable mass. Conventional treatment for paragangiliomas typically involves complete surgical excision, while surgical debunking is taken into account as mainstay of palliative therapy for malignant paragangiliomas [2]. In some cases complete excision is sometimes not feasible due to highly vascular characteristics of the paragangiliomas and their closeness to the major blood vessels. Abdominal paragangiliomas are mostly located in the retro peritoneum, overall 85% of the extra-adrenal paragangiliomas. The foremost common site of retroperitoneal paragangiliomas occurs between origin of inferior mesenteric c artery and aortic bifurcation and it is known as organ of zuckerkandl. paragangilioma originating from the jugulotympanic body are called chemodectomas While paragangilioma arising from chemoreceptor are referred to as chemoreceptor tumors. Paragangiliomas residing in the second part of the duodenum are called gangiliocytic paragangilioma [5]. functional paragangiliomas are diagnosed by its clinical presentation and laboratory results showing raised level of catecholamine’s and their byproduct within the urine and blood whereas nonfunctional paragangiliomas are commonly found incidentally or present as mass with compression symptoms of the organ it compresses [6].
4. Conclusion
Extra adrenal retroperitoneal paragangiliomas are uncommon neoplasms which pause difficult in diagnosis and treatment. However careful preoperative preparation and planning is mandatory as nature of tumor is endocrine tumor which secretes certain hormones and sudden rise or fall serum level of those hormones can result life threatening hypertension or hypotension. Full precaution must be taken to avoid these severe complications.
References
- Nancy Perrier, Alexandria Phan, Steven Waguespack, et al. Clinical Benefits of Systemic Chemotherapy for Patients with Metastatic Pheochromocytomas or Sympathetic Extra-Adrenal Paragangliomas. Cancer 1 (2012): 2805.
- Wen J, Li HZ, Ji ZG, et al. A decade of clinical experience with extra-adrenal paragangliomas of retroperitoneum: Report of 67 cases and a literature review. Urology annals 2 (2010): 12.
- McNicol AM. Update on tumours of the adrenal cortex, phaeochromocytoma and extra?adrenal paraganglioma. Histopathology 58 (2011): 155-168.
- Shibata M, Inaishi T, Miyajima N, et al. Synchronous bilateral pheochromocytomas and paraganglioma with novel germline mutation in MAX: a case report. Surgical case reports 3 (2017): 1-5.
- Mete O, Tischler AS, De Krijger R, et al. Protocol for the examination of specimens from patients with pheochromocytomas and extra-adrenal paragangliomas. Archives of Pathology and Laboratory Medicine 138 (2014): 182-188.
- Tischler AS, Pacak K, Eisenhofer G. The adrenal medulla and extra-adrenal paraganglia: then and now. Endocrine pathology 25 (2014): 49-58.
